Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of the central nervous system caused by reactivation of John Cunningham (JC) virus in immunosuppressed individuals.1 Immunosuppressive treatment in patients with haematologic neoplasms predisposes to the development of the disease2; it is extremely rare for PML to be diagnosed before the neoplasm. We present the case of a patient with PML as the initial manifestation of systemic lymphoma.
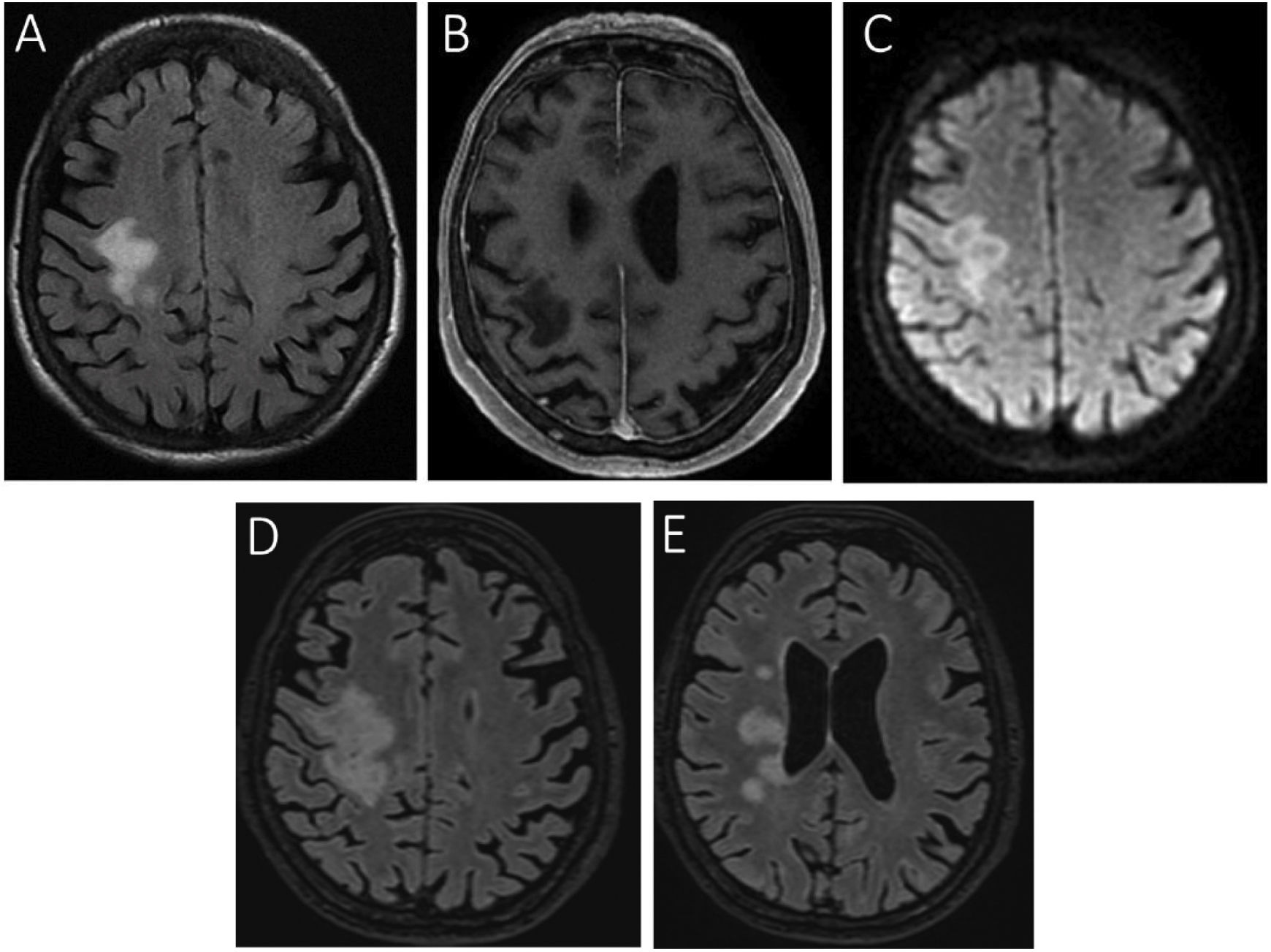
In March 2020, a 74-year-old woman was admitted to our hospital due to a 2-month history of progressive muscle weakness of the left upper limb. Physical examination revealed left hemiparesis and ipsilateral central facial palsy. Blood analysis revealed mild anaemia (haemoglobin: 11.9 g/dL) and elevated erythrocyte sedimentation rate (62 mm/h) and beta-2-microglobulin level (6789 µg/L). Brain MRI showed altered signal intensity in the right frontal lobe, which displayed diffusion restriction, but no contrast enhancement on T1-weighted sequences (Fig. 1A–C). The patient was discharged with a diagnosis of ischaemic stroke and began rehabilitation treatment. Two months later, she was readmitted due to worsening of hemiparesis. A brain MRI study revealed progression of the lesion (Fig. 1D and E). PCR testing for JC virus in the CSF yielded positive results. Treatment was started with mirtazapine at 15 mg/24 hours and citalopram at 20 mg/24 hours, but symptoms did not improve.
Brain MRI study.
