Hallucinations are frequent in clinical practice, with an incidence of up to 38.7% in the general population. We aim to determine the prevalence of hallucinations among healthy young adults in our environment.
Subjects and methodsWe designed an observational study, using as subjects, third to sixth year medical students of the Universidad Complutense de Madrid who complete clinical rotations in the Hospital Clínico San Carlos. After a screening questionnaire, an individual interview was conducted via telephone or e-mail for those students who reported hallucinations. We obtained clinical and epidemiological data through a semi-structured clinical interview performed by a third year neurology resident.
ResultsN=134 (average age was 22.1 years; 77.6% were women). 74 respondents answered affirmatively to one or more screening questions, and 54 completed the follow-up interview. 22.2% described visual phenomena and 64.8%, auditory. The majority reported sleep-related experiences and auditory perceptions related to hyper vigilance, such as hearing the telephone or the doorbell ring when in fact it had not (38.8%). All subjects had good insight and none had psychotic symptoms. Two cases were associated with substance abuse.
ConclusionsHallucinations are frequent among the general population. Traditionally, auditory phenomena have been associated with psychotic pathology, and other studies show a low population incidence (0.6%). However, in our sample, short auditory perceptions with immediate insight were frequent and not pathological.
Las alucinaciones son frecuentes en la práctica clínica y presentan una incidencia poblacional de hasta el 38.7%. El objetivo del estudio es determinar la prevalencia de percepciones aberrantes entre jóvenes sanos de nuestro entorno.
Sujetos y MétodosEstudio observacional entre estudiantes de 3.° a 6.° curso de Medicina de la Universidad Complutense de Madrid que realizan prácticas en el Hospital Clínico San Carlos. Tras una encuesta de cribado, se realizó una entrevista individual a aquellos sujetos que presentaban percepciones aberrantes. Recogimos datos epidemiológicos mediante anamnesis semi-estructurada administrada por una residente de tercer año de Neurología.
ResultadosN=134 (edad media 22.1 años, 77.6% mujeres). 74 respondedores contestaron afirmativamente a alguna de las preguntas de screening y 54 completaron la entrevista. El 22.2% presentó fenómenos visuales y el 64.8% auditivos. La mayoría describieron fenómenos asociados al sueño y percepciones auditivas como oír el teléfono o el timbre de la puerta sin que hubieran sonado (38.8%). Todos presentaron crítica de los episodios y ninguno refirió síntomas psicóticos. Dos casos se asociaron a tóxicos.
ConclusionesLas percepciones aberrantes son muy frecuentes entre la población general. Clásicamente, se asocian los fenómenos auditivos a patología psicótica, y otros estudios dan una incidencia poblacional baja (0.6%). Sin embargo, en nuestra serie las percepciones auditivas de corta duración y con crítica inmediata eran frecuentes y no se asociaban a patología.
The American Psychiatric Association1 defines hallucination as a perception that has the compelling sense of reality of a true perception but that occurs without external stimulation of the relevant sensory organ. They may affect any of the senses, or various sensory modalities at once in the case of complex hallucinations.
Aberrant perceptions should be considered a symptom and not a disease. They do not affect sick people exclusively, nor do they always indicate illness.2 According to epidemiological studies, incidence in the general population ranges from 3% to 38.7%.3,4 These discrepancies are probably due to differences in methodology. The hypothesis which has persisted for many years is that the spectrum of hallucinatory predisposition in the general population ranges from psychotic patients to healthy subjects with no hallucinations. This spectrum includes a percentage between 10% and 15% with aberrant perceptions and no other symptoms of psychosis.5,6 While a few studies have focused on auditory verbal hallucinations3,6,8 that would seem to suggest psychosis, the literature has ignored other phenomena.
We present the results of an observational descriptive study of aberrant perceptions among healthy young adults in a single geographical area in order to define their characteristics, incidence, and associated diseases.
Subjects and methodsParticipantsOur subjects were third, fourth, fifth, and sixth year medical students at Universidad Complutense de Madrid who were completing clinical rotations at Hospital Clínico San Carlos. Inclusion criteria were giving consent to participate in the study, completing the survey, and providing a telephone number or e-mail address. Subjects who did not meet these criteria were excluded from the study.
