Dementia is a chronic, degenerative disease with a strong impact on families and health systems. The instruments currently in use for measuring cognitive impairment have different psychometric characteristics in terms of application time, cut-off point, reliability, and validity. The objective of this review is to describe the characteristics of the validated, Spanish-language versions of the Mini-Cog, Clock-Drawing Test, and Mini–Mental State Examination scales for cognitive impairment screening.
DevelopmentWe performed a three-stage literature search of articles published on Medline since 1953. We selected articles on validated, Spanish-language versions of the scales that included data on reliability, validity, sensitivity, and specificity.
ConclusionsThe 3 screening tools assessed in this article provide support for primary care professionals. Timely identification of mild cognitive impairment and dementia is crucial for the prognosis of these patients.
La demencia es una enfermedad crónica degenerativa de alto impacto para las familias y los sistemas de salud. Los instrumentos de medición del deterioro cognitivo que se utilizan actualmente tienen características psicométricas diferentes en cuanto a tiempo de aplicación, punto de corte, confiabilidad y validez. El objetivo de la presente revisión fue describir las características de las escalas Mini Cog, Prueba del Reloj y Mini Mental para tamizaje de deterioro cognitivo validadas al idioma español.
DesarrolloLa búsqueda bibliográfica se realizó en tres etapas mediante la base de datos Medline a partir del año 1953. Se realizó una selección de publicaciones validadas al español que incluyeran la confiabilidad, validez, sensibilidad y especificidad de las escalas.
ConclusionesLas tres herramientas de tamizaje descritas en este artículo proporcionan un apoyo para el personal de salud. La detección oportuna es crucial para el pronóstico de las personas que viven con deterioro cognitivo leve o demencia.
The growth forecast in the elderly population by 2050 will result in an increased demand for healthcare resources, particularly in primary care. Primary care staff constitute the first point of medical contact for elderly individuals with such cognitive disorders as mild cognitive impairment (MCI) and dementia. In Mexico, MCI and dementia have a prevalence of 7.3% and 7.9%, respectively; the prevalence of these conditions is age-dependent.1 This has led to the creation of international organisations that aim, with the support of the World Health Organization, to promote the development of national strategies and specific actions, such as early detection of Alzheimer disease (AD) and other dementias, in a wide range of countries, including Mexico.
MCI is considered an intermediate stage between normal cognitive function and mild dementia.2 From a biological viewpoint, disease progression may be delayed or even halted if measures are taken in the 5–10 years before diagnosis of MCI,3 that is before the activation of mechanisms that lead to neuronal death. Neuronal death causes cognitive symptoms, which are not easily identified by patients or their caregivers as they tend to be interpreted as normal signs of ageing.4
At present, preserving cognitive function and independence in elderly individuals requires early diagnosis of cognitive impairment using neuropsychological tests.5 The cognitive screening tools currently used in Spanish-speaking populations differ in terms of administration times, cut-off points, reliability, and validity. However, not all these parameters have been critically reviewed. Our study describes the characteristics of the Mini-Cog, the Clock-Drawing Test, and the Spanish-language version of the Mini–Mental State Examination (MMSE) to screen for cognitive impairment.
