Retrochiasmatic lesions of the optic tract usually result in contralateral homonymous hemianopsia; the main cause of these lesions is brain disease, particularly in the occipital region. The nasal retinal fibres are represented on the anterior part of the visual cortex. As this representation is unilateral, retrochiasmatic lesions in this region can cause atypical visual alterations.
Clinical caseOur patient was a 69-year-old man with a history of deep vein thrombosis and thrombophilia, receiving treatment with acenocoumarol. He attended the emergency department due to a 6-hour history of left-sided far peripheral vision loss associated with mild headache. The patient reported no nausea or vomiting.
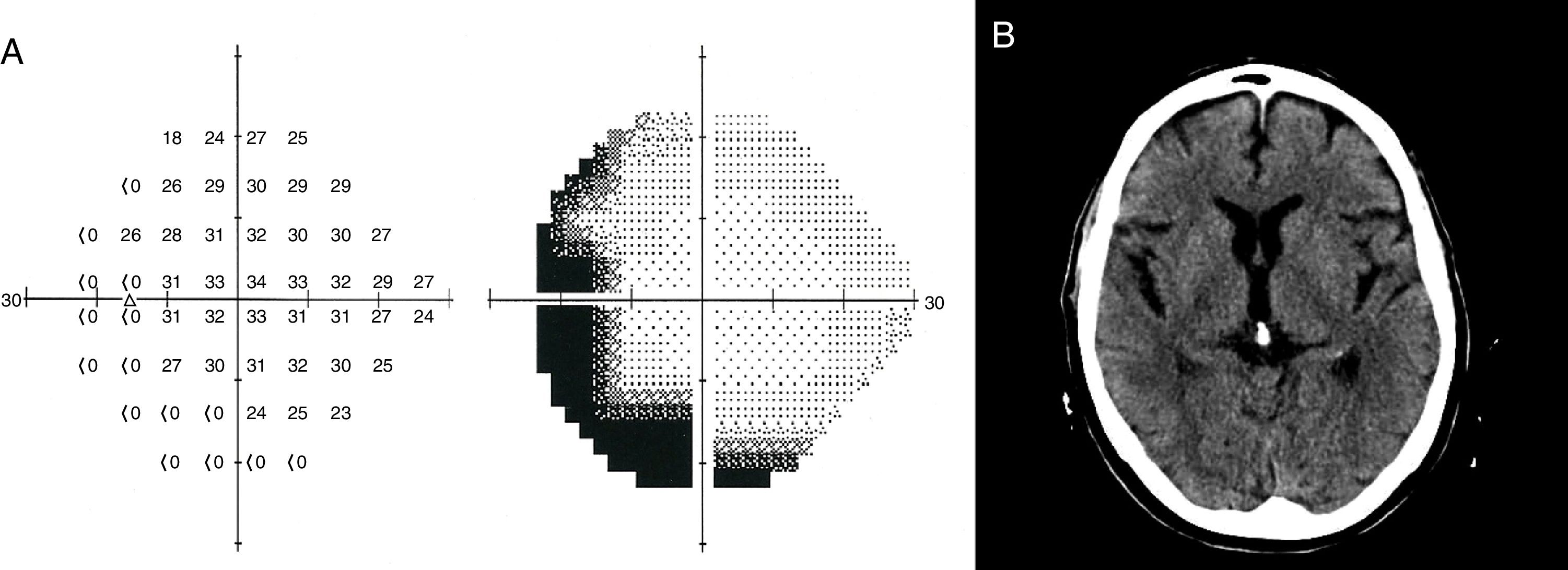
The physical examination revealed normal visual acuity, preserved pupillary light reflex, and no eye fundus alterations. Perimetry revealed incomplete hemianopsia in the left eye only. The patient did not present motor or sensory alterations, and displayed an extensor plantar response in the left foot. The Humphrey visual field test revealed a left-sided crescent-shaped temporal visual field defect (Fig. 1A).
A brain CT scan (Fig. 1B), electrocardiogram, and transcranial and supra-aortic trunk Doppler ultrasound revealed no abnormalities. Electroencephalography (EEG) findings were normal. International Normalised Ratio (INR) was below the therapeutic range (1.9). Brain MRI was not performed during the symptomatic phase as MRI equipment is not available at our centre's emergency department.
The patient's condition gradually improved, with symptoms resolving fully by the following day; this improvement was in line with the normalisation of the patient's INR. A brain MRI scan performed the following day revealed no alterations.
We discharged the patient with a diagnosis of temporal crescent syndrome secondary to transient ischaemic attack, in the light of the sudden onset of symptoms, coinciding with the subtherapeutic INR value and improving as INR normalised, as well as the presence of cardiovascular risk factors, and having ruled out other possible diagnoses: migraine with aura (absence of personal or family history of migraine), epileptic seizure (long duration of symptoms; normal EEG readings), optic neuritis (absence of central and/or centrocecal visual field defects; sudden onset and transient nature of symptoms), and retinal detachment (normal eye fundus).
