Ischaemic stroke is rare during childhood. Congenital and acquired heart diseases are one of the most important risk factors for arterial ischaemic stroke (AIS) in children.
Patients and methodsWe conducted a retrospective study of all children with AIS and heart disease diagnosed between 2000 and 2014.
ResultsWe included 74 children with heart disease who were eligible for inclusion. 60% were boys with a mean stroke age of 11 months. 20% of the patients died during the study period. 90% of the patients had a congenital heart disease, while cyanotic heart disease was identified in 60%. Hypoplastic left heart syndrome was the most frequent heart disease. In 70% of patients AIS was directly associated with heart surgery, catheterisation or ventricular assist devices. Most patients with AIS were in the hospital. Seizures and motor deficit were the most frequent symptoms. Most patient diagnoses were confirmed by brain CT. The AIS consisted of multiple infarcts in 33% of the cases, affected both hemispheres in 27%, and involved the anterior and posterior cerebral circulation in 10%.
ConclusionsArterial ischaemic strokes were mainly associated with complex congenital heart diseases, and heart procedures and surgery (catheterisation). AIS presented when patients were in-hospital and most of the patients were diagnosed in the first 24hours.
Los ictus isquémicos son poco frecuentes en la infancia. Las cardiopatías tanto congénitas como adquiridas son uno de los factores de riesgo más importante para presentar un ictus en la edad pediátrica.
Pacientes y métodosEstudio retrospectivo descriptivo de niños con cardiopatía diagnosticados de ictus arterial isquémico entre enero del 2000 y diciembre del 2014.
ResultadosCumplieron los criterios de inclusión 74 pacientes, el 60% varones. La mediana de edad del ictus fue de 11 meses. Fallecieron un 20% de los pacientes. La cardiopatía era congénita en un 90%, cianógena en un 60%. El ventrículo izquierdo hipoplásico fue la cardiopatía más frecuente. El ictus estuvo relacionado temporalmente con una cirugía cardiaca, cateterismo o asistencia ventricular en el 70% de los casos.
La mayoría de los ictus ocurrieron en el hospital. La forma de presentación más frecuente fue el déficit motor y las convulsiones. El diagnóstico se realizó mediante TC craneal en la mayoría de los casos. El ictus fue múltiple en el 33% de los casos y bihemisférico en el 27%, y afectaba a la circulación anterior y posterior cerebral en el 10%. En un 10% de los casos se produjo una recurrencia del ictus.
ConclusionesLas cardiopatías congénitas complejas y las intervenciones cardiacas, la cirugía y los cateterismos fueron los principales factores asociados con el ictus isquémico. El ictus se produjo en pacientes hospitalizados y el diagnóstico se realizó en las primeras 24h en la mayoría de los pacientes.
Ischaemic strokes are uncommon in children. Congenital and acquired heart diseases are one of the most frequent risk factors for stroke in children, and are considered to be responsible for 10%-30% of paediatric strokes.1 Despite the significant reduction in mortality due to advances in the management of children with heart disease and the availability of clinical guidelines for the management and prevention of thromboembolic events, the prevalence of ischaemic strokes in these patients has remained stable over the past 30 years.2
Ischaemic strokes in patients with heart diseases can be triggered by various mechanisms3–5:
- –
The formation of emboli in left heart cavities in patients with cardiac arrhythmias, complete or partial ventricular dysfunction, abnormal valves, catheterisation, heart surgery, or the presence of prosthetic material, etc.
- –
The formation of emboli in the venous system or right heart cavities; through a right-to-left shunt, emboli would bypass pulmonary circulation, being transported directly to the cerebral arteries.
- –
Cerebral venous thrombosis due to a combination of several frequent predisposing factors in heart disease patients: venous stasis, dehydration, venous hypertension, and polycythaemia.
- –
Artery diseases: some patients with heart diseases may also present stenotic lesions in the intracranial arteries.
Paediatric stroke particularly occurs in patients with congenital heart disease (mainly in complex cases presenting right-to-left shunt) or cyanotic heart disease.
In addition to congenital heart diseases, other heart-related causes of stroke in children are myocardiopathy, especially dilated and non-compaction cardiomyopathies, arrhythmias, acute myocardial infarction secondary to coronary artery disease, cardiac tumours, infectious endocarditis, and myocarditis.6–8 In these cases, the embolic potential is related to thrombosis caused by the blood stasis manifesting in these diseases.
Very frequently, stroke in these patients is temporally related to some procedure, whether it be heart surgery,9 catheterisation,10 or the use of circulatory support devices (ECMO, Berlin-Heart).11,12
Cardioembolic strokes clinically manifest with sudden-onset focal neurological deficit or seizures. Partial improvement over the following hours or days occurs due to the partial dissolution of the embolus and vessel recanalisation. Frequent complications are the involvement of the posterior circulation and the haemorrhagic transformation of ischaemic strokes due to thrombus dissolution and reperfusion of the infarcted area. The presence of multiple strokes,13 affecting several distinct vascular territories or occurring at different stages of progression, is also typical.
Two sets of guidelines for the management of stroke in children have recently been published: the American College of Chest Physicians Evidence-Based Clinical Practice Guidelines14 and the American Heart Association guidelines.15 In cases of cardioembolic stroke, both documents recommend initiating anticoagulation 5-7 days after stroke is diagnosed and subsequently administering low-molecular-weight heparin or oral anticoagulants for at least 3-6 months, depending on the risk of recurrence.
Only a small number of series of stroke in children with heart diseases have been published. The aim of our study is to describe the epidemiological and clinical characteristics of ischaemic strokes in these patients.