Axial slices from FLAIR (A), gadolinium-enhanced T1-weighted (B), and diffusion-weighted sequences (C) at the time of the patient’s first admission, showing altered signal in the right perirolandic area, extending to the centrum semiovale. The lesion presents no contrast enhancement, and appears hyperintense on the diffusion-weighted sequence. Two months later (D), the initial lesion had increased in size, extending to the corpus callosum and internal capsule; small satellite lesions were also visible in the adjacent white matter (E).
Suspecting an underlying neoplastic disease, we performed a chest and abdomen CT scan, which revealed splenomegaly and adenopathic conglomerates in the abdomen and pelvis; these findings are suggestive of a lymphoproliferative process. Finally, after an inguinal biopsy, the patient was diagnosed with high-grade B-cell non-Hodgkin lymphoma. In the light of the progressive worsening, chemotherapy was ruled out. However, we did start infusions of cidofovir dosed at 5 mg/kg, administered twice weekly. During treatment, the patient presented a partial motor improvement. A further brain MRI study showed a slight reduction in the size of the lesions. On account of the patient’s significant clinical improvement after 8 months’ treatment with cidofovir, we decided to start a cycle of chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. A follow-up CSF analysis performed before onset of chemotherapy revealed a considerable reduction in the number of copies of JC virus (710 IU/mL, vs 15 960 IU/mL in the previous study). However, 14 months after symptom onset, the patient died due to massive intracranial haemorrhage.
DiscussionWe present the case of a patient whose diagnosis of a haematologic neoplasm resulted from the detection of PML. We believe that the systemic lymphoma caused a state of immunosuppression that predisposed the patient to PML, as she was not receiving any immunosuppressive treatment. Differential diagnosis considered the possibility of lymphoma dissemination to the brain due to the diffusion restriction in the lesions; however, treatment with cidofovir led to a clear clinical and radiological improvement, and significantly decreased JC viral load in the CSF.
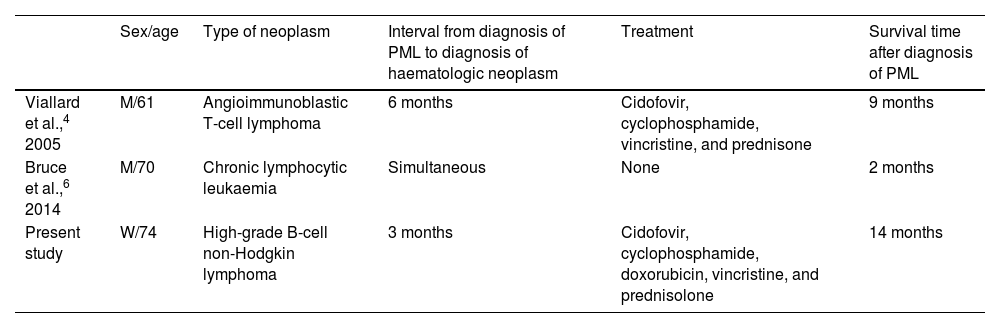
Primary asymptomatic infection with JC virus occurs during childhood in most patients, with the virus subsequently remaining latent.1 In immunosuppressed individuals, the virus infects and destroys oligodendrocytes, causing progressive demyelination of white matter in the brain.3 After HIV-positive individuals, patients with haematologic neoplasms are the largest group at risk of developing PML. In addition to the immunosuppression caused by the haematologic-oncological disease itself, chemotherapy and immunosuppressive treatments cause a further deterioration of these patients’ immune status. A retrospective study conducted at an oncology centre gathered clinical data from 16 patients with haematologic cancer and diagnosed with PML in the period 2000-2015. All but one of the patients had previously been treated with chemotherapy.2 It is even rarer for diagnosis of PML to precede diagnosis of the neoplasm (Table 1). As shown in the table, our patient’s survival time was somewhat longer than those of other patients with similar characteristics.
Cases of progressive multifocal leukoencephalopathy preceding diagnosis of haematologic neoplasm.
| Sex/age | Type of neoplasm | Interval from diagnosis of PML to diagnosis of haematologic neoplasm | Treatment | Survival time after diagnosis of PML | |
|---|---|---|---|---|---|
| Viallard et al.,4 2005 | M/61 | Angioimmunoblastic T-cell lymphoma | 6 months | Cidofovir, cyclophosphamide, vincristine, and prednisone | 9 months |
| Bruce et al.,6 2014 | M/70 | Chronic lymphocytic leukaemia | Simultaneous | None | 2 months |
| Present study | W/74 | High-grade B-cell non-Hodgkin lymphoma | 3 months | Cidofovir, cyclophosphamide, doxorubicin, vincristine, and prednisolone | 14 months |
M: man; PML: progressive multifocal leukoencephalopathy; W: woman.
With respect to treatment, the available options are limited and the clinical outcomes are rarely satisfactory.3,4 Prognosis is generally fatal, with a mortality rate of approximately 90% at 2 months after diagnosis.5,6
In conclusion, our case demonstrates that PML can be the initial manifestation of a haematologic neoplasm, and underscores the importance of tumour screening in patients presenting PML in the absence of any apparent cause of immunosuppression.
Informed consentThe patient gave written informed consent to the publication of this study.
FundingThis study has received no specific funding from any public, commercial, or non-profit organisation.
Conflicts of interestThe authors have no conflicts of interest to declare.