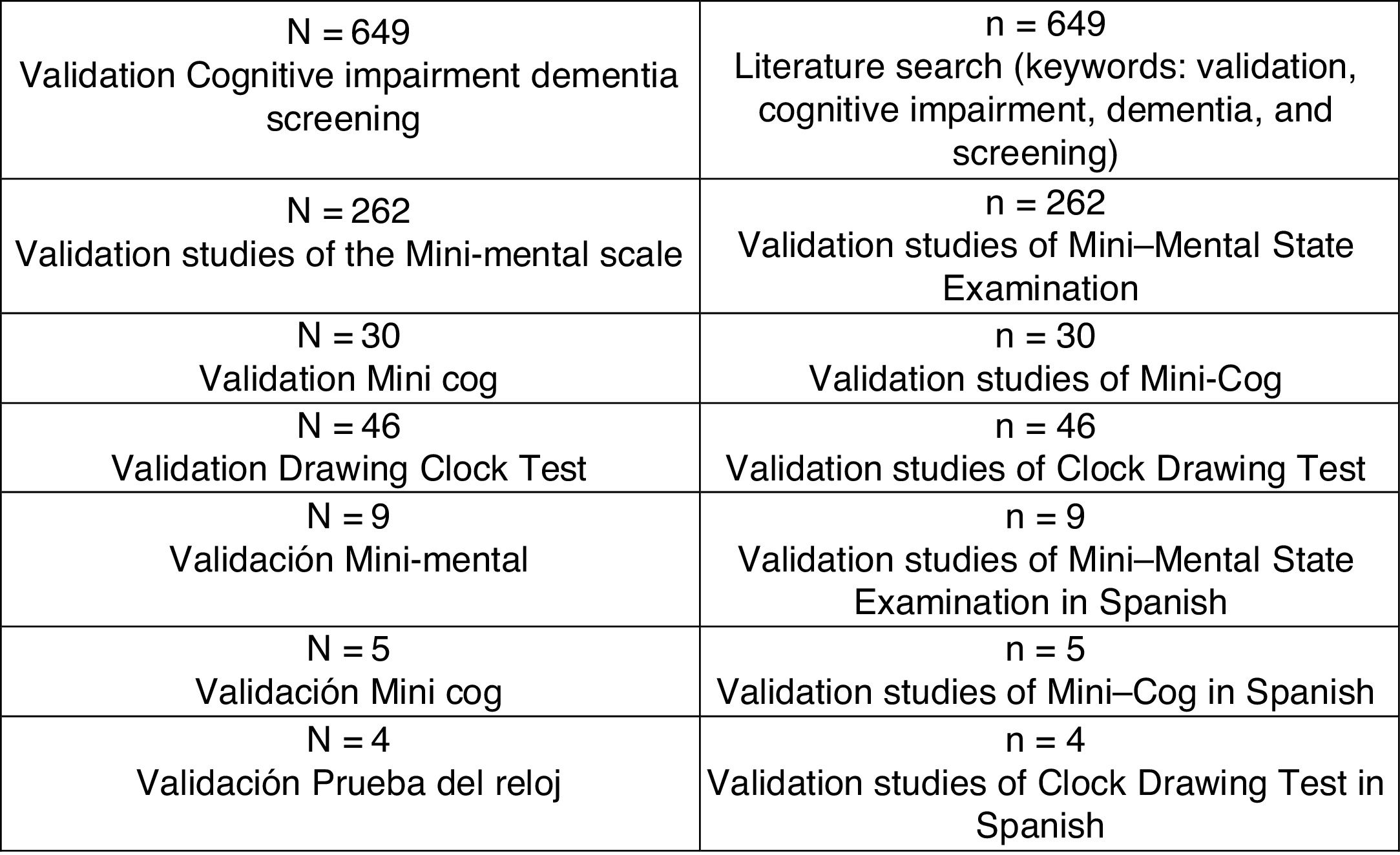
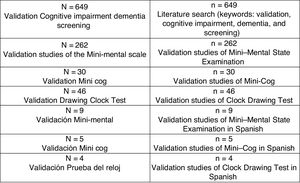
DevelopmentWe conducted a bibliographic search on Medline to gather articles published since 1953, using the keywords validation, cognitive impairment, dementia, and screening. Our search yielded 649 articles from different countries, mainly from Asia, Europe, and America, validating more than 8 cognitive scales for different types of dementia. We selected the scales relevant to our study, identifying 262 articles on the MMSE, 30 on the Mini-Cog, and 46 on the Clock-Drawing Test. Finally, we selected articles written in Spanish and addressing the typical factors of validation studies (reliability, validity, sensitivity, and specificity): 9 articles on the MMSE, 5 on the Clock-Drawing Test, and 4 on the Mini-Cog (Fig. 1). These tools have been validated in several Spanish-speaking countries as they are easy and quick to administer in primary care.