Patients and methodsWe conducted a retrospective descriptive study of children younger than 16 with heart diseases who suffered an arterial ischaemic stroke between January 2000 and December 2014. Hospital Materno-Infantil Gregorio Marañón is a Spanish centre of reference for heart disease in children. The hospital's cardiovascular prevention programme was launched in 1973, and in recent years has performed an annual mean of 170 diagnostic cardiac catheterisations, 300 interventional catheterisations, and 400 cardiac surgical procedures, 185 of which involved extracorporeal circulation. The mean number of heart transplants is 10-12 per year. Using patient clinical histories, we recorded demographic data, data on risk factors and heart disease characteristics, and clinical and analytical data. We also reviewed neuroimaging studies.
We excluded patients with haemorrhagic stroke or transient ischaemic attack, as well as those with such heart diseases as patent foramen ovale and patent ductus arteriosus, due to the high prevalence of both conditions in children and its uncertain connection with stroke.
Normally distributed quantitative variables were expressed as mean±standard deviation; non-normally distributed variables were expressed as median and interquartile range (p25-p75).
Qualitative variables are shown as frequency values and percentages.
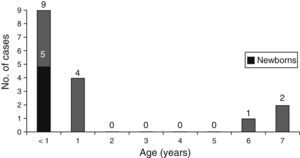
ResultsDemographic dataWe included a total of 74 patients. Median age of stroke onset was 11.7 months (1.6-51.7). Thirty-seven patients (50%) experienced the stroke during the first year of life; in 14 of them (19%) it occurred during the neonatal period. Boys accounted for 60% of the sample. Chromosomal disorders (4 patients with Down syndrome, 3 with 22q11.2 deletion [CATCH 22 syndrome], one with 17p duplication, and