Stroke recurrence is an important issue in stroke registries, but direct patient contact months after stroke is not always feasible. Telephone assessment is often used to evaluate long term stroke outcome, treatments and recurrences. Our aim is to evaluate telephone interview in a stroke registry.
Material and methodsThree hundred and eighty patients with a stroke or TIA were prospectively registered, evaluating baseline characteristics and type of event. At 6 months, 248 patients were reviewed by structured telephone interview and 132 were reviewed by direct contact. We analysed stroke outcome and disability, treatments and stroke or TIA recurrences.
ResultsThere were no differences in baseline characteristics and type or severity of the index event. At 6 months, treatments were similar between both groups and 10.5% (40 patients) had a recurrent event. There were no differences in recurrent ischemic strokes (6.1% in direct contact vs 4.4% telephone, P=.49), but we detected a higher number of TIA in direct examination compared to phone interview (9.1% vs 4.0%, P=.04).
ConclusionsTelephone assessment of stroke patients is reliable and facilitates stroke registries in detecting long-term treatments and stroke recurrences. However, it is probable that new transient events or TIA are under-estimated.
La recurrencia de ictus o AIT es un aspecto clave en la mayoría de los registros de ictus, pero la revisión presencial de todos los pacientes no siempre es viable. Con frecuencia, la revisión telefónica es utilizada para evaluar las recurrencias, la situación funcional y los tratamientos a largo plazo. El objetivo es evaluar la revisión telefónica en un registro de ictus.
Material y métodosSe registraron prospectivamente 380 pacientes con ictus o AIT valorando las características basales y tipo de evento. Posteriormente, fueron evaluados a los 6 meses tras el evento inicial. Doscientos cuarenta y ocho pacientes fueron revisados telefónicamente mediante una entrevista estructurada y 132 fueron revisados físicamente en consulta. Se compararon ambos grupos analizando las diferencias detectadas en las escalas funcionales, tratamientos y recurrencias (AIT o ictus).
ResultadosNo hubo diferencias en las características basales de ambos grupos, ni en el tipo de evento o gravedad al inicio. A los 6 meses, los tratamientos realizados fueron similares en ambos grupos, presentando un 10,5% (40 pacientes) recurrencia de ictus o AIT. No hubo diferencias significativas en la tasa de nuevos ictus isquémicos (6,1% revisión física vs 4,4% telefónica, p=0,49), pero se detectó un mayor número de AIT en la revisión física frente a la telefónica (9,1% vs 4,0%, p=0,04).
ConclusionesLa revisión telefónica de los pacientes con ictus es viable y facilita la realización de registros de ictus, permitiendo una adecuada identificación de los tratamientos y recurrencias de ictus. Sin embargo, es probable que los nuevos eventos transitorios o AIT estén infraestimados.
Recurrence after a stroke is a key element in the study of cerebrovascular disease and provides information on the effectiveness of secondary prevention measures adopted after the event. Factors that influence recurrence include advanced age, diabetes mellitus and hemorrhagic stroke, with the estimated risk of recurrent stroke being close to 22.5% in the first 5 years,1 although it is more common in the first 6 months (8%–10%).2
Given the importance and frequency of stroke recurrence, it is important to record it systematically. However, hospital stroke records often assess recurrence retrospectively or based on readmission of a patient at the same centre. This is due to the fact that conducting reviews through direct contact months after a stroke is not always feasible and may determine a selection of the patients reviewed.
Reviews conducted by telephone through structured interviews can simplify the long-term evaluation of patients after stroke and potentially reduce its costs. Although reviews by telephone have been used in the assessment of functional status and even cognitive status of patients,3,4 there are few prospective studies that examine the telephonic review as a method of evaluating recurrence after a stroke.
The aim of this study was to determine the feasibility of telephonic review of patients after a stroke, in the context of hospital stroke records, assessing the detection of recurrent stroke or transient ischemic attacks (TIAs) and functional status at 6 months from the event.
Material and methodsWe performed a prospective study, recording 380 consecutive cases of ischemic stroke, hemorrhagic stroke or TIA treated at the emergency department of a tertiary hospital. We evaluated baseline demographic data such as gender, age and vascular risk factors, as well as any treatments followed prior to the stroke. The initial severity of the event was assessed using the Canadian scale (Canadian Stroke Scale) upon arrival of the patient at the emergency department; in those cases in which an evaluation according to this scale was not available, we estimated according to the initial neurological examination.
For the diagnosis of TIA, we used the criteria of the World Health Organisation (WHO), which define it as the presence of focal neurological symptoms of vascular origin and sudden onset, and with a duration of less than 24h.
