Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) is a clinical-radiological entity1 characterised by symptoms of encephalopathy, which may be mild or severe, associated with decreased level of consciousness, irritability, delirium, language alterations, and occasionally seizures and fever. T2-weighted and FLAIR MRI sequences show hyperintensities without contrast enhancement in the centre of the corpus callosum, which resolve completely.2 Many cases of MERS have been described in children; however, the condition is much less frequent among adults.3 Its prevalence in radiological series is 3%. The broad clinical spectrum of MERS makes differential diagnosis difficult.4,5 The aetiology of the syndrome includes metabolic alterations, toxicity, viral or bacterial infection, and drug withdrawal. The exact pathophysiological mechanisms and the reason for the preferential involvement of the corpus callosum are unknown. In most cases, the clinical-radiological course of the disease is self-limited, with lesions resolving spontaneously, and prognosis is favourable; however, cases with poor outcomes have also been reported. We present a case of adult-onset MERS to help expand our knowledge of this rare entity.
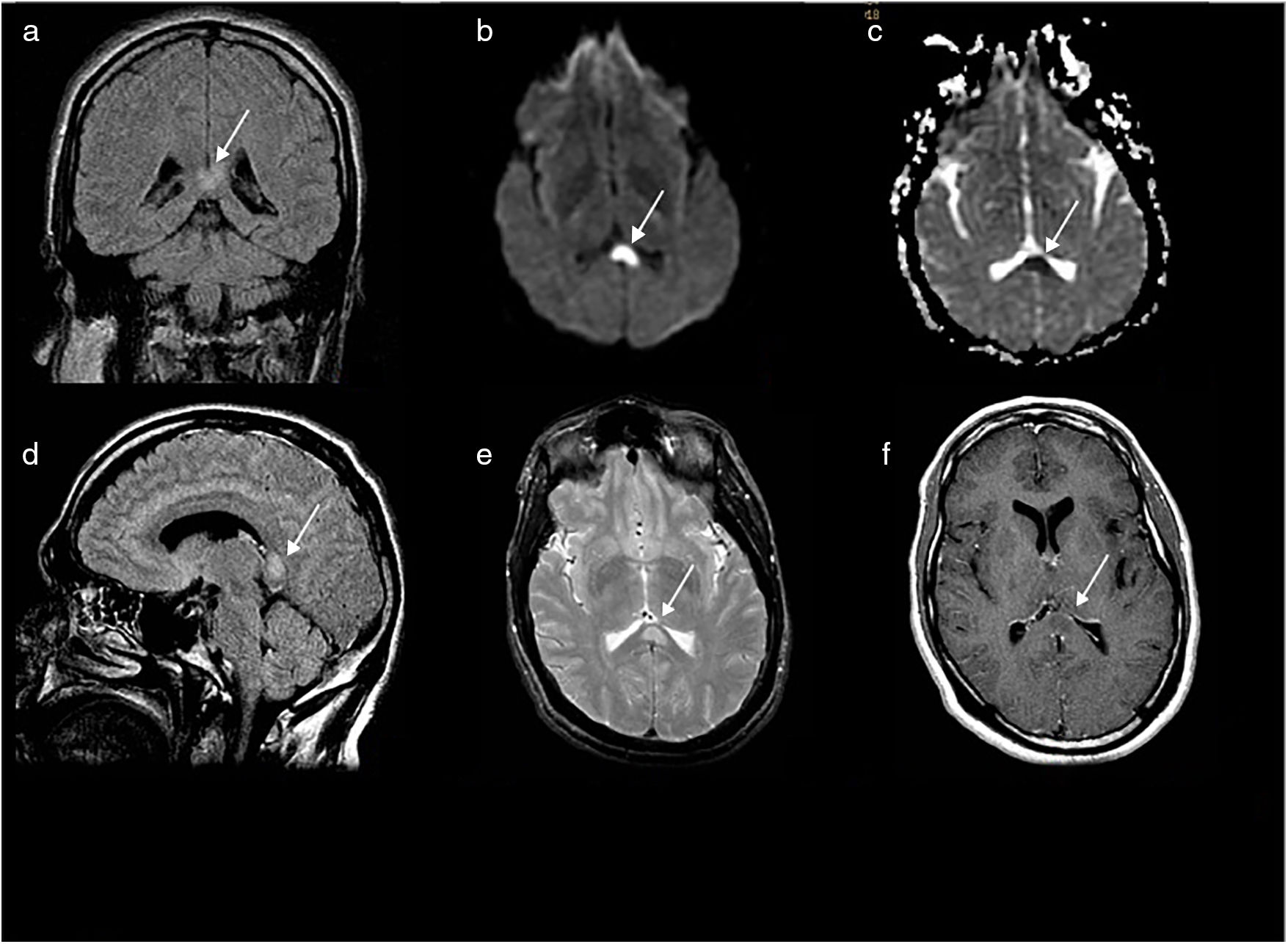
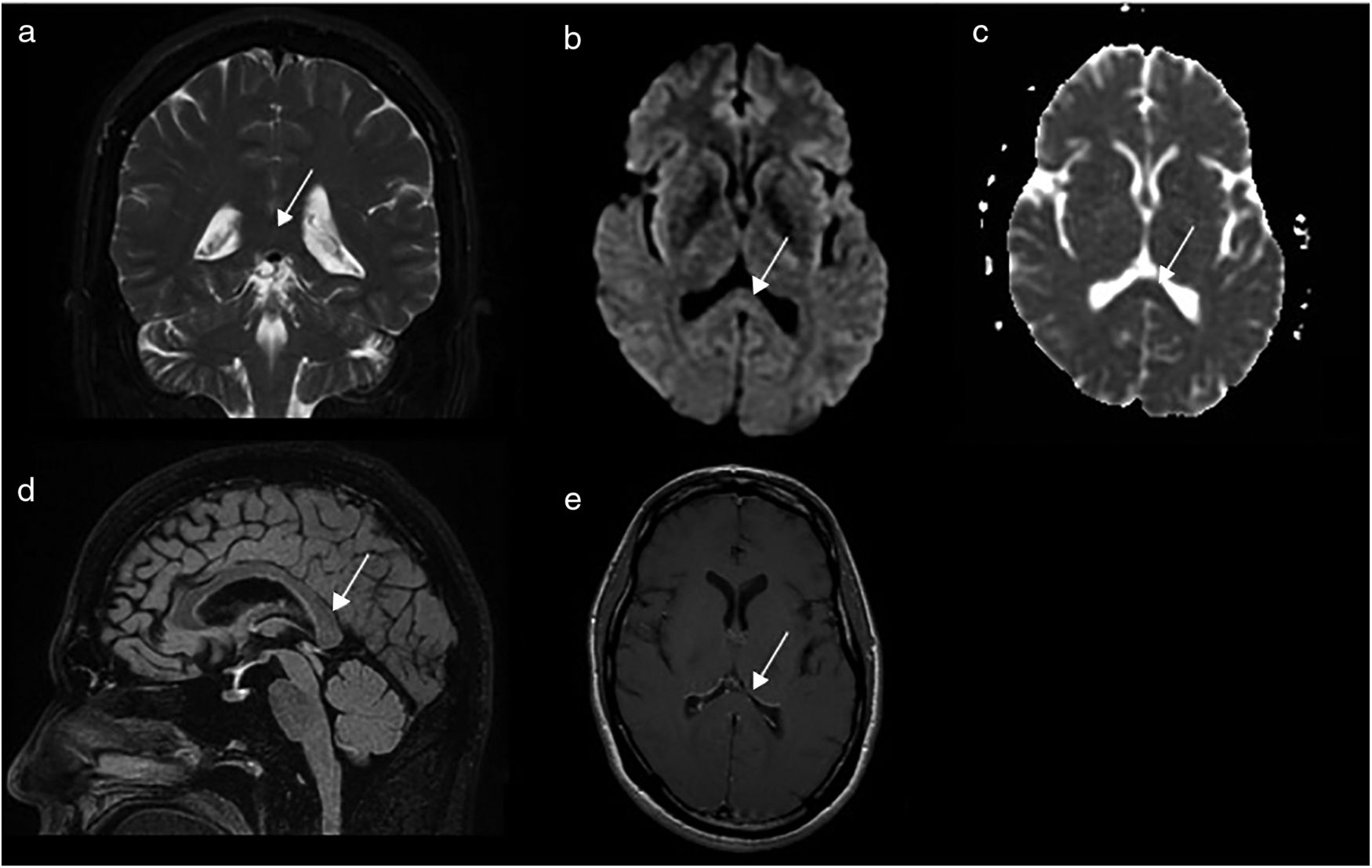
Our patient was a 33-year-old man from Croatia with schizophrenia and drug and alcohol addiction; he was enrolled in a drug rehabilitation programme and receiving olanzapine. He was evaluated due to an episode of aggressiveness in a public space. The previous week he had disappeared from the rehabilitation centre; no witnesses were available who could give information on what had happened after his disappearance. Upon arrival at the emergency department, the patient presented fever (39 °C), confusion, and disorientation, with episodes of marked psychomotor agitation. The neurological examination detected no focal signs. A chest radiography and urine analysis yielded