one with chromosome 13 deletion) or polymalformative syndromes (one patient with Cornelia de Lange syndrome, one with cranio-cerebello-cardiac [3C] syndrome, and the remaining 3 with polymalformative symptoms of unknown origin) were present in 19% of patients. Sixteen patients (21.6%) were deceased when this study was carried out, 8 of these (11%) died shortly after the stroke occurred, during hospital admission.
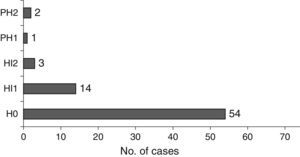
As shown in Fig. 1, patients died at young ages. Of the 16 deceased patients, 2 (2.7%) died as a consequence of stroke-related events; the other 14 died due to complications related to the heart disease or other causes.
Heart diseaseHeart disease was congenital in 89% and acquired in 11% of patients. Cyanotic heart disease accounted for 63.5% of cases.
Heart diseases were classified into 4 groups, according to severity and treatment:
- –
Group 1. Heart conditions requiring surgery during the neonatal period: 49%.
- –
Group 2. Cyanotic heart conditions not requiring treatment during the neonatal period: 20%.
- –
Group 3. Ventricular dysfunction: 14%.
- –
Group 4. Other heart diseases: 17%.
Most of the patients who died belonged to group 1 (those needing surgery during the neonatal period).
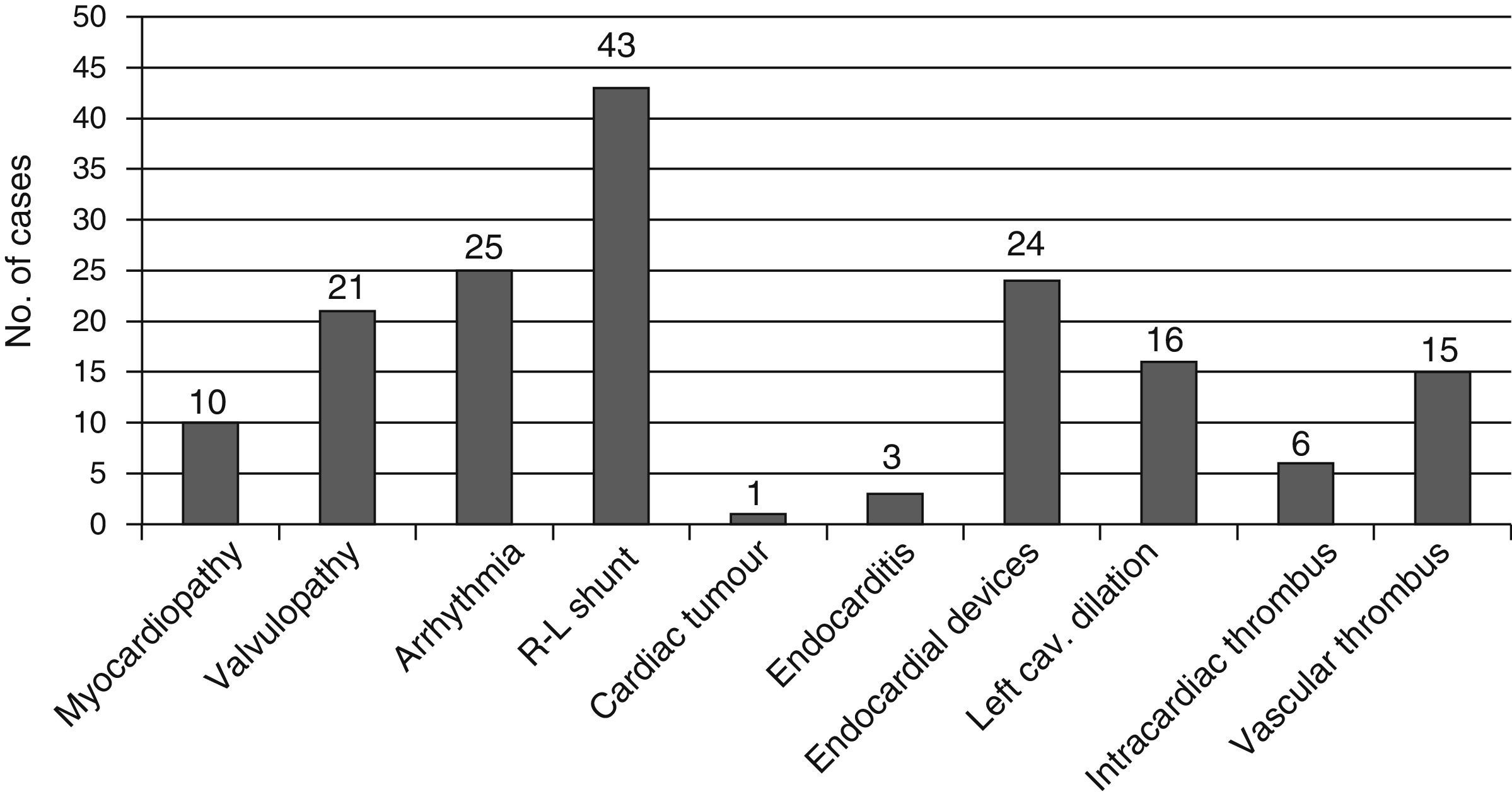
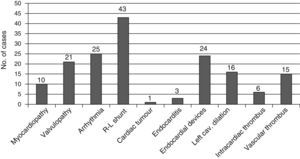
At the time of stroke, many patients presented one or several cardiological factors linked to a higher risk of cardioembolic events (Fig. 2).
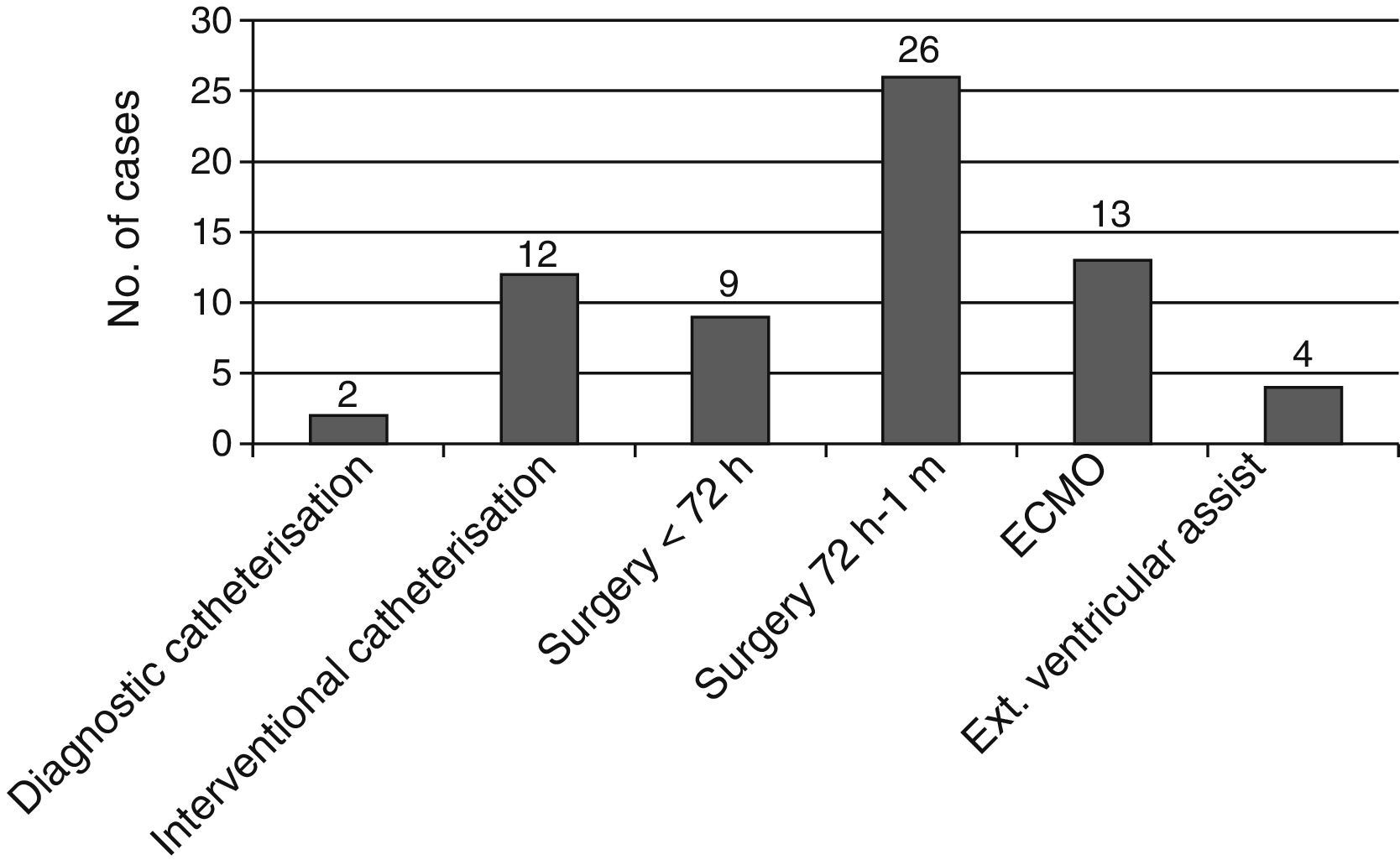
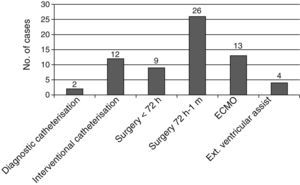
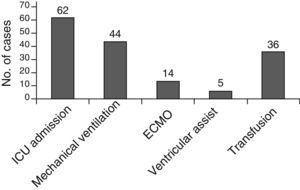
Fig. 3 shows the strokes which were temporally associated with some cardiac procedure, catheterisation, or implantation of ventricular assist devices. Stroke was not associated with any procedure in only 22 patients (30%).
