One of the consequences of poor postural control in children with cerebral palsy is hip dislocation. This is due to the lack of weight-bearing in the sitting and standing positions. Orthotic aids can be used to prevent onset and/or progression.
ObjectiveThe aim of this study is to analyse the effectiveness of positioning systems in achieving postural control in patients with cerebral palsy, and discuss these findings with an emphasis on what may be of interest in the field of neurology.
DiscussionWe selected a total of 18 articles on interventions in cerebral palsy addressing posture and maintenance of ideal postures to prevent deformities and related problems. The main therapeutic approaches employed combinations of botulinum toxin and orthoses, which reduced the incidence of hip dislocation although these results were not significant. On the other hand, using positioning systems in 3 different positions decreases use of botulinum toxin and surgery in children under 5 years old. The drawback is that these systems are very uncomfortable.
ConclusionPostural control systems helps control hip deformities in children with cerebral palsy. However, these systems must be used for prolonged periods of time before their effects can be observed.
Una de las consecuencias de la mala calidad en el control postural de los niños con parálisis cerebral es la luxación de caderas. Esto es debido a la falta de carga de peso en las posiciones de sedestación y bipedestación. Para ello, se puede hacer uso de ayudas ortésicas para evitar su aparición o progresión.
ObjetivoEl objetivo de este estudio es analizar la efectividad de dichos sistemas de posicionamiento en el control postural de pacientes con parálisis cerebral, y discutir estos hallazgos a la luz de lo que pueda ser de interés para la neurología.
DiscusiónSe seleccionaron un total de 18 artículos de intervenciones de la parálisis cerebral infantil que abordaban el ámbito de la postura y su mantenimiento en posiciones idóneas para evitar deformidades y problemática relacionada. Los principales resultados terapéuticos fueron: combinación de toxina botulínica junto con ortesis, que reduce la incidencia en la luxación de caderas, aunque estos resultados no fueron significativos, y el empleo de sistemas de posicionamiento en 3 posturas diferentes, que supone un descenso en el empleo de la toxina botulínica y de las intervenciones quirúrgicas en niños menores de 5 años. El inconveniente es que resultan muy incómodos.
ConclusiónEl empleo de sistemas de control postural produce beneficios en el control de las deformidades de cadera en niños con parálisis cerebral. Sin embargo, su utilización debe ser prolongada en el tiempo para que los efectos sean objetivos.
Human posture during different activities requires adjusting the body's position to maintain the centre of gravity within the base of support.1,2 Postural control depends on the visual, somatosensory, and vestibular systems as well as on the central nervous system's ability to interpret information and execute actions.3–8
This ability to adjust posture is impaired in children with cerebral palsy (CP). Problems in adapting the degree of muscle contraction may explain why these children display excessive coactivation of antagonist muscles groups, especially during such complex voluntary tasks as reaching and balancing.9,10
Maintaining postural control frequently requires excessive activation of antagonist muscles.11–13 The most frequently affected area is the axial plane of the human body: over 65% of all patients with CP have scoliosis, and between 28% and 60% have hip problems.14,15
Hip problems are therefore a common complication in CP as well as a source of pain during adolescence and adulthood. Although the hips of children with CP are normal at birth, they subsequently undergo structural changes due to imbalances between adductor/abductor and flexor/extensor muscles, and also because of decreases in muscle extension and joint range of motion.16
These problems are especially marked in children with more severe neurological impairment and those incapable of walking or weight-bearing: delays in reaching these motor milestones increase the risk of hip deformation, whereas standing promotes acetabular development.14,15,17 Patients with spasticity show alterations in the hip migration percentage (HMP) and acetabular index (AI); these indicators are used to evaluate hip deformities (subluxation or dislocation).18
Therefore, clinical practice aims to provide early interventions, including use of special seats, night-time support, standing support, and orthotic aids, as well as personalised therapies. Support devices include custom-moulded sitting and standing aids19; orthotics such as the SWASH orthosis ensuring hip abduction in the sitting, standing, and walking positions20; and postural support systems such as the Chailey adjustable postural support,21 which allows hip abduction in lying, sitting, and standing positions and is frequently used as a complement to physical therapy. The purpose of our review article is to determine the effectiveness of interventions with different postural support systems and examine their benefits for CP patients with, or at risk of, hip subluxation or dislocation.