Mini–Mental State examinationThe MMSE was developed by Folstein6 in 1975 to screen for cognitive impairment in hospitalised patients. This test, and various modified versions,7 constitutes the most widely used cognitive screening tool in clinical practice and epidemiological studies due to its brevity and ease of use. It is widely recommended to support diagnosis of such cognitive disorders as AD, Parkinson’s disease, and other types of dementia.8
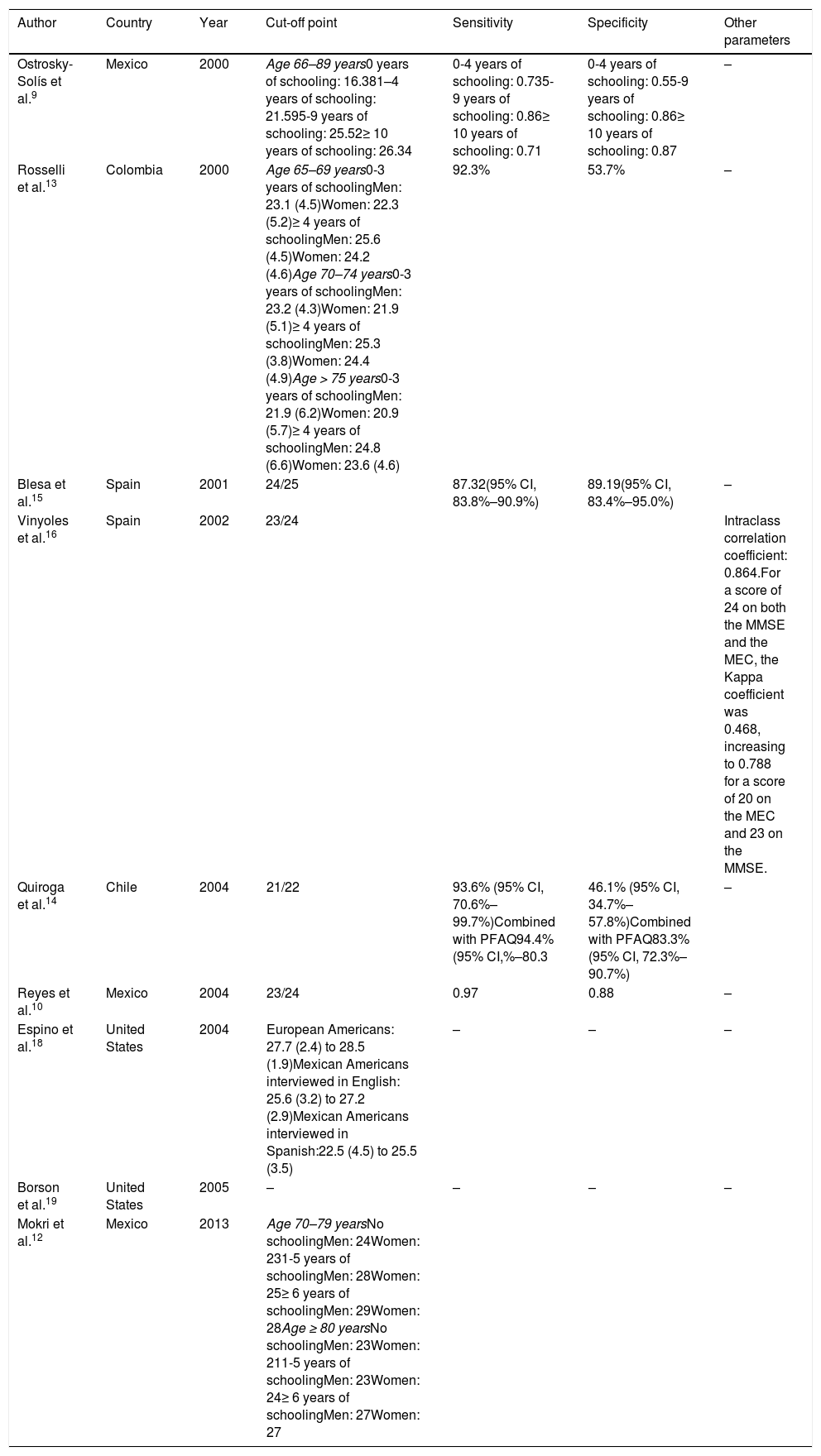
The scale includes 11 items and has a maximum score of 30. The cut-off point was originally set at 24, although it has been argued that the cut-off point is affected by age, socioeconomic status, ethnicity, and education level (Table 1). In Mexico in 2000, Ostrosky-Solís et al.9 administered the Spanish-language version of the MMSE to 430 individuals aged 16–50, 51–65, and 66–89, and to a group of 40 patients with dementia, and detected education-related changes in sensitivity and specificity (Table 1). Patients with severe dementia and individuals with no schooling achieved similar total scores, whereas individuals with 1–4 years of schooling performed similarly to patients with mild dementia. The authors conclude that modifying the cut-off point is not sufficient to obtain adequate levels of sensitivity and specificity, and suggested that the MMSE is useful to confirm presence of severe cognitive impairment in individuals with more than 5 years of schooling.