no abnormal findings. Urine toxicology test results were negative. A blood analysis revealed high levels of creatine phosphokinase (9353), creatinine, and urea, with no other relevant findings. The results from a CSF analysis were normal. EEG and video-EEG showed no epileptiform activity. An emergency brain CT scan revealed no alterations. Empirical treatment was started with aciclovir. A brain MRI scan performed at 24 hours revealed an oval-shaped focal lesion in the splenium of the corpus callosum, on the midline, measuring 12 mm in diameter; the lesion was hyperintense on T2-weighted FLAIR sequences, and showed restricted diffusion and no contrast uptake (Fig. 1). Aciclovir was withdrawn, but support measures (fluid therapy, neuroleptics) were maintained. A complete screening study testing for autoimmune diseases, tumour markers, and antineuronal antibodies, and serology tests for neurotropic viruses in the blood and CSF, yielded negative results. Our patient’s level of consciousness progressively improved; his health status returned to baseline and he presented no further episodes of agitation and delirium. A follow-up brain MRI scan performed at 17 days showed complete resolution of the corpus callosum lesions (Fig. 2). The patient was diagnosed with MERS in view of the encephalopathy symptoms and the reversible nature of the corpus callosum lesions. In this case, MERS may have been caused by the suspension of previous treatment with olanzapine, possible drug or alcohol use in the days preceding admission (urine toxicology tests were negative, but the triggering substance may not have been detected), or infection; the latter is the most frequent aetiology of MERS. The differential diagnosis of patients presenting symptoms compatible with MERS should include posterior reversible encephalopathy syndrome (frequently associated with arterial hypertension and subcortical white matter involvement), acute disseminated encephalomyelitis, multiple