It was with great interest that we read the letter by Gómez Iglesias et al.1 We would like to present another case of mild encephalitis/encephalopathy with reversible splenial lesion (MERS). This is a reversible clinical and radiological entity characterised by lesions to the splenium of the corpus callosum with restricted diffusion on MRI sequences.2,3 It may present with a wide range of neurological manifestations and may have different aetiologies2,4–6; a high level of suspicion is therefore necessary for appropriate management.
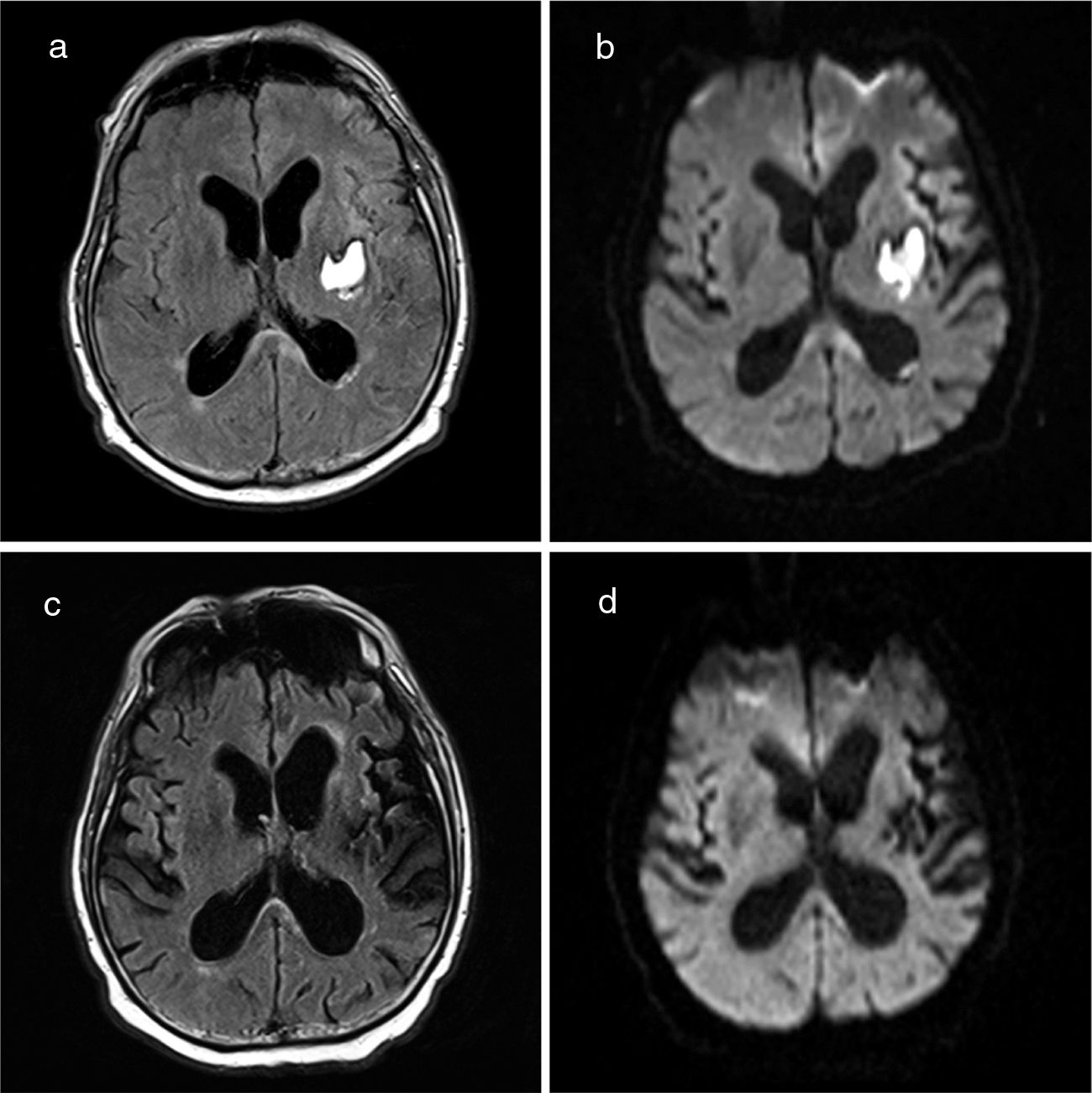
We present the case of a 66-year-old man with history of hypertension and frequent alcohol consumption (48 g/day). He was admitted to the neurology department due to left internal capsule haemorrhage (Intracerebral Hemorrhage Score of 1) manifesting with unilateral motor symptoms. He required labetalol perfusion due to a tendency to hypertension. After 24-48 hours, he developed confusion, psychomotor agitation, and hallucinations. An axial CT scan performed at this time showed no changes with respect to baseline images. He started treatment with tiaprizal 100 mg/8 hours. In the following days, the patient presented fever and a progressive decrease in the level of consciousness. A blood analysis revealed leukocytosis and high C-reactive protein levels. We suspected a respiratory tract infection secondary to bronchoaspiration, and started antibiotic therapy; the patient was transferred to the intensive care unit for ventilatory support. Chest radiography revealed increased density in the right lower lobe. Blood, saliva, and urine cultures yielded negative results. The neurological examination revealed a Glasgow Coma Scale score of 10 (eye 4, verbal 1, motor 5), with mutism, right hemianopsia (lack of menace response), and right hemiplegia. Inflammatory biochemical parameters normalised after 12 days with antibiotic therapy, but fever persisted. An immunological study including tests for tumour markers and serology tests for neurotropic viruses in the blood and CSF yielded negative results. Electroencephalography revealed no epileptiform activity. A brain MRI scan performed 20 days after onset of coma revealed a lesion to the splenium of the corpus callosum, showing restricted diffusion (Fig. 1), and signs of subarachnoid haemorrhage in the left convexity. Due to suspicion of MERS in the context of probable posterior reversible encephalopathy syndrome (PRES), the patient remained under close neurological and haemodynamic monitoring, showing systolic blood pressure values around 140-160 mm Hg. The patient’s level of consciousness progressively improved and visual disorders resolved, but motor deficits persisted. A follow-up MRI scan performed 35 days after the initial study revealed nearly complete resolution of the corpus callosum lesion (Fig. 1).