Patients were reviewed by a neurologist experienced in stroke at 6 months after the event. Patients were divided into 2 groups, personal review and telephonic review. Consecutively, the first 248 patients included were reviewed using a structured interview by telephone and the following 132 patients were reviewed in person. In both cases there were recurrences of both TIA and new established, ischemic or hemorrhagic events. These were assessed by patient interview as well as by review of emergency admissions and hospital admissions recorded during that period. Furthermore, we evaluated treatment with antithrombotic agents and for the control of vascular risk factors at the time of the review and the functional status of the patient using the modified Rankin scale and Barthel index. In those cases where it was not possible to conduct a review at the hospital due to distance or disability, it was conducted by telephone.
Subsequently, we compared the baseline characteristics of patients according to the type of review and the data corresponding to recurrences, treatment followed and functional status of patients at 6 months. The qualitative variables according to study groups (telephone or physical review) were analysed using the chi-square test or Fisher's exact test when necessary and were expressed as absolute and relative frequencies. Quantitative variables were analysed using the Mann–Whitney U test, since they did not follow a normal distribution, and were expressed as medians (interquartile range).
This study was approved by the local ethics committee and patients signed an informed consent form prior to inclusion.
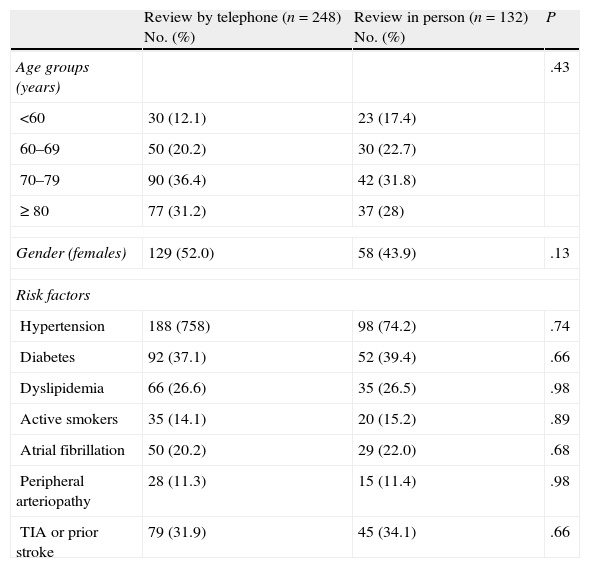
ResultsOf the total of 380 registered patients, 248 (65.3%) were reviewed by telephone and 132 (34.7%) were assessed in person during hospital consultation. A total of 13 patients who had been assigned to personal review could not attend due to disability or distance and were reviewed by telephone. When comparing the 2 types of reviews, we did not detect significant differences by age group. We found a high percentage of patients above 80 years of age in both groups (31% of those reviewed by telephone vs 28% reviewed in person, P=.46). As for gender, no differences were found between both groups, with 49.2% of patients being females (Table 1).
Demographic data.
| Review by telephone (n=248) No. (%) | Review in person (n=132) No. (%) | P | |
| Age groups (years) | .43 | ||
| <60 | 30 (12.1) | 23 (17.4) | |
| 60–69 | 50 (20.2) | 30 (22.7) | |
| 70–79 | 90 (36.4) | 42 (31.8) | |
| ≥ 80 | 77 (31.2) | 37 (28) | |
| Gender (females) | 129 (52.0) | 58 (43.9) | .13 |
| Risk factors | |||
| Hypertension | 188 (758) | 98 (74.2) | .74 |
| Diabetes | 92 (37.1) | 52 (39.4) | .66 |
| Dyslipidemia | 66 (26.6) | 35 (26.5) | .98 |
| Active smokers | 35 (14.1) | 20 (15.2) | .89 |
| Atrial fibrillation | 50 (20.2) | 29 (22.0) | .68 |
| Peripheral arteriopathy | 28 (11.3) | 15 (11.4) | .98 |
| TIA or prior stroke | 79 (31.9) | 45 (34.1) | .66 |
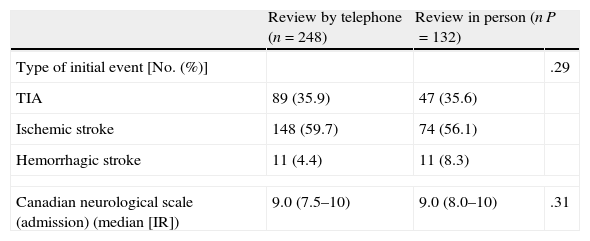
The types of initial vascular events were distributed similarly amongst both groups (Table 2), with no significant differences being found. Ischemic stroke accounted for 58% (59% in telephonic reviews and 56% in personal reviews), TIA for 36% (36% in both groups) and hemorrhagic stroke for 5.8% (5% and 8% respectively). The severity of the initial stroke on arrival at the emergency service, as assessed through the Canadian Stroke Scale, was also comparable between patients from both types of review (median=9 [7.5–10] of telephone reviews vs 9 [8.0–10] of personal reviews, P=.31).