QuestionnairesWe designed a screening survey in order to identify any subjects who had experienced aberrant perceptions at some point in their lives (Appendix A). The survey collected demographical data including age and sex, contact information, and the items for the study.
Items 1 to 3 enquired about the presence or absence of aberrant perceptions, and only a yes/no response was required. Items 4 to 5 referred to personal and family history of neurological or psychiatric disorders. Items 6 to 8 referred to the consumption of toxic substances, and item 9 to use of medications.
We added 6 yes/no questions to these items. It is important to note that question number 3 (asleep/nearly asleep, aware of losing train of thought) was included as a control question. We consider events in this context to be common sleep-related phenomena rather than hallucinations. We therefore intentionally excluded those subjects who reported only sleep-related events as aberrant perceptions. These subjects were also excluded from the calculation of the total percentage of aberrant perceptions.
The survey was administered to students class by class, and they were informed that the survey was anonymous and voluntary. We also gave examples of common and innocuous aberrant perceptions so as to obtain true responses.
Subsequently, a third year neurology resident (S.G.-P.) took a semi-structured medical history (by telephone or e-mail) from subjects who responded in the affirmative. The process of taking down the medical history included asking directed questions about the hallucination and allowing subjects to respond freely in an imitation of normal clinical practice.
VariablesWe collected the following data: age, sex, family and personal medical history of psychiatric or neurological disorder, frequent headaches, routine medications, alcohol consumption (frequency and quantity), consumption of toxic substances (type and quantity), presence/absence of aberrant perceptions (senses affected, frequency of perceptions, age at onset, isolated/multiple episodes, association with fever, toxic substances, headache, sleep, and subject's analysis of the experience). We also took down subjects’ accounts of the phenomena as they were described.
ResultsThe total sample was N=134. The mean age of the respondents was 22.1 years (typical deviation 1.67). Women accounted for 77.6% (n=104) of the total. At least 1 of the screening questions was answered in the affirmative by 55.22% of the subjects; 40.3% (n=54) then completed the interview.