Stroke characteristicsThe first clinical symptoms of stroke manifested outside hospital in 18% of the patients. The remaining patients experienced symptoms while at the ICU (67%) or the paediatric inpatient ward (15%).
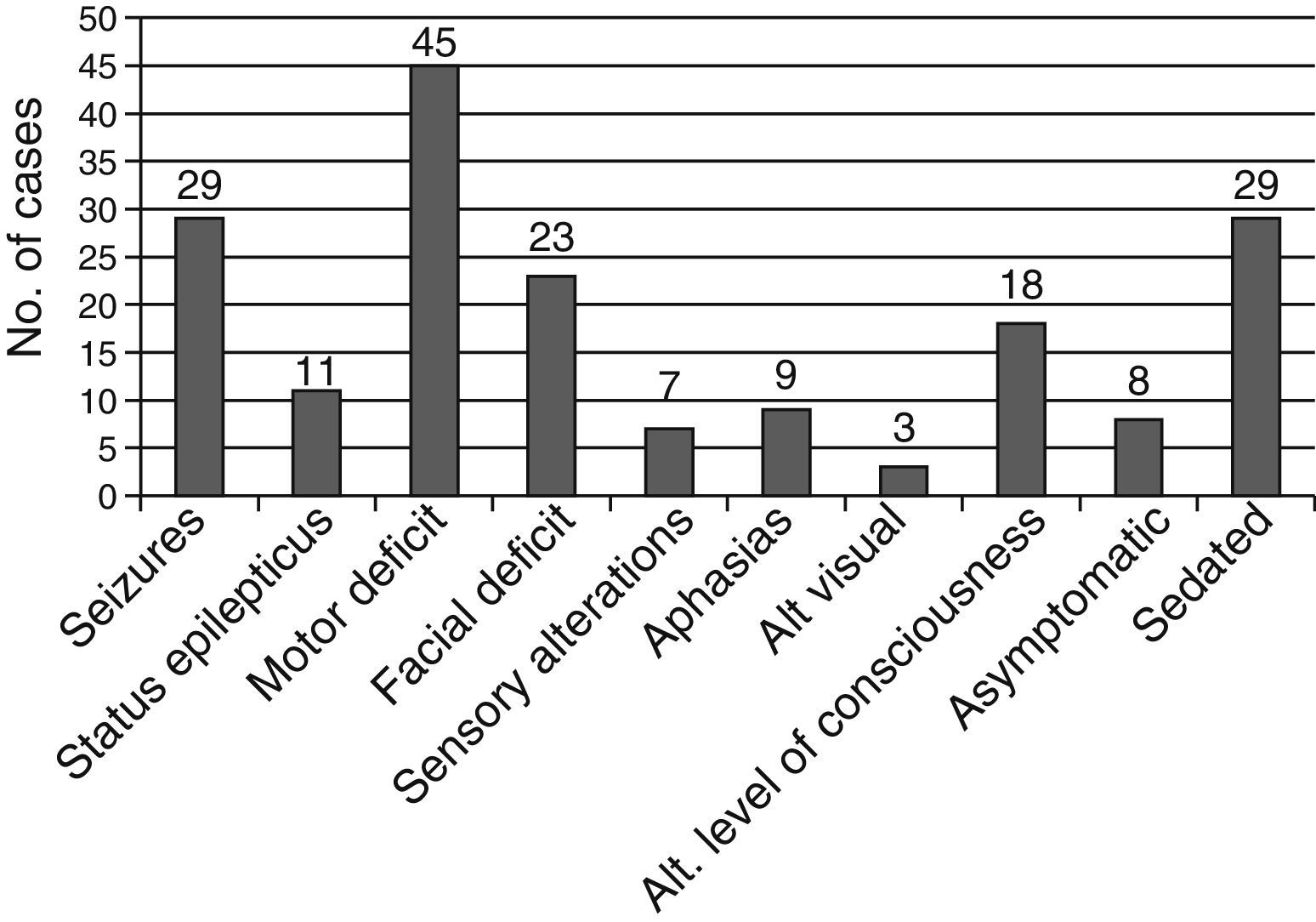
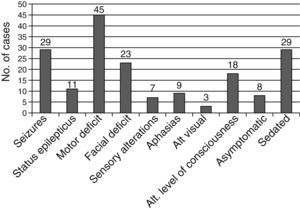
A total of 29 patients (39.2%) were receiving some type of pharmacological sedation at the time of stroke, which could have delayed diagnosis. The patients’ clinical symptoms are shown in Fig. 4.
One third of the patients presented other thromboembolic events, with deep vein thrombosis being the most frequent, followed by thrombi in cardiac cavities and venous sinus thrombosis.
Diagnostic testsDiagnosis was performed using cranial CT scan in 35 patients, brain MRI in 26 patients, and brain ultrasound in 13. Furthermore, a diffusion-weighted MRI was performed in 41 patients (55.4%), and a brain MRI angiography in 24 patients (32.4%).