Validation studies for the Mini–Mental State Examination.
| Author | Country | Year | Cut-off point | Sensitivity | Specificity | Other parameters | ||
|---|---|---|---|---|---|---|---|---|
| Ostrosky-Solís et al.9 | Mexico | 2000 | Age 66–89 years0 years of schooling: 16.381–4 years of schooling: 21.595-9 years of schooling: 25.52≥ 10 years of schooling: 26.34 | 0-4 years of schooling: 0.735-9 years of schooling: 0.86≥ 10 years of schooling: 0.71 | 0-4 years of schooling: 0.55-9 years of schooling: 0.86≥ 10 years of schooling: 0.87 | – | ||
| Rosselli et al.13 | Colombia | 2000 | Age 65–69 years0-3 years of schoolingMen: 23.1 (4.5)Women: 22.3 (5.2)≥ 4 years of schoolingMen: 25.6 (4.5)Women: 24.2 (4.6)Age 70–74 years0-3 years of schoolingMen: 23.2 (4.3)Women: 21.9 (5.1)≥ 4 years of schoolingMen: 25.3 (3.8)Women: 24.4 (4.9)Age > 75 years0-3 years of schoolingMen: 21.9 (6.2)Women: 20.9 (5.7)≥ 4 years of schoolingMen: 24.8 (6.6)Women: 23.6 (4.6) | 92.3% | 53.7% | – | ||
| Blesa et al.15 | Spain | 2001 | 24/25 | 87.32(95% CI, 83.8%–90.9%) | 89.19(95% CI, 83.4%–95.0%) | – | ||
| Vinyoles et al.16 | Spain | 2002 | 23/24 | Intraclass correlation coefficient: 0.864.For a score of 24 on both the MMSE and the MEC, the Kappa coefficient was 0.468, increasing to 0.788 for a score of 20 on the MEC and 23 on the MMSE. | ||||
| Quiroga et al.14 | Chile | 2004 | 21/22 | 93.6% (95% CI, 70.6%–99.7%)Combined with PFAQ94.4% (95% CI,%–80.3 | 46.1% (95% CI, 34.7%–57.8%)Combined with PFAQ83.3% (95% CI, 72.3%–90.7%) | – | ||
| Reyes et al.10 | Mexico | 2004 | 23/24 | 0.97 | 0.88 | – | ||
| Espino et al.18 | United States | 2004 | European Americans: 27.7 (2.4) to 28.5 (1.9)Mexican Americans interviewed in English: 25.6 (3.2) to 27.2 (2.9)Mexican Americans interviewed in Spanish:22.5 (4.5) to 25.5 (3.5) | – | – | – | ||
| Borson et al.19 | United States | 2005 | – | – | – | – | ||
| Mokri et al.12 | Mexico | 2013 | Age 70–79 yearsNo schoolingMen: 24Women: 231-5 years of schoolingMen: 28Women: 25≥ 6 years of schoolingMen: 29Women: 28Age ≥ 80 yearsNo schoolingMen: 23Women: 211-5 years of schoolingMen: 23Women: 24≥ 6 years of schoolingMen: 27Women: 27 | |||||
MEC: Mini–Examen Cognoscitivo; MMSE: Mini–Mental State Examination; PFAQ: Pfeffer Functional Activities Questionnaire.