DevelopmentWe conducted a literature search in MEDLINE, Ovid, CINHAL, PEDRo, and Índice Médico Español using the following keywords: cerebral palsy, hip deformity, subluxation, subluxated, hip subluxation, postural control, postural management, standing, standing posture, seated, seated posture, and corset, both in English and in Spanish. We also searched for combinations of these terms and truncated the keywords to retrieve all possible variations.
We limited our search to articles written in English, Spanish, or Portuguese, including human participants, and with an abstract available online. Likewise, we decided to increase the date range and include studies conducted in other countries. In addition, we manually searched the online journals considered to be most relevant for this topic and also used the snowball method, that is, reviewing the references cited by the articles included in our study to identify articles not returned by the database search.
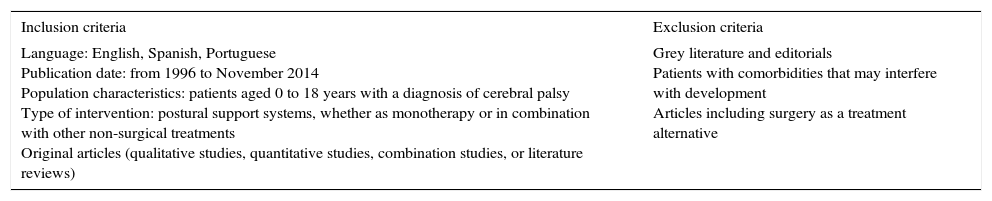
We obtained a total of 34 potentially useful studies and excluded 16 articles which did not meet the inclusion criteria described previously. Inclusion and exclusion criteria are summarised in Table 1. Table 2 provides a summary of the most relevant articles included in our review.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Language: English, Spanish, Portuguese Publication date: from 1996 to November 2014 Population characteristics: patients aged 0 to 18 years with a diagnosis of cerebral palsy Type of intervention: postural support systems, whether as monotherapy or in combination with other non-surgical treatments Original articles (qualitative studies, quantitative studies, combination studies, or literature reviews) | Grey literature and editorials Patients with comorbidities that may interfere with development Articles including surgery as a treatment alternative |
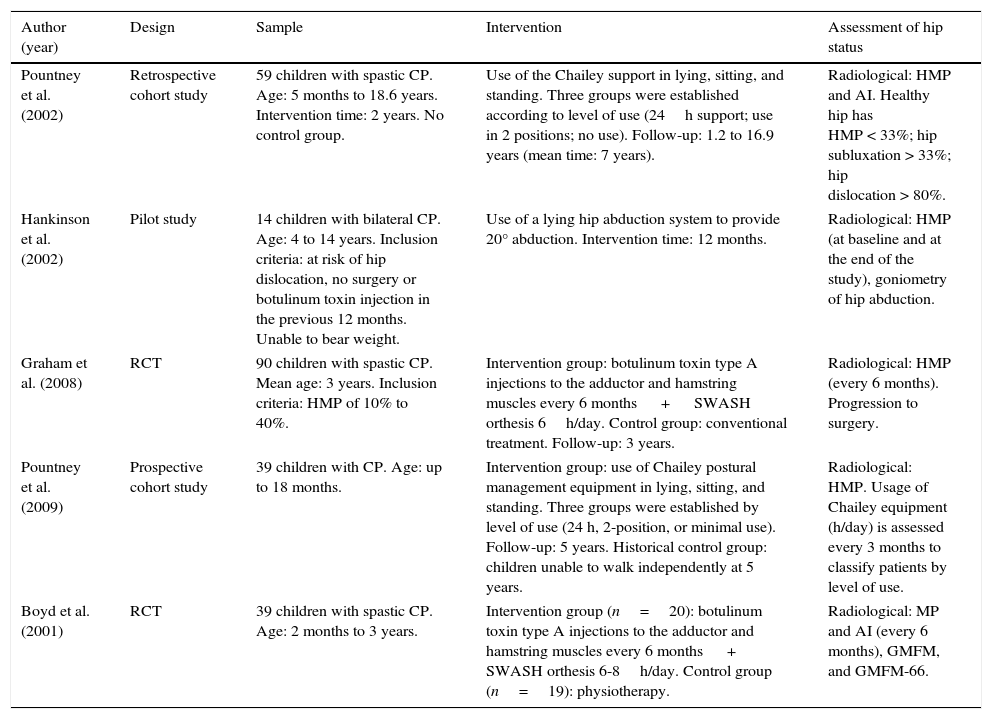
General characteristics of the articles included in our review.