Median delay between onset of the first clinical symptoms and the first radiological study with positive results was 0.50 days (0.00-3.25).
Location of stroke was multiple in 33% and bilateral in 27% of patients. Of the 54 cases of unilateral stroke, the right hemisphere was affected in 61%. Stroke affected the anterior circulation area in 81.1% of the cases, the posterior circulation area in 5.4%, and both in 13.5%.
Stroke most frequently affected the middle cerebral artery (MCA) territory, involving the cortical MCA territory in 80%, the subcortical MCA territory in 74%, and the basal ganglia in 39% of cases. Stroke affected the anterior cerebral artery territory in 3 patients (4.1%) and the posterior cerebral artery territory in 14 patients (18.9%). We found no cases in which the basilar artery was fully affected.
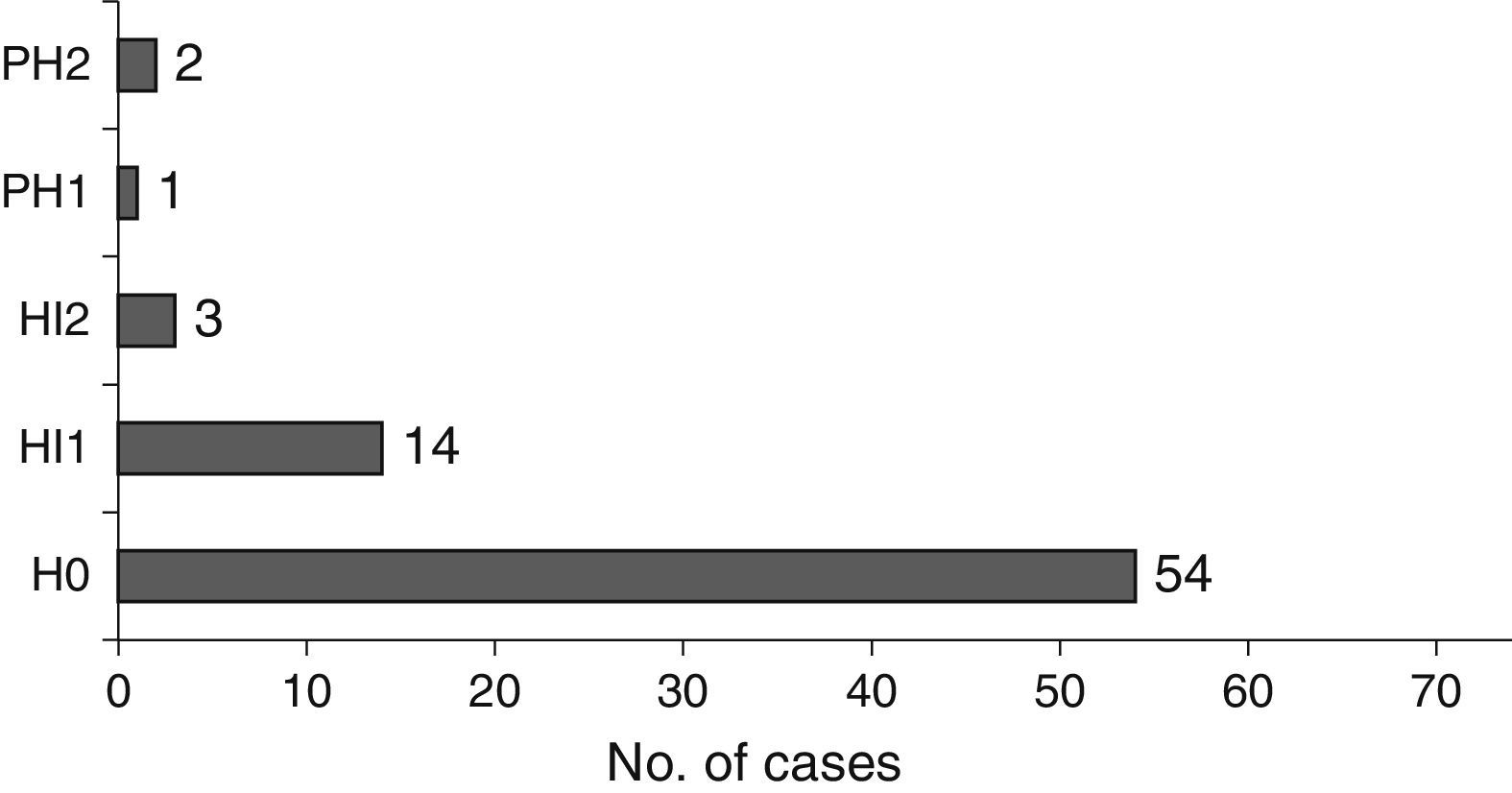
In terms of size, stroke was lacunar in 5 patients (6.8%), medium in 34 (45.9%), and large in 35 (47.3%). Nineteen patients (25.7%) experienced massive MCA stroke. In 27% of cases, stroke presented a haemorrhagic component (Fig. 5).
Electroencephalographic studies were performed during the acute phase of stroke in 40 patients (54.1%), whose results were: normal in 6 patients (15%), generalised slow activity in 4 (10%), focal slow activity in 21 patients (52.5%), focal epileptiform activity in 8 patients (20%), and generalised epileptiform activity in one case (2.5%).
A complete coagulation study was conducted in only 30 patients (40%), with abnormal results in 14 patients (protein C deficiency in 6, protein S deficiency in 2, MTHFR mutation in 5, and multiple deficits secondary to infection in one); results were normal in 16 patients. The remaining patients underwent no study or testing was incomplete.