The most common disorders listed in response to family history were dementia (n=13), Parkinson's disease (n=5), and depression (n=8). The most common disorders given in the personal history were headache (n=20) and asthma. Oral contraceptives were the most common routine medications.
With regard to toxic substances, 20% of the subjects occasionally consumed alcohol, 5% frequently consumed alcohol on weekends, 2 subjects cited higher, but not excessive, levels of alcohol consumption, and 1 subject's daily consumption of alcohol exceeded levels recommended by the WHO. Cannabis consumption was reported by 11%. Consumption of other toxic substances was much less frequent.
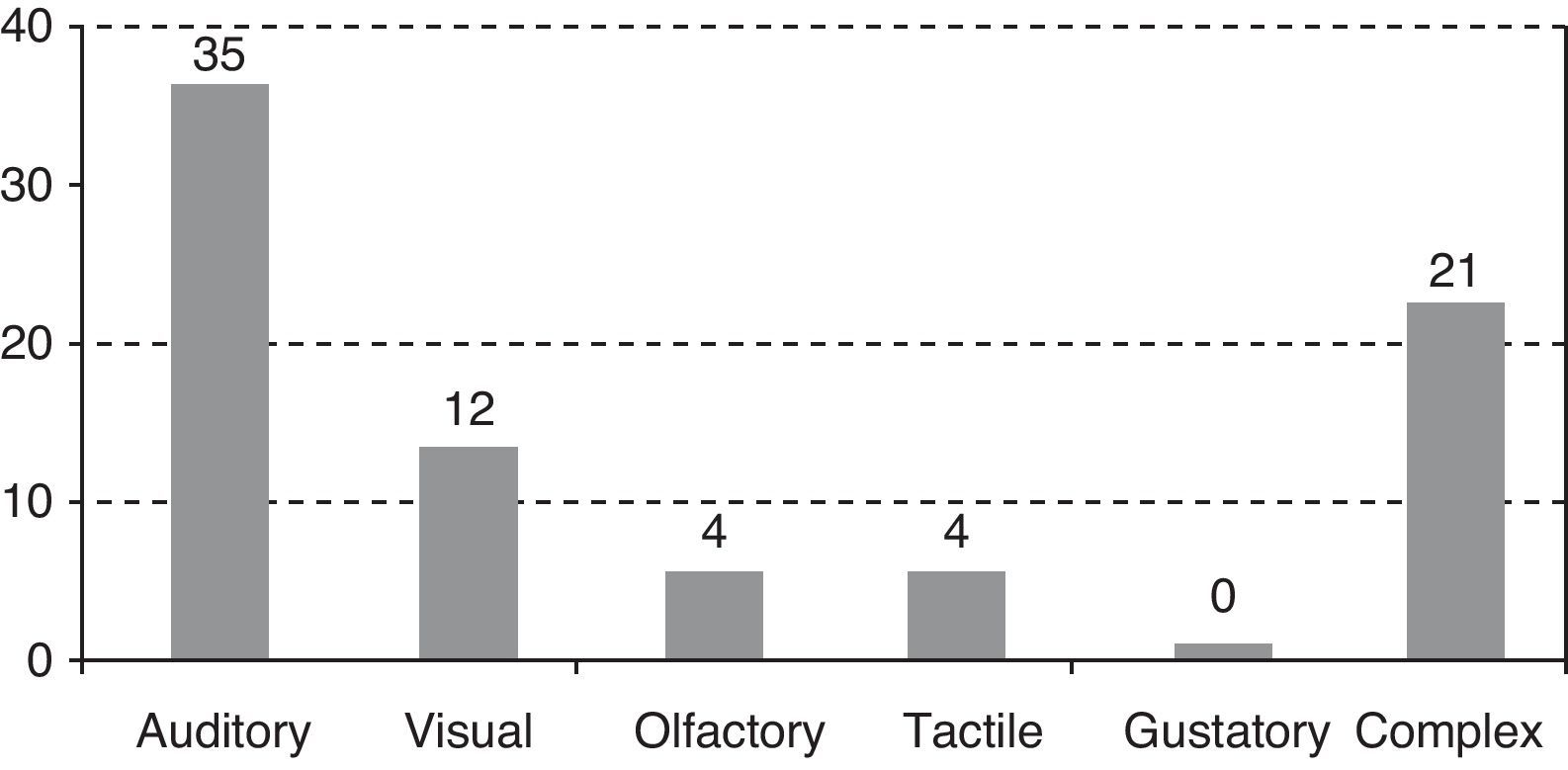
Fig. 1 shows the frequency of the aberrant perceptions classified by sensory modality.
Frequency of appearance was quite variable. Ten subjects had experienced single episodes; 12, fewer than 5 episodes; 6, several episodes per year; 8, several episodes per month; and 2, several episodes per week. None of the subjects experienced daily episodes. Only 1 case was associated with fever and 2 were directly associated with substance abuse (hallucinogens). Subjects were specifically questioned about headaches since we expected to find a high frequency of migraine aura. However, none of the phenomena reported by subjects were associated with headaches, although many experienced headaches during unrelated episodes.
Sleep-related phenomena were reported by a high percentage of subjects (13.4%).
All subjects provided a good analysis of their experiences and none reported psychotic symptoms.
DiscussionAberrant perceptions are frequent symptoms in neurological and psychiatric disorders, but they also appear in the healthy population. Ohayon4 collected data from the non-institutionalised general population older than 15 years in Germany, the UK, and Italy, obtaining a sample of 13,057 subjects. The study was conducted by trained non-medical personnel by means of semi-structured telephone interviews. The incidence of hallucinations in this sample was 38.7%; half of these cases were not associated with any disease. Hypnagogic (sleep onset) hallucinations accounted for 24.8% of the total, with hypnopompic (wakefulness onset) hallucinations accounting for 6.6% of the total; 27% occurred in daytime, 3.2% were visual, and 0.6% auditory. The latter type was associated with psychotic disorder and depression. Tactile hallucinations were uncommon (3.1%) and most commonly associated with toxic substances. This study did not include any members of the Spanish population.