Type of initial event.
| Review by telephone (n=248) | Review in person (n=132) | P | |
| Type of initial event [No. (%)] | .29 | ||
| TIA | 89 (35.9) | 47 (35.6) | |
| Ischemic stroke | 148 (59.7) | 74 (56.1) | |
| Hemorrhagic stroke | 11 (4.4) | 11 (8.3) | |
| Canadian neurological scale (admission) (median [IR]) | 9.0 (7.5–10) | 9.0 (8.0–10) | .31 |
IR: interquartile range.
An evaluation of the baseline presence of vascular risk factors in the patients reviewed in person and by telephone revealed no significant differences between both groups (Table 1). Up to 75% of patients presented a history of hypertension (75.8% reviewed by telephone vs 74.2% reviewed in person), 38% were diabetic (37% vs 39%) and 27% in both groups suffered dyslipidemia. Up to 14.5% were active smokers and 12.1% were former smokers. Only 11.3% presented known peripheral arterial disease and 21% presented atrial fibrillation. Up to one third of patients in both groups had suffered a previous episode of stroke or TIA (32% reviewed by telephone vs 34% reviewed in person, P=.66). After the initial event, 92.6% of patients were discharged from the hospital with antithrombotic therapy, with no differences between both groups. The majority (73.2%) were treated with antihypertensive agents, 35.3% were treated for diabetes and 31.8% were treated with statins, with no significant differences between both groups.
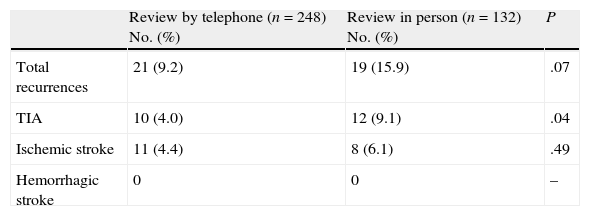
At 6 months, 10.5% of the total (40 patients) suffered recurrence of a cerebrovascular event (Table 3). We detected a trend towards higher detection rates of recurrent events in the group of patients reviewed in person than in those reviewed by telephone (15.9% vs 9.2%, P=.07). When assessing the type of recurrence detected, 19 patients of the total (5%) presented a recurrent ischemic stroke, with a similar frequency in both groups (4.4% in those reviewed by telephone compared to 6.1% in those reviewed in person, P=.5). However, when evaluating the cases of TIA detected, we noted a significant increase in diagnoses among patients reviewed in person compared to those reviewed by telephone (9.1% vs 4.0%, P=.04). There were no recurrences of hemorrhagic stroke at 6 months.
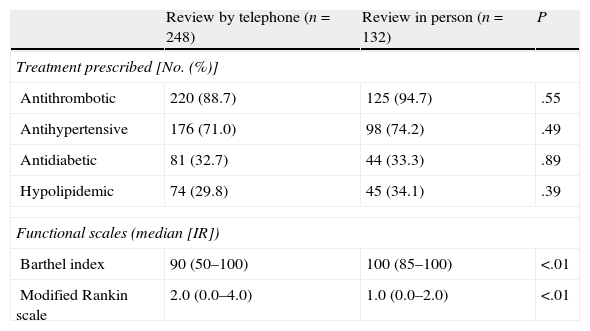
Regarding the treatment performed at the time of the review, 90% of patients continued with antithrombotic medication, with this percentage being slightly higher among patients reviewed in person (89% in patients reviewed by telephone vs 94% in patients reviewed in person, P=.06). Of these, 18% followed oral anticoagulation (18.8% vs 17.4%, P=.58). No significant differences were found between both groups regarding antihypertensive, antidiabetic or hypolipidemic treatment. Finally, we evaluated the functional scales and found a greater degree of disability according to the modified Rankin scale and Barthel index in the group of patients reviewed by telephone compared to those reviewed in person (median: 2.0 vs 1.0, P<.01; 90 vs 100, P<.01, respectively) (Table 4).
Treatments prescribed at 6 months and functional scales.
| Review by telephone (n=248) | Review in person (n=132) | P | |
| Treatment prescribed [No. (%)] | |||
| Antithrombotic | 220 (88.7) | 125 (94.7) | .55 |
| Antihypertensive | 176 (71.0) | 98 (74.2) | .49 |
| Antidiabetic | 81 (32.7) | 44 (33.3) | .89 |
| Hypolipidemic | 74 (29.8) | 45 (34.1) | .39 |
| Functional scales (median [IR]) | |||
| Barthel index | 90 (50–100) | 100 (85–100) | <.01 |
| Modified Rankin scale | 2.0 (0.0–4.0) | 1.0 (0.0–2.0) | <.01 |
IR: interquartile range.