TreatmentAt the time of stroke, 48 patients (65%) were receiving prophylactic treatment: antiplatelet therapy in 15 (20% of the total), anticoagulants in 25 (34%), both antiplatelet and anticoagulant therapy in 7 (10%), and dual antiplatelet drugs in one (1%). The remaining 26 patients (35%) were not receiving prophylactic treatment.
Most patients (61 patients, 82.4%) were admitted to hospital at the time of stroke.
No patient received intravenous or intra-arterial fibrinolytic treatment. Twenty-four patients (32%) received antiplatelet treatment, and 48 patients (65%) anticoagulant therapy. Two patients (3%) were treated with corticosteroids to reduce the cerebral oedema, 27 patients (36%) received acute treatment with antiepileptic drugs, and 9 patients (12%) received antihypertensive drugs.
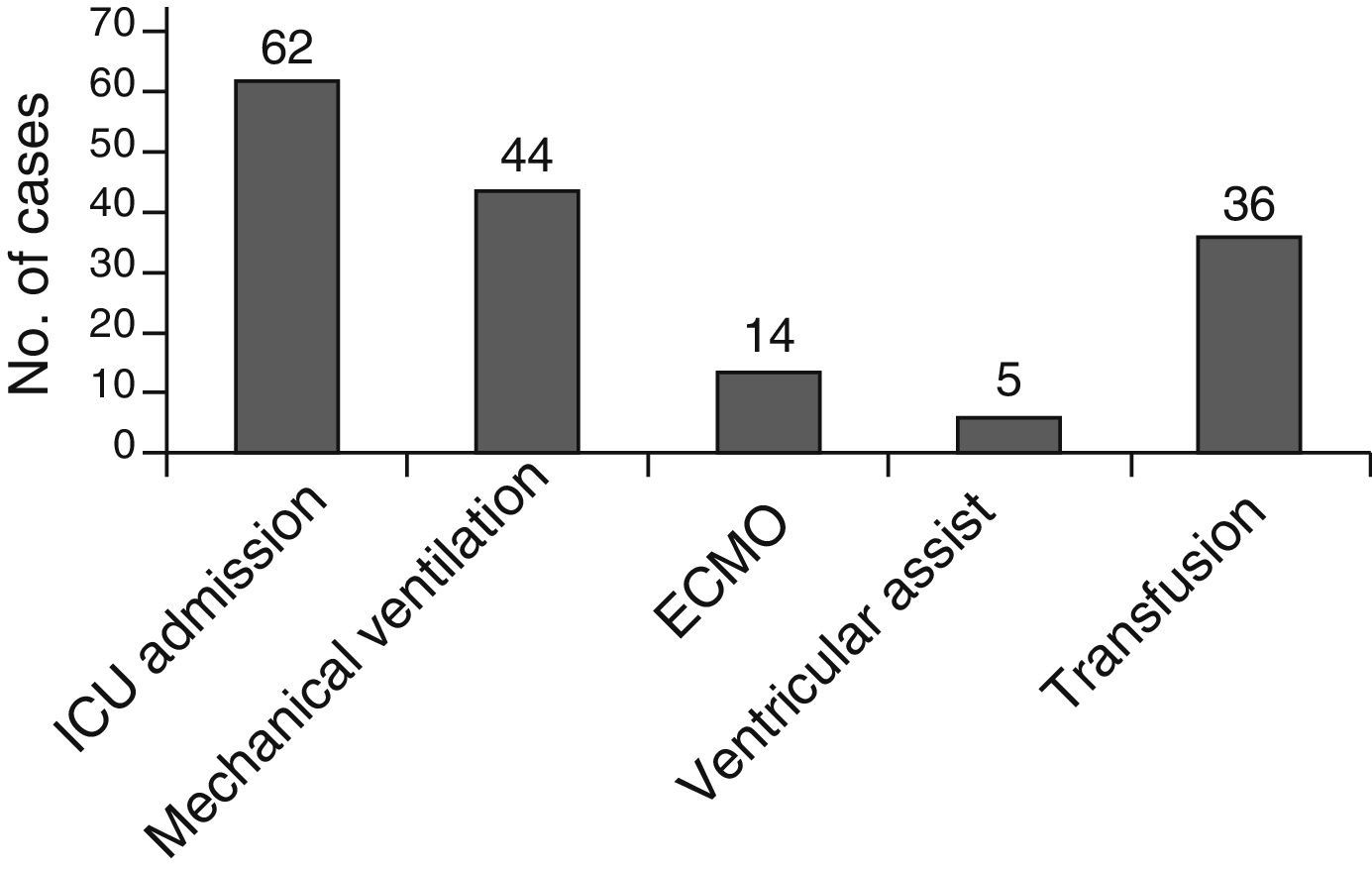
Most patients (62 patients, 83.7%) were admitted to the neonatal or paediatric intensive care unit (ICU) at the time of stroke; many of them had previously been admitted to the ICU due to their heart conditions. Fig. 6 shows the supportive treatments used.
RecurrenceStroke recurred in 8 (11%) of the 74 patients. The new stroke occurred a median of 98.50 days (34.50-341.25) after the sentinel event. In half of these patients (4 cases) recurrence occurred during the first 3 months, while they were hospitalised due to the first stroke. In the remaining cases, recurrence occurred after discharge and up to 3 years after the sentinel event.
Recurrence was most frequent in patients with endocarditis during the sentinel stroke (33% vs 10% of patients not displaying endocarditis), but the difference was not significant. We found a recurrence rate of 20% among patients with endocardial devices vs 6% found in those with no devices (P=.05).
