Miller-Fisher syndrome (MFS) is a clinical variant of Guillain–Barré syndrome characterised by the triad of ophthalmoparesis, ataxia, and areflexia. Additionally, it is often associated with other symptoms secondary to cranial nerve weakness (facial paralysis, swallowing disorders, etc.), and even with sensory symptoms in the distal limbs.1
It is usually preceded by an infection, most typically a gastrointestinal infection caused by Campylobacter jejuni.2 Other triggers have been described, including vaccination, surgical procedures, etc.
Diagnosis tends not to be difficult when patients have the classic triad of symptoms, albumino-cytological dissociation, and neurophysiological findings. Further clues are provided by certain antibodies associated with these dysimmune neuropathies of the peripheral nervous system.3
At times, the presence of other associated symptoms, the absence of Anti-GQ1b, and lack of anomalous results on complementary tests during the acute phase of the syndrome may delay diagnosis and result in requests for unnecessary diagnostic tests.
We present the case of a 35-year-old man with no relevant personal history except for obesity. He experienced an episode of progressive-onset binocular diplopia and gait instability associated with a headache that had lasted 4 to 5 days. The patient reported having gone scuba diving before the onset of symptoms.
The neurological examination performed at the Emergency Department revealed bilateral eyelid ptosis, eyes remaining immobile in a neutral position, reactive bilateral mydriasis, bilateral but predominantly right-sided peripheral facial paralysis, weakness, bilateral elevation of the soft palate with no muscular atrophy or muscle tone alteration, universal areflexia, preserved sensitivity, and ataxic gait. During the hospital stay, he presented high blood pressure and required treatment with intravenous nitrates.
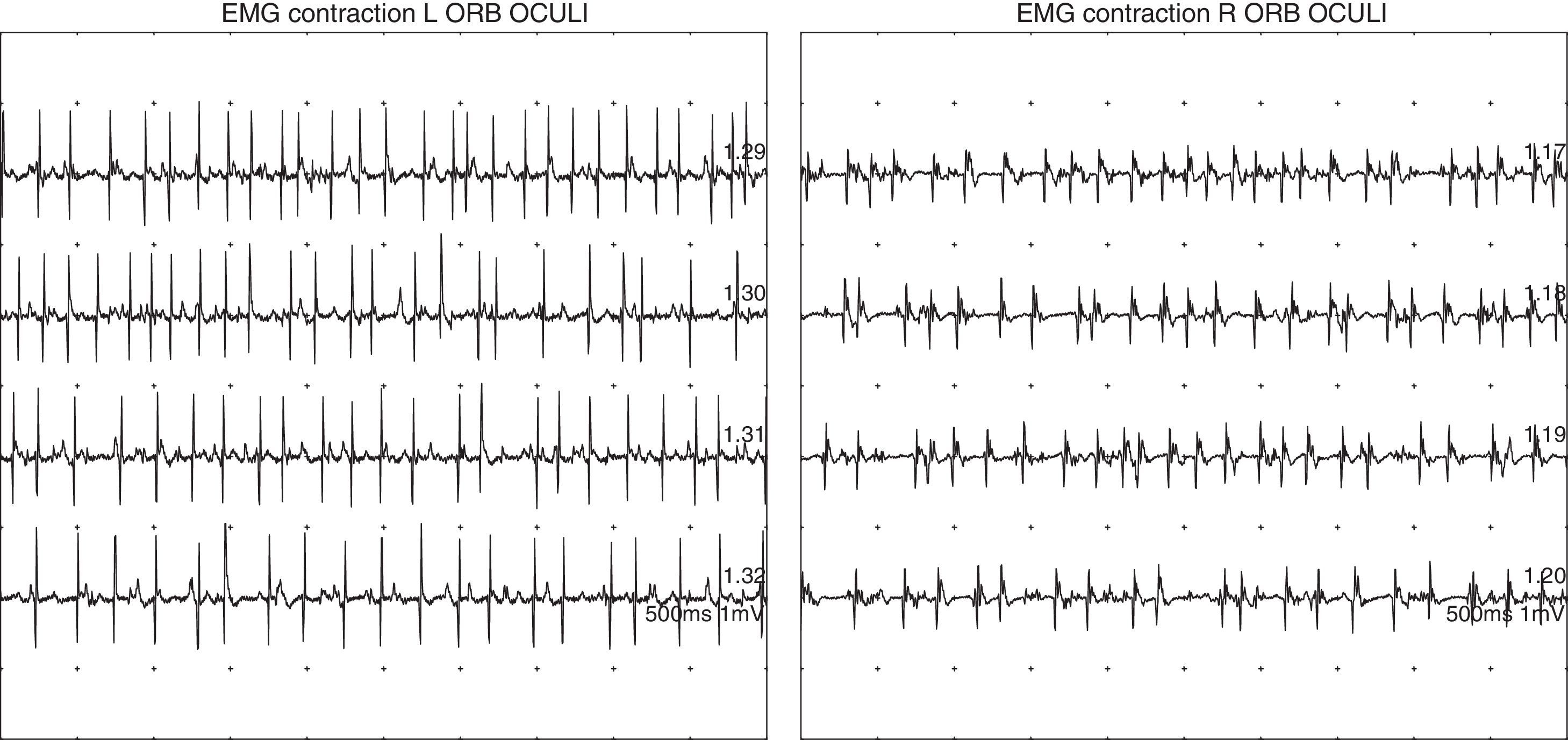
A complete complementary study was performed, including biochemical, immunology (Anti-GQ1b), tumour marker, folate, and cyanocobalamin tests. Results were negative or normal. Serology tests were normal, except for the test for C. jejuni antibodies, which delivered positive results. The CSF study showed albumino-cytological dissociation. Neuroimaging studies (including brain MRI), and intracranial vessel and cerebral blood flow studies all yielded normal results. The neurophysiological study during the acute phase revealed a decrease in M response amplitude in the bilateral facial nerve and abolished blink reflex. An EMG taken 15 days later showed severe demyelinating neuropathy with axonal damage in the facial nerve. While its latency was still high, the previously abolished palpebral reflex (blink reflex) could be observed (Fig. 1).
The patient was diagnosed with Miller-Fisher syndrome associated with C. jejuni.