Stroke is a major cause of mortality in the world and, in Spain, as in other countries, it is a health priority. Although the mortality rate has steadily decreased in recent years, stroke causes chronic disability in many patients and represents a major social and healthcare cost. For this reason, it is important to keep records of stroke patients at those centres offering care for this pathology, to assess short-, medium- and long-term morbidity and mortality in clinical practice, as well as recurrences. Although the possibility of stroke recurrence is maintained in the long term, it is much more common within the first 6–12 months after the initial event, reaching figures of up to 9% and 13%–14%, respectively.1 This higher initial recurrence is particularly relevant in TIA, since rates of occurrence of stroke after TIA of nearly 10% in the first 90 days have been described.5,6 Therefore, stroke records typically include reviews at 6 months or 1 year after the initial event, in order to establish the functional status of the patient and also to detect new vascular events. However, given the high incidence of cerebrovascular disease, direct contact and review of all patients in person is not always feasible and represents a challenge for the maintenance of records.
Telephone assessment of stroke patients has frequently been used in clinical trials and stroke registries,7–9 as it simplifies the design of studies, reduces costs and potentially avoids investigator bias derived from the knowledge of clinical data, especially in the assessment of functional scales. There are several studies comparing the validity of the assessment of functional scales such as the Barthel index and the modified Rankin scale through reviews conducted by telephone compared to physical or in-person examination of stroke patients.10,11 Newcommon et al.10 found excellent agreement between observers in the assessment of the Rankin scale in reviews conducted in person (K=0.72), but with much greater variability when the review was conducted by telephone (K=0.3). However, the use of a structured interview for the application of functional scales manages to reduce interobserver variability and improves the quality of the studies.12 It has recently been proven that the use of structured interviews is also useful during telephone reviews, optimising agreement between observers.13
Telephone interviews have been used not only to assess the functional patient status after stroke, but also to study the presence of cognitive impairment.4 However, there are few studies in the literature evaluating the use of telephonic reviews of the clinical outcome of stroke and the onset of recurrences. Using a telephonic survey conducted by an experienced researcher, Meschia et al.14 found high reliability in the detection of patients without stroke or TIA, but with less specificity in the diagnosis of new strokes or TIAs compared to those reviewed in person.
In the present study, after reviewing 380 patients at 6 months after a cerebrovascular event, we detected 10.5% of recurrences of new strokes or TIAs. Despite studying 2 samples with equal baseline characteristics, when comparing the 2 types of reviews, detection of recurrences was more frequent in personal reviews than in telephonic reviews. Although the rate of new ischemic strokes was similar in both groups and equivalent to that described previously in the literature,1,2,15 TIAs were diagnosed significantly more often during direct contact with patients (9.1% vs 4.0%). This may be because telephonic interviews are conducted in a shorter time than personal interviews, usually in a few minutes,14 so the detection of minor events such as TIA can be difficult. In addition, while telephonic interviews are usually conducted with a single person (the patient or a relative), personal reviews are conducted more in depth with both patients and companions, which facilitates the detection of any type of event. This is especially relevant when considering the high frequency of patients with neurological deficit of less than 24h duration diagnosed with TIA, who present an ischemic lesion identified by neuroimaging (up to 50% of patients),16 and which are actually established ischemic strokes. This has even led to a recent change in the traditional definition of TIA.17
Despite the difference in the recurrence of new events, the treatments for both groups at the time of the review were very similar. Neither antithrombotic therapy nor that of vascular risk factors differed significantly in both samples.
The evaluation of functional scales showed a greater dependence of patients reviewed by telephone. This is probably justified by the fact that patients who were interviewed by telephone were those for whom it was not possible to attend a physical examination in the hospital due to their functional status. This could represent a limitation, as a greater number of events might be expected in telephonic reviews. Nevertheless, this study detected more events in the group reviewed in person, which does not justify a greater disability in the group reviewed by telephone. On the other hand, this is one of the advantages of telephonic reviews since, while making it possible to maintain stroke records and evaluation of new events, they avoid movement of patients that would otherwise be very difficult.
Consequently, the telephonic review of stroke patients is a viable method that facilitates the completion of stroke records and the assessment of treatments and recurrences. However, detection of new transient events or TIAs is probably underestimated in this type of review.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Moniche F, et al. Evaluación de la revisión telefónica en la recurrencia de ictus y AIT. Neurología. 2011;27:97–102.