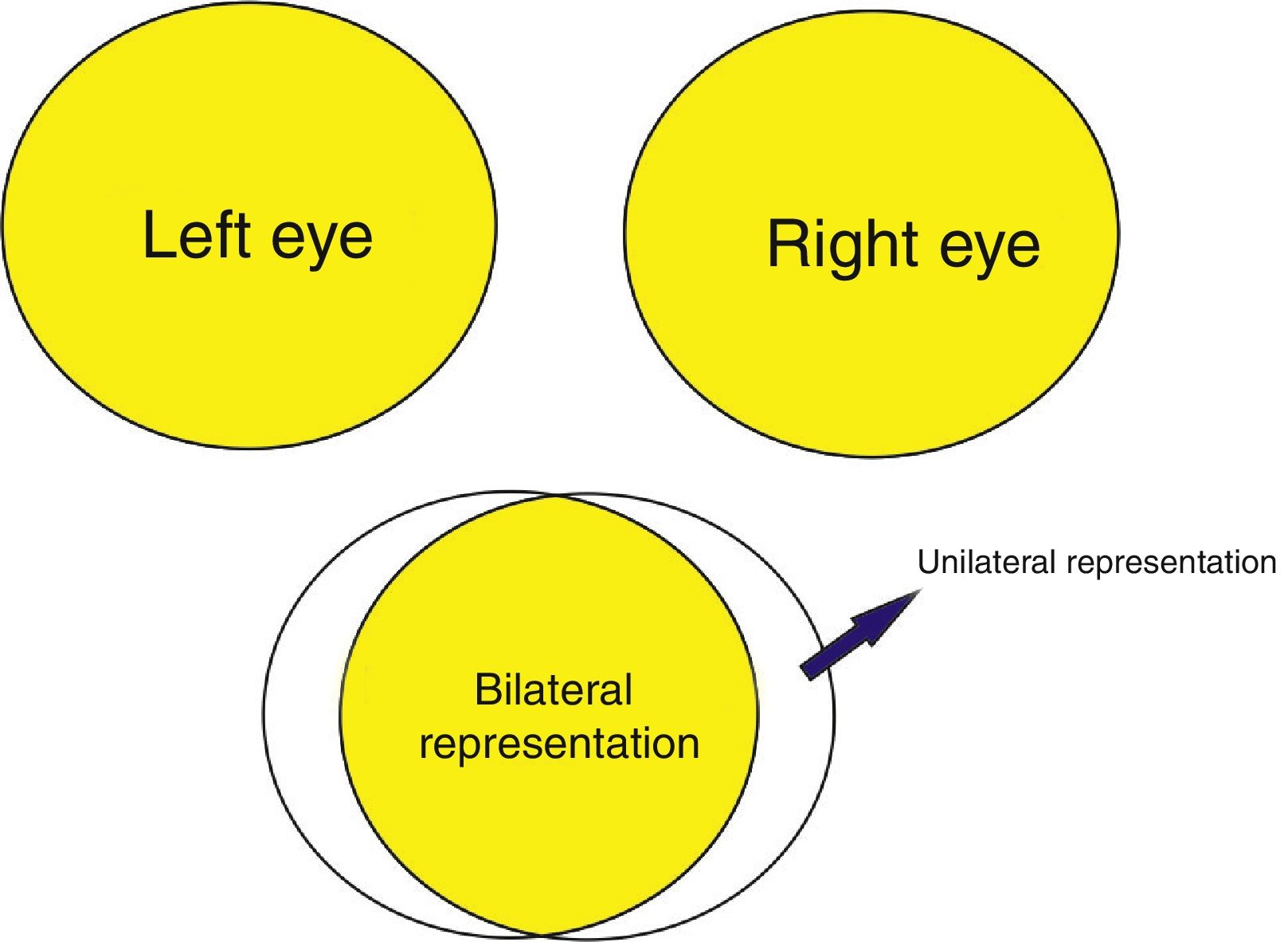
DiscussionTemporal crescent syndrome is an atypical visual field alteration comprising monocular vision loss in the temporal field.1 Retrochiasmatic lesions generally cause homonymous visual field defects. The exception to this rule is temporal crescent syndrome, which is caused by a lesion to the anterior region of the contralateral visual cortex.2,3 The visual field usually extends 60° nasally and 100° temporally. Therefore, 40° of the temporal peripheral vision is represented unilaterally in the visual cortex, on the contralateral side (Fig. 2). The syndrome may also be caused by lesions to the Meyer loop (anterior temporal lobe)4 or anterior areas of the primary visual cortex, just posterior to the splenium of the corpus callosum, on the medial surface of the occipital lobes.
Differential diagnosis of temporal crescent syndrome should consider migraine with aura, which can be differentiated by symptoms of headache; visual auras (typically scintillating scotoma); hypersensitivity to light, sound, and smell; nausea; and occasionally vomiting. Ischaemic optic neuritis is differentiated by altitudinal visual field defects. Patients with retinal detachment display eye fundus abnormalities and diminished visual acuity in addition to the visual field loss. Retrobulbar neuritis is differentiated by reduced visual acuity, more central visual field loss, alterations in colour perception, and retro-orbital pain.
Retrochiasmatic lesions may cause such other atypical visual alterations as quadruple sectoranopia,5 a wedge-shaped visual field defect caused by lesions to the medial and lateral areas of the lateral geniculate nuclei (irrigated by the anterior choroidal artery). Horizontal sectoranopia results from a lesion to the hilum, which is irrigated by the lateral choroidal artery.