| Author (year) | Design | Sample | Intervention | Assessment of hip status |
|---|---|---|---|---|
| Pountney et al. (2002) | Retrospective cohort study | 59 children with spastic CP. Age: 5 months to 18.6 years. Intervention time: 2 years. No control group. | Use of the Chailey support in lying, sitting, and standing. Three groups were established according to level of use (24h support; use in 2 positions; no use). Follow-up: 1.2 to 16.9 years (mean time: 7 years). | Radiological: HMP and AI. Healthy hip has HMP < 33%; hip subluxation > 33%; hip dislocation > 80%. |
| Hankinson et al. (2002) | Pilot study | 14 children with bilateral CP. Age: 4 to 14 years. Inclusion criteria: at risk of hip dislocation, no surgery or botulinum toxin injection in the previous 12 months. Unable to bear weight. | Use of a lying hip abduction system to provide 20° abduction. Intervention time: 12 months. | Radiological: HMP (at baseline and at the end of the study), goniometry of hip abduction. |
| Graham et al. (2008) | RCT | 90 children with spastic CP. Mean age: 3 years. Inclusion criteria: HMP of 10% to 40%. | Intervention group: botulinum toxin type A injections to the adductor and hamstring muscles every 6 months + SWASH orthesis 6h/day. Control group: conventional treatment. Follow-up: 3 years. | Radiological: HMP (every 6 months). Progression to surgery. |
| Pountney et al. (2009) | Prospective cohort study | 39 children with CP. Age: up to 18 months. | Intervention group: use of Chailey postural management equipment in lying, sitting, and standing. Three groups were established by level of use (24 h, 2-position, or minimal use). Follow-up: 5 years. Historical control group: children unable to walk independently at 5 years. | Radiological: HMP. Usage of Chailey equipment (h/day) is assessed every 3 months to classify patients by level of use. |
| Boyd et al. (2001) | RCT | 39 children with spastic CP. Age: 2 months to 3 years. | Intervention group (n=20): botulinum toxin type A injections to the adductor and hamstring muscles every 6 months + SWASH orthesis 6-8h/day. Control group (n=19): physiotherapy. | Radiological: MP and AI (every 6 months), GMFM, and GMFM-66. |
The first approach that we will describe here was used by Graham et al.22 and Boyd et al.23 Both studies evaluated the effects of intramuscular injections of botulinum toxin type A to the adductor and hamstring muscles every 6 months. Postural treatment was provided in the form of a SWASH orthosis, which enables hip abduction, for 6 to 8hours daily. Regarding the effects of the intervention, Graham et al.22 describe progression of hip displacement in both groups, although the percentage of migration was lower in the intervention group, with a difference of 1.4% between groups.
During the follow-up period, the rate of surgery for hip control was lower in the intervention group than in the control group. However, this difference in rates disappeared once the intervention was finished. The intervention was relatively well tolerated by the participants given that the SWASH brace is a variable hip abduction orthosis. Pascual-Pascual24 conducted a study with 98 children receiving botulinum toxin injections to the adductor, hamstring, and iliopsoas muscles in addition to orthotic therapy and physiotherapy; in this study, progression of femoral head displacement halted in 74% of the patients and reversed in 14%. Boyd et al.23 only provide the number of children requiring surgery due to an HMP over 40%: 7 patients in the control group vs 2 in the intervention group. Motor function, however, was similar in both groups. Therefore, although these 2 studies report positive effects of combined treatment with botulinum toxin type A injection and use of a variable hip abduction orthosis, their results are not significant. We should point out that both studies were randomised clinical trials (RCT) and therefore have a good methodological quality.
The studies by Pountney et al.20,25 involved 24-hour use of a postural control system, the Chailey support, which positions the hip and pelvis adequately to allow better fitting of the femoral head into the acetabulum. This system can be used with the patient in a lying, sitting, or a standing position. Both studies20,25 are cohort studies, although only one includes a control group.25 The first study20 has a more heterogeneous sample (age ranges from 5 months to 18.6 years) and the second one25 is more homogeneous in terms of both sample characteristics and follow-up time (patients younger than 18 months who were monitored for 5 years). Both studies classified the sample by use of the Chailey support: the first group used it in all 3 positions, that is 24hours a day (recommended use), the second group in 2 of the 3 possible positions (moderate use), and the third group in only one or none of the positions (minimal use). The group using the Chailey support in all 3 positions showed less pronounced hip migration and a lower risk of hip problems.20,25,26 Patients undergoing the intervention before the age of 5 were less likely to need surgery or botulinum toxin type A injections; this is the reason why the second study included only those patients younger than 18 months; the follow-up period was 5 years.25
The literature also reports use of hip postural support systems during sleep. The purpose of these devices is to achieve and maintain hip abduction during night-time sleeping hours. The study by Hankinson and Morton,27 a pilot study including 14 patients and no control group, used a system that maintains a hip abduction of 20°. One of the most striking findings from this study was its high drop-out rate (50% of the total), which was explained by the discomfort this static system caused to patients. The children who completed the intervention (18 months) displayed an 11% decrease in HMP, increased hip abduction, and improved gait pattern.