MERS constitutes the clinical and radiological manifestation of a large group of processes, including infection, autoimmune diseases, antiepileptic drug toxicity, metabolic disorders, trauma, and PRES.5–7 The pathophysiology of the syndrome remains poorly understood. The corpus callosum, and particularly the splenium, has a high density of cytokine receptors, glutamate, and toxins, which makes it more vulnerable to cytotoxic oedema than other brain regions.7 The characteristic MRI findings in MERS (corpus callosum lesions with restricted diffusion) have been interpreted as cytotoxic oedema,8,9 which may be caused by cytokinopathy.7
The case presented here manifested with hypertensive haemorrhage. Given our patient’s progression, with hypertension, visual hallucinations, and altered level of consciousness, and imaging findings of subarachnoid haemorrhage in the convexity, we hypothesise that MERS was secondary to PRES.
PRES is characterised by headache, visual alterations, altered level of consciousness, epileptic seizures, and other neurological deficits.10 The syndrome is usually accompanied by sustained hypertension, and subarachnoid haemorrhage in the convexity is a frequent finding.11 Although the aetiopathogenic mechanism of PRES is not clear, the syndrome has been associated with alterations in endothelial self-regulation, which results in fluid extravasation, vasogenic oedema (with no diffusion restriction on MRI), and release of proinflammatory cytokines.12,13 The posterior circulation territory is particularly susceptible to disruption of vascular self-regulation. In our patient, cytokinopathy secondary to sustained endothelial dysfunction may have triggered the formation of cytotoxic lesions in the splenium. Endothelial dysfunction may also explain the subarachnoid haemorrhage.
Both MERS and PRES are clinical syndromes with typical radiological features that may manifest with severe neurological symptoms. We should consider an association between the 2 syndromes in patients with unexplained alterations in the level of consciousness.
FundingNo funding was received for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pagola-Lorz I, Cámara MS, Diaz-Pertuz ED, Erro ME. Coma por lesión reversible del cuerpo calloso. Neurología. 2020;35:671–672.