Fonseca-Pedrero et al.5 studied Spanish university students to evaluate predisposition to hallucinations in the healthy population and validate a Spanish-language version of the Launay–Slade Hallucination Scale-Revised. They analysed a sample of 807 young adults but focused on predisposition to hallucinations (rather than hallucinations per se) in an approach aimed at studying mental illness. In another study by Cangas et al.,9 researchers administered the Revised Hallucination Scale to 265 healthy Spanish participants. Once again, their hallucinatory experiences were analysed.
It has long been accepted that some percentage of the population may experience auditory hallucinations without requiring psychiatric treatment. De Loore et al.7 studied a sample of 1800 adolescents and found an incidence of verbal hallucinations of 5%. The hallucinations were still reported 2 years later in 27% of those cases. The presence of hallucinations in this sample was correlated with an increase in mental disorders. However, only persistent hallucinations were associated with an increase in delusional thinking. Another study of adolescents by Dhossche et al.3 described a similar incidence rate and an association with non-psychotic mental illness.
Sommer et al.6 carried out a study in adults using an online survey, but their analysis was limited to subjects with no diagnosis of psychiatric disorders who reported more than 1 verbal hallucination “with good audio quality” per month. Compared to the control population, these subjects had more paranormal beliefs, sleep-related hallucinations, intrusive thoughts, visual hallucinations and vivid fantasies, and higher scores for some schizotypal features. Unlike psychotic hallucinations, these verbal hallucinations were predominantly positive and had little effect on subjects’ daily lives. Authors concluded that isolated episodes of verbal hallucinations in an undiagnosed population might indicate a predisposition to a psychotic disorder. They did concede that their strict selection process could mean that their subjects might not reflect the general population.
The literature tends to focus on typically pathological hallucinations while ignoring other phenomena that could be more prevalent. Lack of a strict definition of a hallucination, added to the fact that most phenomena are self-reported, may explain the considerable variability of figures for incidence given by different studies. If we accept the continuum hypothesis for hallucinations in patients with neurological and psychiatric disorders, ranging from ‘vulnerable’ to healthy subjects, it seems reasonable to establish an even wider range. The hallucinations reported by our medical students could be within that spectrum and provide information about the origin of the symptoms.
The incidence of hallucinations in our study was higher than in other studies. This could be due to using direct questions (the 6 yes/no questions) and our emphasis on sleep-related phenomena. We detected no cases of dementia, which is normal given our subjects’ ages. It is harder to explain the lack of association between hallucinations and mental illness and the low number of phenomena associated with substance abuse.
In both cases, we believe that subjects may have voluntarily omitted this type of information during follow-up interviews. Another possibility could be that studying medicine requires a very high functional level and that subjects with severe mental disorders would not have reached the final years of the programme, thereby excluding themselves from the study. However, these arguments do not explain the absence of non-psychotic psychiatric disorders which was only present in 1 subject. We believe that this condition and substance abuse were both underrepresented in the sample.
Daytime hallucinations are classically associated with neurological and psychiatric disorders, while night-time phenomena seem to be less pathological.4 Although 13% of the sample reported nocturnal phenomena, daytime phenomena were also very frequent and inconsequential.
The high frequency of complex hallucinations in our sample is interesting to note. These episodes occurred in contexts of emotionally stressful situations, poor lighting, or during sleep or childhood. Subjects reported misunderstanding visual perceptions and assigning them different meanings. For instance, a coat on a chair could be mistaken for a person; others, while studying, had a nagging feeling that someone was watching them from behind. Most of these experiences have dreamlike characteristics although they were not directly associated with sleep. All subjects immediately questioned their experiences.