Four patients (50%) with stroke recurrence died during the follow-up period. None of the patients with recurrence displayed complete clinical recovery at discharge.
DiscussionWe describe the epidemiological characteristics of 74 children with heart disease presenting with ischaemic stroke at our hospital over the past 15 years.
The patients in our series are predominantly boys, with a percentage similar to that reported in other paediatric stroke series.16 We found that the age of stroke onset in children with heart disease (median of 11.7 months) was lower than that described in the literature in children with stroke of any aetiology (78 months) and for series of paediatric stroke associated with heart diseases (37.2 months).17 We believe this is explained by the fact that patients in our series had more complex heart diseases, requiring treatment during the neonatal period.
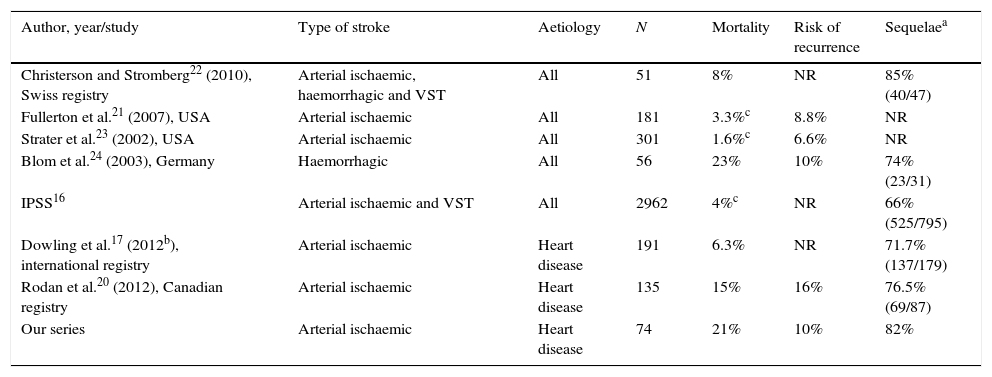
The mortality rate was higher in our patients (21%) than that described in the literature for series of paediatric ischaemic stroke of any aetiology,18–23 and similar to that of haemorrhagic stroke in children24 (Table 1). Furthermore, the in-hospital mortality rate in our study (11%) is higher than that described in the literature for children with stroke and heart disease.17,20 Also, patients died at early ages, most of them during the first year of life. These patients had complex heart diseases which required surgery during the neonatal period, and their deaths were related to heart problems in the majority of cases. No other series reports the percentage of patients with polymalformative syndrome or chromosomal disorder, which was very high in our series (almost 20%); this could also have had a role in the higher mortality rate observed in our series.
Mortality, recurrence, and morbidity of stroke in children from the main series published.
| Author, year/study | Type of stroke | Aetiology | N | Mortality | Risk of recurrence | Sequelaea |
|---|---|---|---|---|---|---|
| Christerson and Stromberg22 (2010), Swiss registry | Arterial ischaemic, haemorrhagic and VST | All | 51 | 8% | NR | 85% (40/47) |
| Fullerton et al.21 (2007), USA | Arterial ischaemic | All | 181 | 3.3%c | 8.8% | NR |
| Strater et al.23 (2002), USA | Arterial ischaemic | All | 301 | 1.6%c | 6.6% | NR |
| Blom et al.24 (2003), Germany | Haemorrhagic | All | 56 | 23% | 10% | 74% (23/31) |
| IPSS16 | Arterial ischaemic and VST | All | 2962 | 4%c | NR | 66% (525/795) |
| Dowling et al.17 (2012b), international registry | Arterial ischaemic | Heart disease | 191 | 6.3% | NR | 71.7% (137/179) |
| Rodan et al.20 (2012), Canadian registry | Arterial ischaemic | Heart disease | 135 | 15% | 16% | 76.5% (69/87) |
| Our series | Arterial ischaemic | Heart disease | 74 | 21% | 10% | 82% |
NR: not reported; VST: venous sinus thrombosis.
Most of our patients had a complex congenital heart disease; of these, 63% were cyanotic heart diseases. Our patients’ heart diseases were severe, with almost 50% requiring surgery during the neonatal period; most patients presented multiple heart risk factors. Hypoplastic left heart syndrome was the cardiopathy most frequently associated with stroke, as has been described previously.2
In children with heart disease, strokes frequently occur shortly after some cardiac procedure. It is estimated that one in 200 children undergoing cardiac surgery suffers a stroke, with a higher incidence rate for complex procedures and reoperations.9 Stroke is a frequent complication of both diagnostic and interventional catheterisations in these patients due to the endothelial lesion caused by the catheter, the formation of thrombi at the tip of the catheter, and the rupture and embolisation of tissue in interventional catheterisations.10 In addition to this, the use of circulatory support devices (ECMO, Berlin-Heart) in patients not responding to conventional means of ventilation or in patients with severe heart failure may cause ischaemic or haemorrhagic stroke due to the requirement for prolonged systemic heparin administration, the alterations in cerebral pulsatile flow it causes, and the possibility of microthrombi forming in circuits.11,12
In our series, more than 50% of patients experienced stroke with a temporal relation to some procedure, whether cardiac surgery (almost half of patients had undergone surgery in the previous month) or catheterisation (19%), particularly interventional catheterisation. It should be noted that our hospital performs a high number of interventional catheterisations, which are very frequently urgent and of great complexity; this would increase the percentage of strokes related to interventional catheterisations in comparison with other series.17
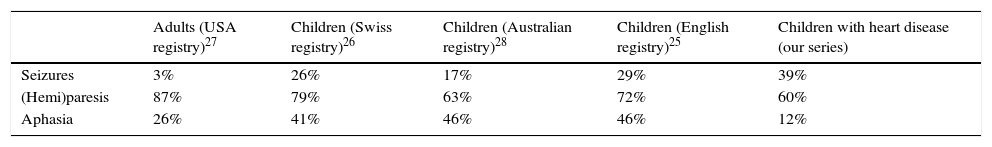
The most frequent presentations in our study were motor deficit and convulsive seizures, similar to those seen in strokes of other aetiologies in children, and with a higher rate of seizures than in adult strokes (Table 2).25–28 We found a lower percentage of speech alterations, explained by the young age of our patients. We should underscore that we found many patients with no symptoms at the time of stroke, probably due to pharmacological sedation, since stroke mainly occurred in the ICU, in the postoperative period following cardiac surgery.