Another therapeutic approach is the use of custom-moulded plaster cast orthoses for sitting and standing.28 These systems enable postural control while sitting and provide a safe base of support that allows patients to use their hands and manipulate objects. We have found only one study using this system. However, this study has a lower methodological quality since it is a case report of 2 children who had not responded to other treatment approaches.28 In both cases, the HMP decreased over 3 years, although this system needs to be used for at least 5hours a day. In any case, the results of the case report mentioned above cannot be extrapolated to the population with CP due to the nature of the study.
When comparing the results from the studies included in this review, we should bear in mind that the studied populations are homogeneous (children with bilateral CP), but age and follow-up times are not. For example, one of the studies included children younger than 18 months,26 whereas other studies also included adolescents.20,27 Early intervention is based on the assumption that patients with low degrees of hip subluxation experience significantly more marked improvements than patients with greater degrees of hip subluxation.20
As for the systems used, 2 studies combined botulinum toxin type A injection with a variable hip abduction orthosis,22,23 whereas the remaining studies used static systems.25,27,29
The literature demonstrates that static systems are a valid option for controlling progression of hip deformities, but they require long-term use to be more effective and are also more uncomfortable for patients.28 The reviewed studies of static systems have methodological limitations inherent to their study design: one was a case report, another was a pilot study, and there were 2 cohort studies (only one of these included a control group). Dynamic hip abduction systems demonstrate limited success; although they have shown favourable results, these are not statistically significant. However, the studies that examined them demonstrate greater methodological quality (2 RCT).22,23 We should also bear in mind that dynamic systems are better tolerated than static systems. Studies with more precise methodological approaches will be necessary to evaluate the effects of static systems.
All interventions used a hip abduction of 20°; this angle achieves good femoral head coverage by the acetabulum. In all cases, postural support systems were used for more than 5–6hours a day, and for periods longer than 18 months; usage time was found to be directly correlated with the level of control of hip deformities.20,25 We should highlight the studies by Abd El-Kafy30 and Kim et al.31, which used systems to control progression of hip deformities. The first of these studies evaluated the effectiveness of a static ankle orthosis for improving gait; use of this system also affected flexion of the ipsilateral knee and hip. This intervention was found to significantly improve kinetic and kinematic parameters in the patient sample (57 children). The second study used a custom-moulded fitting chair in 34 severely disabled children. The intervention lasted 24 months, after which 19 patients displayed a lower degree of hip subluxation.
The studies included in our review have a number of limitations. Firstly, some studies had poor methodological quality, as mentioned previously: only 2 were RCTs22,23 and another included a historical control group25; 2 of the remaining 3 studies have very small sample sizes (2 and 7 patients).27,29 Furthermore, differences in the systems used and in follow-up times do not allow us to compare their results.
Although the level of evidence provided by these studies is insufficient to support use of postural support systems for managing patients with hip deformities, the studies do suggest that these systems may help control and even reverse progression.
Regarding follow-up times, it seems clear that these systems require long-term use (over 2-3 years) in order to achieve observable results. In conclusion, we should stress the importance of conducting these interventions as early as possible, since success rates are greater for patients with lower degrees of hip subluxation.20,25 Monitoring the state of the hip when children with CP start walking is therefore essential.29
ConclusionOur literature review shows that postural support systems are useful for the management of hip deformities in children with CP. However, these interventions require long-term use for at least 5 or 6hours per day to achieve observable results. Research shows that the effects are more marked when these systems are used for longer periods.
FundingThis study received funding from the University of Almería, Spain (Department of Nursing, Physiotherapy, and Medicine).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-de la Cruz S. Parálisis cerebral infantil y el uso de sistemas de posicionamiento para el control postural: estado actual del arte. Neurología. 2017;32:610–615.