The patient was treated with intravenous immunoglobulins (IGIV) during 5 consecutive days. His facial weakness initially increased to the point of becoming bilateral facial paralysis, but the condition began to subside slowly after a week. Throughout the course of the disease, he presented no swallowing/respiratory disorders or ECG abnormalities, although his diastolic blood pressure was high.
After 3 months, doctors observed clinical improvement and near-complete resolution of facial weakness. Diplopia and ocular motility resolved partially, and the patient experienced no gait abnormalities and no other associated symptoms.
Regarding the predisposing factors, the infection caused by C. jejuni is widely described in the scientific literature. After a long Medline search, however, we did not find any association between this disease and scuba diving, even if the nervous system is frequently affected by decompression problems and one of the divers’ most common symptom is headache.4 Although our case does not enable us to consider diving a predisposing factor, we do think that it could facilitate and probably cause other associated symptoms (headache) that were unclear upon initial diagnosis.
While non-reactive bilateral mydriasis is not usually present in MFS, neither is it uncommon. The symptom calls for differential diagnosis, especially in cases of botulism.5
Clinical data led us to order complementary studies of the central nervous system in order to rule out processes associated with diving, as well as other processes including cerebral venous sinus thrombosis. Another approach was to examine sociodemographic data, such as canned food consumption, in order to rule out the possibility of botulism, which would have been consistent with the marked cranial nerve involvement and the finding of mydriasis.
Despite the atypical symptoms and the negative result for Anti-GQ1b, findings that are present in more than 90% of MFS patients,6 results from the neurophysiological study during the acute phase helped us establish an early diagnosis and rapidly administer immunomodulatory therapy. In severe cases, this treatment is associated with better clinical progression and, consequently, with a better prognosis.
In general, neurophysiological findings during the acute phase of the disease have not been widely studied, and the subject remains controversial. The study by Calleja et al.7 assessed 5 patients who were diagnosed with MFS. Their results were similar to those from our patient, with a decrease in M response amplitude and abolished palpebral reflex.
In conclusion, we believe neurophysiological studies are necessary during the acute phase of polyneuropathies such as Miller-Fisher syndrome. Results will serve to support the suspected diagnosis from the beginning and unnecessary complementary studies may therefore be avoided.
Please cite this article as: Gabaldón Torres L, Badía Picazo C, Salas Felipe J. Papel del estudio neurofisiológico en el síndrome de Miller-Fisher. Neurología. 2013;28:451–452.