Half and half syndrome is a rare oculomotor disorder characterised by unilateral internuclear ophthalmoplegia (INO) and ipsilateral sixth nerve palsy. Its name refers to the impairment of half of the contralateral gaze (secondary to INO, which limits adduction of the ipsilateral eye) and half of the ipsilateral gaze (secondary to a fascicular lesion to the abducens nerve, with no damage to the abducens nucleus, allowing normal contralateral eye adduction).1 This is an extremely rare INO plus syndrome, which may hinder differential diagnosis of other acute or subacute oculomotor disorders.
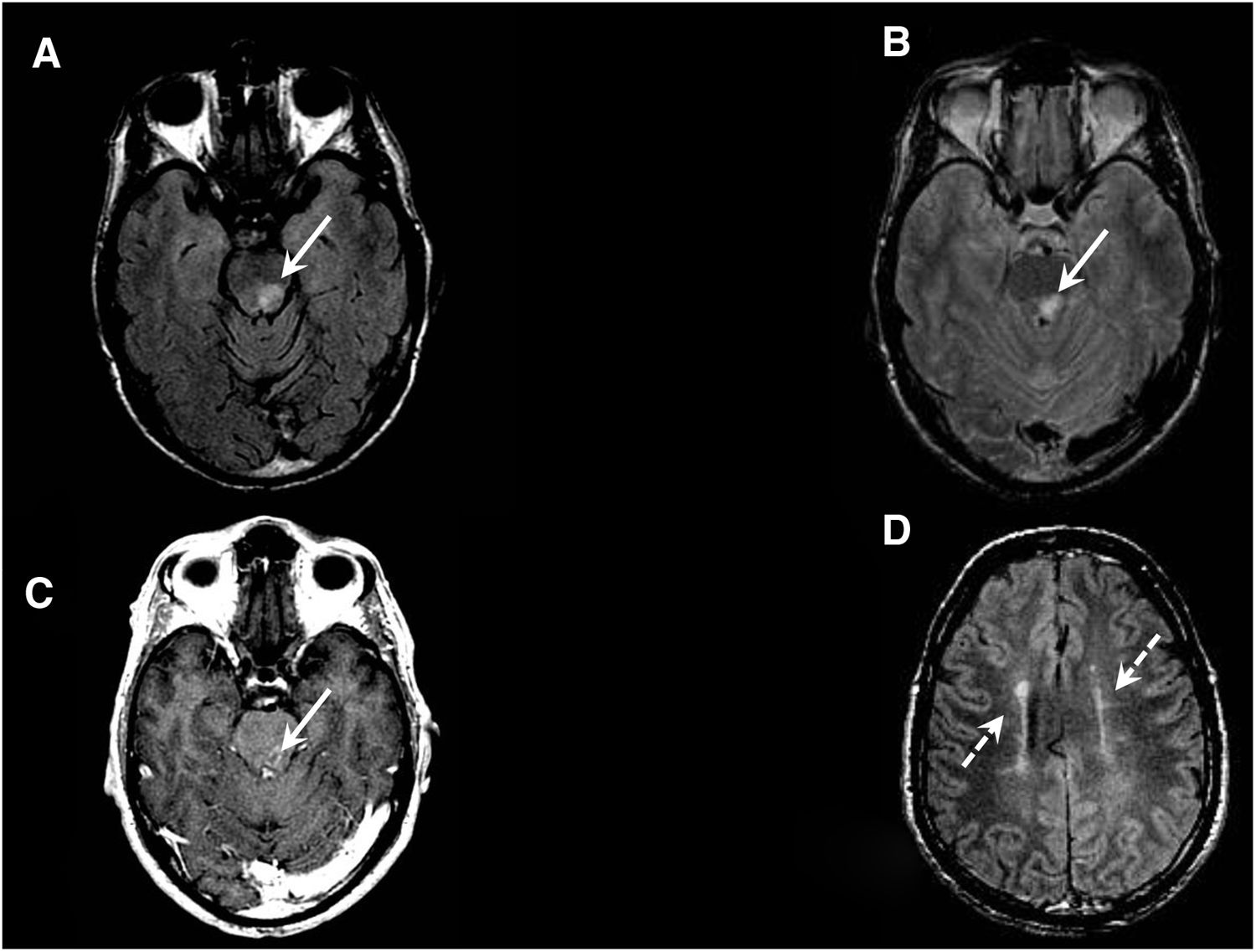
We present the case of a 47-year-old man with no relevant medical history who visited our hospital due to a 6-day history of progressive sensory impairment, right faciobrachial hemiparesis, and horizontal diplopia. The neurological examination revealed horizontal diplopia when looking to the left, with the false image being generated by the left eye; this finding is compatible with left sixth cranial nerve palsy. We also observed limited adduction of the left eye when looking to the right (with preserved convergence) and persistent horizontal-rotary nystagmus in the right eye (dissociated nystagmus), with reduced saccade velocity in the left eye when looking to the right. These findings are compatible with left INO. All complementary tests (complete blood count, CT scan, CT angiography, serology testing) yielded normal results. CSF analysis revealed a slightly elevated protein level (0.61 g/L) and no oligoclonal bands. T2-weighted brain MRI sequences revealed several hyperintense lesions to the periventricular white matter, genu of the corpus callosum, and left posterior parasagittal region of the pons; the latter region also displayed contrast uptake (Fig. 1). These lesions are suggestive of inflammation/demyelination; a spinal cord MRI scan revealed a central-dorsal lesion measuring 12 mm in length at the C2 level. The patient received corticosteroid therapy at standard doses for 4 days, showing good progression. He was diagnosed with half and half syndrome as the initial manifestation of multiple sclerosis, according to the 2017 McDonald criteria.2,3
Brain MRI scan (axial plane). A and B) FSE T2-FLAIR and FSE T2 sequences at the level of the orbital apex showing a focal lesion to the left posterior parasagittal region of the pons (solid arrows). C) 3D FSPGR T1 sequence after intravenous administration of single-dose contrast, revealing open ring contrast enhancement around the lesion (solid arrow); this is a frequent finding in inflammatory/demyelinating lesions. D) FSE T2 FLAIR sequence showing more than 3 lesions to the supratentorial periventricular white matter, distributed along an axis perpendicular to the lateral ventricles; these findings are also frequent in patients with inflammatory/demyelinating lesions (dashed arrows).