A delay has been reported in the diagnosis of stroke in children, due to prolonged sedation after cardiac surgery, the absence of motor signs in infants, and the difficulty of performing imaging studies in patients who are haemodynamically unstable or with temporary or permanent metallic devices which contraindicate MRI.29 In our patients, diagnosis was confirmed by radiological study in the first 24 hours from symptom onset in 63% of the cases, a shorter delay than that described in the literature,30 which we attribute to the high percentage of patients in our series who were already hospitalised at the time of the stroke.
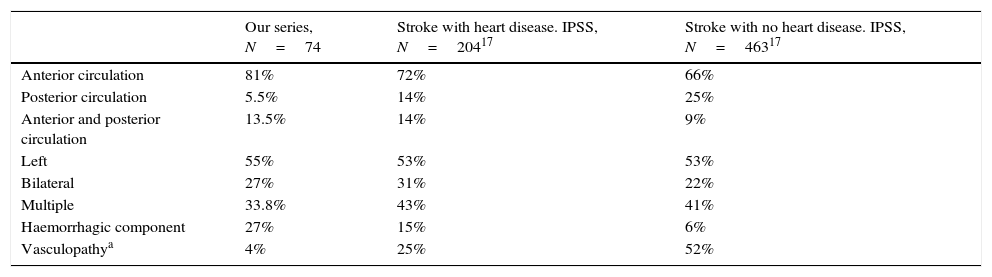
In 2013, the International Pediatric Stroke Study (IPSS) published a retrospective multicentre study which compared 204 children with stroke and heart disease to 463 children with stroke of any aetiology.17 When comparing the characteristics of our neuroimaging findings to those of that study, we can observe a similar percentage of patients with involvement of both anterior and posterior circulation, and patients with bilateral stroke, between studies (Table 3). We found a lower proportion of patients with multiple stroke. The low percentage of associated vascular disease in our series is striking; this is explained by the limited number of brain MRI angiographies performed (in only one third of the patients). Current guidelines recommend performing vascular studies even where a thromboembolic origin is suspected.31 We observed a higher percentage of stroke with a haemorrhagic component than that seen in the IPSS series17; this component was probably associated with the higher rate of cardiac surgery, mechanical circulatory support devices, or anticoagulant therapy.
Neuroimaging findings for ischaemic strokes in our series and other series of stroke with and without heart disease.
| Our series, N=74 | Stroke with heart disease. IPSS, N=20417 | Stroke with no heart disease. IPSS, N=46317 | |
|---|---|---|---|
| Anterior circulation | 81% | 72% | 66% |
| Posterior circulation | 5.5% | 14% | 25% |
| Anterior and posterior circulation | 13.5% | 14% | 9% |
| Left | 55% | 53% | 53% |
| Bilateral | 27% | 31% | 22% |
| Multiple | 33.8% | 43% | 41% |
| Haemorrhagic component | 27% | 15% | 6% |
| Vasculopathya | 4% | 25% | 52% |
We found a stroke recurrence rate of 10%, with stroke occurring during hospital admission for the sentinel event in half of cases. This percentage is higher than that reported for ischaemic stroke of any aetiology in children and lower than that in series of haemorrhagic strokes (Table 1).20,21,23,24 In 2012, Rodan et al.20 reported a recurrence rate of 16% in a series of 135 children with heart disease and ischaemic stroke. In this series, transient ischaemic attacks and silent strokes are considered recurrence; this is not the case in our study, which may explain this difference.
Factors reported in the literature as being related to recurrence of ischaemic stroke in children with heart diseases are the presence of endovascular devices, infection symptoms/fever during the sentinel event, or abnormal prothrombotic study results.20 Our study also found a higher recurrence rate in patients with endovascular devices, but not for the other 2 factors (fever or thrombotic diathesis). The low percentage of patients in our series who underwent prothrombotic study may partly explain these differences.
We conclude that complex congenital heart diseases and cardiac surgery were the main factors associated with ischaemic stroke. Stroke occurred in hospitalised patients and diagnosis was established in the first 24 hours in most patients. The mortality rate was high and was related to the severity of heart disease.
FundingThis study received no public or private funding.
Conflicts of interestAll authors have given their approval for the publication of the manuscript. The authors have no conflicts of interest to declare.
Please cite this article as: Vázquez-López M, Castro-de Castro P, Barredo-Valderrama E, Miranda-Herrero MC, Gil-Villanueva N, Alcaraz-Romero AJ, et al. Ictus isquémico en niños con cardiopatía: estudio epidemiológico. Neurología. 2017;32:602–609.
This study was presented as an oral communication at the 38th Annual Meeting of the Spanish Society of Paediatric Neurology (SENEP) in Logroño, 21-23 May 2015. It was awarded one of the 5 prizes for best oral communications at the 2015 SENEP meeting.