In 2004, Reyes et al.10 validated a modified, Spanish-language version of the MMSE in a sample of 203 elderly individuals registered with the Mexican Institute of Social Security. The authors report an optimal cut-off point of 23/24, with sensitivity of 0.97 and specificity of 0.88. The authors concluded that 60.6% of the variance was explained by the variables orientation in space, orientation in time, language plus attention and calculation, and naming objects.
In a 2010 study on an elderly Mexican population by Franco-Marina et al.,11 ceiling and floor effects were still observed after adjusting scores for level of schooling. They concluded that additional tests should be used to rule out MCI when using an education-adjusted MMSE.
In 2013, Mokri et al.12 published normative scores for the Spanish-language versions of 3 neuropsychological tests: the MMSE, the Free and Cued Selective Reminding Test, and the Isaacs Set Test. They included a sample of 1047 elderly Mexican patients from the Coyoacán cohort study. The lowest cut-off points were established for the group of illiterate participants, both in men (24) and in women (23); the cut-off point was even lower in illiterate women aged over 80 years (21). The highest cut-off points were obtained for individuals with more than 6 years of schooling, both in men (29) and in women (28); this cut-off point was lower for individuals aged over 80 years (27). The authors concluded that MMSE cut-off points vary according to age, sex, and education level.
In Colombia, Rosselli et al.13 administered the Spanish-language version of the MMSE to a population including a high percentage of illiterate individuals; the sample was drawn from EPINEURO, a nation-wide neuroepidemiological study conducted in Colombia. The study reports 92.3% sensitivity and 53.7% specificity. These findings support the hypothesis that education level has a major impact on MMSE scores, to an even greater degree than age. The correlation between total score and education level was nearly 3 times greater (0.34) than that observed between total score and age (–0.13). The authors conclude that the MMSE is useful for individuals with a high level of schooling and for detecting severe cognitive impairment, but should not be used to evaluate individuals with a low education level or MCI.
In Chile in 2004, Quiroga et al.14 conducted a validation study of a dementia screening battery including the MMSE and the Pfeffer Functional Activities Questionnaire in a sample of 100 elderly individuals. The combination of both tests achieved greater sensitivity and specificity (94.4% and 83.3%, respectively) than the MMSE alone (93.6% and 46.1%). The authors concluded that the combination of both tools had good sensitivity and specificity for dementia screening in the Chilean population and that education level has a major impact on MMSE scores in individuals without dementia.
In Spain, Blesa et al.15 adapted the MMSE to Spanish using a sample of 111 patients with Alzheimer-type dementia, 86 with MCI, and 253 controls, and found an optimal cut-off point of 24/25, with 87.32% sensitivity and 89.19% specificity; scores require adjustment for age and education level, however.
Vinyoles et al.16 evaluated the degree of concordance between the MMSE and the adapted Spanish-language version, the Mini–Examen Cognoscitivo in 3167 individuals aged over 65 years, reporting an intraclass correlation coefficient of 0.864 and a kappa coefficient of 0.788 for both tests for a cut-off score of 20 in the Mini–Examen Cognoscitivo and 23 in the MMSE; the authors suggest that the test should not be used in individuals older than 80 and/or with a low education level.
In North America, Borson et al.17 compared the Mini-Cog against the MMSE, and found that the former had greater accuracy for detecting dementia (83%, vs 81% for the MMSE), even in individuals with very low education levels, and was easier to administer to non–English speakers.
In the context of the San Antonio Longitudinal Study of Aging, Espino et al.18 report the cut-off points for the MMSE in 3 socioculturally distinct neighbourhoods in San Antonio, Texas, with different education levels; mean scores (SD) ranged from 27.7 (2.4) to 28.5 (1.9) for European Americans, from 25.6 (3.2) to 27.2 (2.9) for Mexican Americans interviewed in English, and from 22.5 (4.5) to 25.5 (3.5) for Mexican Americans interviewed in Spanish. These results suggest that healthcare professionals in the United States should be aware of the possibility of false positives in highly educated English-speaking elderly individuals.