Vertical and horizontal gaze are controlled by the brainstem. The abducens nucleus is the final common pathway for conjugate horizontal eye movements; it is located in the dorsal pontine tegmentum and connects with the nucleus of the contralateral third cranial nerve via the medial longitudinal fasciculus (MLF). Lesions to the abducens nucleus can cause complete ipsilateral conjugate gaze palsy (ipsilateral abduction and contralateral adduction), whereas lesions to the medial longitudinal fasciculus only affect ipsilateral abduction. Convergence, controlled by the midbrain, is usually preserved.4,5
INO is the best known syndrome of the MLF,6 and is characterised by impaired adduction of the eye ipsilateral to the lesion and dissociated nystagmus in the contralateral abducting eye. Nystagmus is thought to be the result of an adaptive response to weakness of the medial rectus muscle ipsilateral to the INO (Hering law). The affected eye presents reduced saccadic velocity, predominantly in adduction. Oculocephalic reflexes were absent, which rules out the possibility of horizontal gaze pseudopalsy.
Several INO plus syndromes have been described, including one-and-a-half syndrome (lesion to the paramedian pontine reticular formation or the abducens nerve, associated with INO), wall-eyed bilateral INO (bilateral damage to the MLF), eight-and-a-half syndrome (one-and-a-half syndrome associated with seventh cranial nerve palsy), and half and half syndrome, which is extremely infrequent. The most common aetiologies are inflammatory (multiple sclerosis) in young patients and vascular in older individuals.7
Half and half syndrome is a rare combination of neurological signs. To our knowledge, this is the second reported case of half and half syndrome of inflammatory origin and the third reported case of the syndrome with any aetiology. This may partially be explained by underdiagnosis. As reported by Frohman et al.,6 clinicians may not detect mild or incomplete forms of the syndrome, manifesting as slowing of adduction saccades in the affected eye. Neuro-ophthalmological examination should include systematic assessment of smooth pursuit movements, saccades, the vestibulo-ocular reflex, and vergence movements; this increases diagnostic sensitivity for milder cases.
In conclusion, half and half syndrome should be included within the spectrum of INO and INO plus syndromes, which are frequent in multiple sclerosis, often presenting as the initial symptom; a high level of suspicion is therefore essential for early diagnosis.
Please cite this article as: Gómez Iglesias P, Sanesteban Beceiro E, Gómez Ruíz MN, Matías Guiu JA. Síndrome del medio y medio como presentación de esclerosis múltiple. Neurología. 2021;36:246–248.