Auditory hallucinations have traditionally been associated with psychotic disorders and other studies show low incidence in the general population.4 Nevertheless, simple auditory perceptions were quite common in our sample. They were all very brief: subjects heard music, their own name or, more frequently, a mobile phone or doorbell ringing when in fact it had not. Some cases were sleep-related, but others may have been linked to hypervigilance. Slight intracranial sounds may be mistaken for external sounds in stressful situations or when ambient noise is very low; most events occurred when subjects were studying or in quiet surroundings.
Olfactory hallucinations were uncommon (only 4 subjects in the sample). At least 2 subjects met criteria for parosmia, that is, perception of a smell which may last for hours; the aetiology of these often chronic phenomena is hard to determine.10,11 None of the events resembled an epileptic aura because their duration was too long.12
The 2 cases of hallucinations associated with substance abuse were visual, as is to be expected. None of these cases were associated with neurological or psychiatric disorders. During the interview, all the subjects presented an analysis of the experience. Most had questioned it immediately after it occurred.
In conclusion, aberrant perceptions are frequent and brief. They affect all sensory modalities and are usually not related to neurological or psychiatric disorders. Auditory phenomena are classically associated with psychotic disorders and other studies indicate a low incidence in the population. Nevertheless, our study suggests that short, simple auditory perceptions in subjects who immediately analyse the experience are common and not pathological.
Conflicts of interestThe authors have no conflicts of interest to declare.
Hallucinations are sensory perceptions that do not correspond to an object. They may be visual, tactile, auditory, olfactory, gustatory, or complex, and they are associated with a wide array of neurological, psychiatric, and systemic disorders. Nevertheless, many healthy people experience hallucinations at some point in their lives without developing any type of disorder.
We would like to ascertain the incidence of hallucinations in a young healthy population, their characteristics, and the circumstances associated with these phenomena. One of our objectives is to clinically distinguish between ‘normal’ hallucinations and those that suggest a disorder.
Please respond to these questions as truthfully as possible. Participation is voluntary. All data will be kept confidential. Please indicate your telephone number or e-mail address so that we may contact you for a second (very short) interview.
Once again, answering the questions will not take long. Thank you for contributing to the progress of science.
Age
Sex
Telephone number or e-mail address (preferably both)
- (1)
Have you ever seen something which was not really there? Examples might be visions, apparitions, voices, smells, tastes, illusions, or perceiving real images in a distorted or different way. These phenomena may have occurred during the day, when you were falling asleep, or when you were waking up.
- (2)
Have you ever perceived something that you know to be impossible?
- (3)
Have you ever been told that something you saw, heard, or felt was not real?
- (4)
Do you have a personal history of neurological or psychiatric disorders?
If you answered “yes”, which disorder(s)?
- (5)
Do you have a family history of neurological or psychiatric disorders?
If you answered “yes”, which disorder(s)?
- (6)
Do you smoke?
If you answered “yes”, how much do you smoke?
- (7)
Do you drink alcohol?
If you answered “yes”, how much do you drink during the weekend? How much do you drink on weekdays?
- (8)
Do you take or have you ever taken any other substances? Examples might be amphetamines, cocaine, ecstasy (MDMA), liquid ecstasy, LSD or naturally occurring drugs such as peyote, magic mushrooms, or cannabis.
If you answered “yes”, how many times in your lifetime/per month/per week? Which drug(s) did you take?
- (9)
Do you take any prescription or non-prescription medications?
If you answered “yes”, which drug(s) do you take and at what dose?
Have you ever:
- 1.
Felt that something or someone was touching you when you were sleeping/nearly asleep?
- 2.
Heard music or your name when you were sleeping/nearly asleep?
- 3.
Lost your train of thought as if you were dreaming when you were sleeping/nearly asleep?
- 4.
Felt the presence of another person in the room when you were sleeping/nearly asleep?
- 5.
Sensed the presence of someone behind you or felt you were being watched (not necessarily associated with sleep).
- 6.
Heard the phone/doorbell ring when in fact it had not.
Once again, please be aware that data will be kept absolutely confidential, as required by law.
Please cite this article as: García-Ptacek S, et al. Las alucinaciones y percepciones aberrantes son prevalentes entre la población joven sana. Neurología. 2013; 28:19–23.