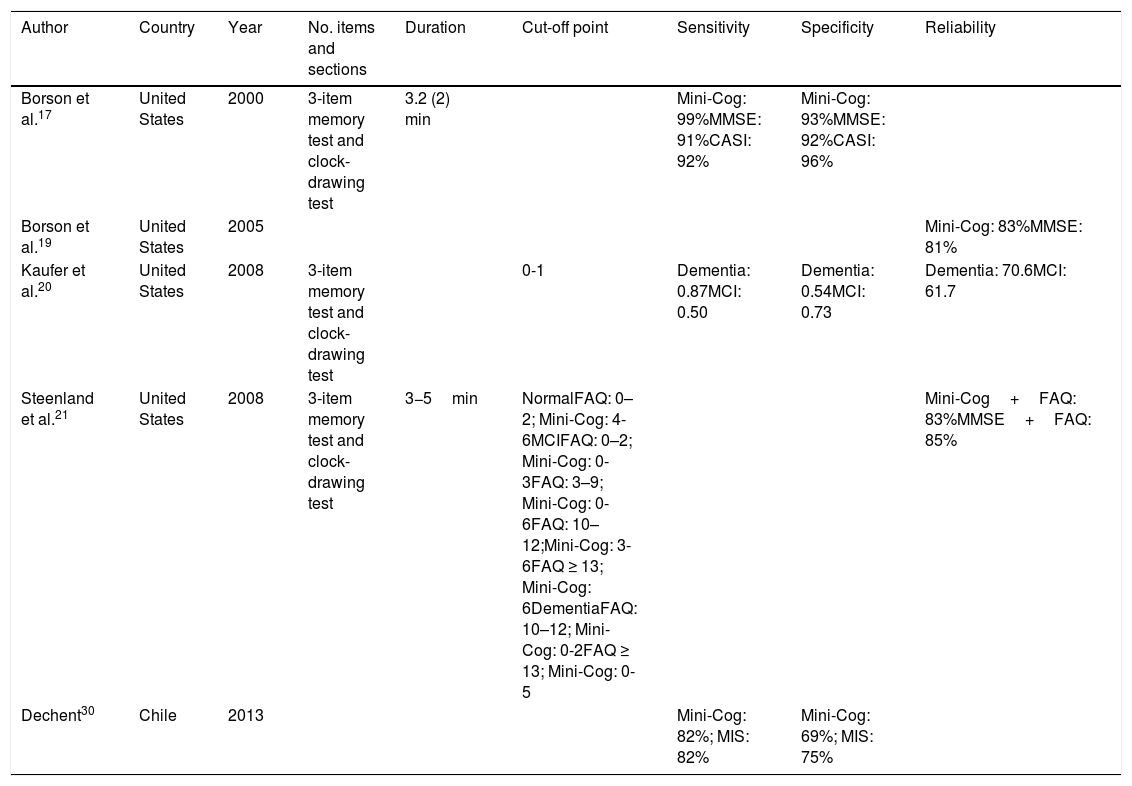
Mini-CogTable 2 shows the different validation studies of the Mini-Cog. This screening tool for dementia is quick to administer (less than 5min) and has 2 sections: the first section is a 3-word memory test and the second is a clock-drawing task. The Mini-Cog was introduced in the United States by Borson17 in 2000, with a sample of 249 elderly individuals from different language communities. The test showed greater sensitivity (99%) and specificity (93%) than the MMSE (91% and 92%, respectively) for identifying patients with moderate dementia. Furthermore, the Mini-Cog showed greater screening accuracy than the MMSE (83% vs 81%), even in individuals with very low levels of schooling, and has been shown to be easy to administer to non–English speakers.19 According to a 2008 study by Kaufer et al.,20 the Mini-Cog has high sensitivity for screening for dementia but low sensitivity and specificity (0.50 and 0.73, respectively) for screening for MCI (Table 2).