sclerosis (particularly relapsing-remitting forms), Marchiafava–Bignami disease (associated with chronic alcohol consumption), ischaemia (irreversible and distributed according to the affected vascular territory), diffuse axonal injury (associated with head trauma), lymphoma (contrast uptake on MRI), central pontine myelinolysis (electrolyte imbalance), HIV infection, and epilepsy (associated with introduction/discontinuation of drugs, seizures).
Baseline brain MR images obtained in a 1T MRI scanner: coronal (A) and sagittal (D) 2D T2-weighted FLAIR pulse sequences; axial EPI-DWI sequence (b = 1000 s/mm2) (B); axial T2-weighted FSE sequence (E); post-contrast axial T1-weighted FSE sequence (F); and axial greyscale ADC map (C). Signal alterations are observed in the left central and lateral splenium (white arrow), with restricted diffusion and no contrast enhancement. These findings are compatible with cytotoxic oedema. No alterations were observed in the rest of the corpus callosum (D) or in any other part of the brain parenchyma.
Follow-up MR images obtained 17 days later in a 1.5T scanner: coronal T2-weighted FSE sequence (A); axial EPI-DWI sequence (b = 1000 s/mm2) (B); sagittal 3D-FSE Cube FLAIR sequence (D); post-contrast axial T1-weighted FSE sequence (E); axial greyscale ADC map (C). The images show complete resolution of the cytotoxic oedema in the splenium (white arrows) and no lesions in the rest of the brain parenchyma.
MERS is a little-known clinical-radiological syndrome that can manifest with severe symptoms,6 but whose prognosis is usually favourable; the condition may be caused by a wide range of factors. Early diagnosis is essential to avoid unnecessary testing and treatments. Brain MRI is crucial to diagnosis.7
Please cite this article as: Gómez Iglesias P, López Valdés E, Vega Bayoll M, Gómez Ruíz MN. Encefalopatía con lesión reversible del cuerpo calloso: una entidad poco conocida con pronóstico favorable. Neurología. 2020;35:581–583.