Validation studies for the Mini-Cog.
| Author | Country | Year | No. items and sections | Duration | Cut-off point | Sensitivity | Specificity | Reliability |
|---|---|---|---|---|---|---|---|---|
| Borson et al.17 | United States | 2000 | 3-item memory test and clock-drawing test | 3.2 (2) min | Mini-Cog: 99%MMSE: 91%CASI: 92% | Mini-Cog: 93%MMSE: 92%CASI: 96% | ||
| Borson et al.19 | United States | 2005 | Mini-Cog: 83%MMSE: 81% | |||||
| Kaufer et al.20 | United States | 2008 | 3-item memory test and clock-drawing test | 0-1 | Dementia: 0.87MCI: 0.50 | Dementia: 0.54MCI: 0.73 | Dementia: 70.6MCI: 61.7 | |
| Steenland et al.21 | United States | 2008 | 3-item memory test and clock-drawing test | 3−5min | NormalFAQ: 0–2; Mini-Cog: 4-6MCIFAQ: 0–2; Mini-Cog: 0-3FAQ: 3–9; Mini-Cog: 0-6FAQ: 10–12;Mini-Cog: 3-6FAQ ≥ 13; Mini-Cog: 6DementiaFAQ: 10–12; Mini-Cog: 0-2FAQ ≥ 13; Mini-Cog: 0-5 | Mini-Cog+FAQ: 83%MMSE+FAQ: 85% | ||
| Dechent30 | Chile | 2013 | Mini-Cog: 82%; MIS: 82% | Mini-Cog: 69%; MIS: 75% |
CASI: Cognitive Abilities Screening Instrument; FAQ: Functional Activities Questionnaire; MCI: mild cognitive impairment; MIS: Memory Impairment Screen; MMSE: Mini–Mental State Examination.
Furthermore, the combination of the Mini-Cog and the Functional Activities Questionnaire identifies individuals with dementia or cognitive impairment with 83% accuracy, compared to 85% for the combination of the MMSE and the Functional Activities Questionnaire, with the latter combination taking twice or 3 times as long to administer as the Mini-Cog.
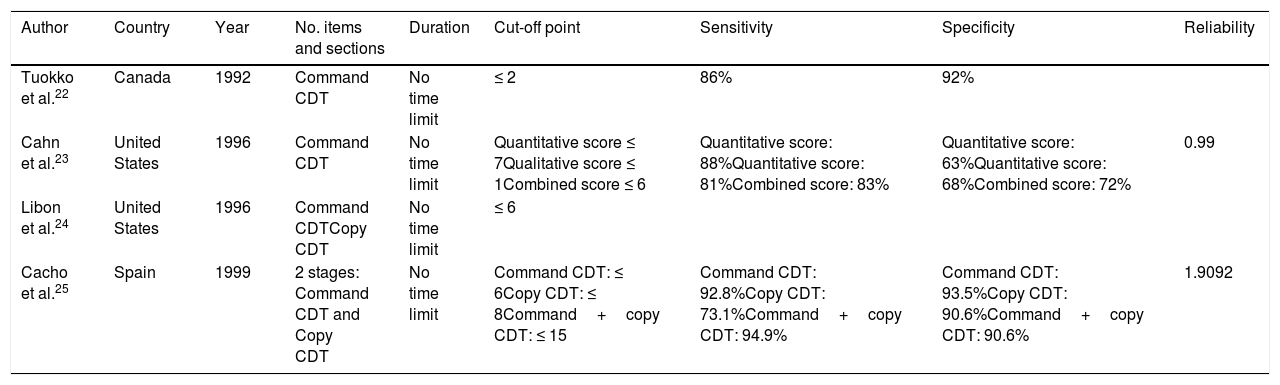
Clock-Drawing testTable 3 lists the studies validating the Clock-Drawing Test, which was created in 1953. This test is easy to administer, and requires the examinee to draw a clock from memory. Scores discriminate between patients with and without dementia. In 1992, Tuokko et al.22 administered the Clock-Drawing Test to a sample of patients with probable AD. The maximum score was set at 31 points, with a cut-off point of 2 drawing errors (errors in 2 or more components) achieving 92% specificity and 86% sensitivity for discriminating between healthy individuals and individuals with AD.
Validation studies for the Clock-Drawing Test.
| Author | Country | Year | No. items and sections | Duration | Cut-off point | Sensitivity | Specificity | Reliability |
|---|---|---|---|---|---|---|---|---|
| Tuokko et al.22 | Canada | 1992 | Command CDT | No time limit | ≤ 2 | 86% | 92% | |
| Cahn et al.23 | United States | 1996 | Command CDT | No time limit | Quantitative score ≤ 7Qualitative score ≤ 1Combined score ≤ 6 | Quantitative score: 88%Quantitative score: 81%Combined score: 83% | Quantitative score: 63%Quantitative score: 68%Combined score: 72% | 0.99 |
| Libon et al.24 | United States | 1996 | Command CDTCopy CDT | No time limit | ≤ 6 | |||
| Cacho et al.25 | Spain | 1999 | 2 stages: Command CDT and Copy CDT | No time limit | Command CDT: ≤ 6Copy CDT: ≤ 8Command+copy CDT: ≤ 15 | Command CDT: 92.8%Copy CDT: 73.1%Command+copy CDT: 94.9% | Command CDT: 93.5%Copy CDT: 90.6%Command+copy CDT: 90.6% | 1.9092 |
CDT: Clock-Drawing Test.
In 1996, Cahn et al.23 examined the diagnostic accuracy of the Clock-Drawing Test for detecting dementia in individuals without significant functional limitations in the general population of the United States. A cut-off point of ≤ 7 for quantitative scores showed 88% sensitivity and 63% specificity, whereas a cut-off point of ≤ 1 for qualitative scores showed 81% sensitivity and 68% specificity. For the global score, a cut-off point of ≤ 6 achieved 83% sensitivity and 72% specificity.
In 1996, Libon et al.24 developed a scoring system for tallying errors in order to study the potential neuropsychological deficits explaining why patients with vascular dementia perform more poorly on the Clock-Drawing Test than those with AD. The researchers used 2 different scoring systems: the first is scored from 1 (worst performance) to 10 (best performance), and the second sums all errors made in the drawing and/or placement of the clock’s face, hands, and numbers. This second scoring system evaluates 10 types of errors, each of which is scored either 1 (present) or 0 (absent). The authors conclude that their adaptation of the scoring system and the analysis of error types are useful for quantifying test performance in patients with AD and vascular dementia, and help to distinguish between both clinical profiles, particularly when cerebrovascular alterations are predominantly subcortical.
ConclusionsThis review addresses the main characteristics of 3 widely used cognitive screening tests (MMSE, Mini-Cog, and Clock-Drawing Test) that have been validated to Spanish; the psychometric properties and administration of these tests have several strengths and limitations.
The Clock-Drawing Test was the first tool to be validated to Spanish, in the 1990s, followed by the MMSE and the Mini-Cog in 2000. The Clock-Drawing Test has been validated to Spanish in Canada, the United States, and Spain; the MMSE in Mexico, Colombia, Spain, Chile, and the United States, and the Mini-Cog in the United States and Chile.
The MMSE, the most popular cognitive screening tool, has been validated in numerous research studies. However, its main limitations include the fact that it depends on social and education variables, the lack of standardisation, and the administration time, which makes the test difficult to administer in primary care.26,27
Although the Mini-Cog is quicker to administer and has shown higher sensitivity, specificity, and accuracy than the MMSE, it may not be suitable for patients with low education levels.28,29
A wide range of tools have been developed to screen for cognitive impairment and dementia. Our review focuses on the validated Spanish-language versions of 3 screening tools used in clinical practice. Practical, reliable instruments are needed for application by primary care professionals, since early diagnosis is essential to improving outcomes for patients with MCI and dementia.
Selecting the most appropriate screening tools and training primary care physicians to detect cognitive disorders constitutes a major public health challenge.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank all professionals who supported our research at the National Institute of Geriatrics, in Mexico City.
Please cite this article as: Torres-Castro S et al. Escalas de tamizaje cognitivo en habla hispana: una revisión crítica. Neurología. 2022;37:53–60.