Collet-Sicard syndrome caused by trauma is rare.1 Vocal cord paralysis (VCP), difficulty swallowing, loss of taste in the posterior third of the tongue, tongue muscle and sternocleidomastoid muscle atrophy and paralysis are the typical clinical manifestations.2 The patient complains to the doctor only about hoarseness and difficulty swallowing. They will ignore the change in taste and muscle. So some doctors misdiagnose it as simple VCP.
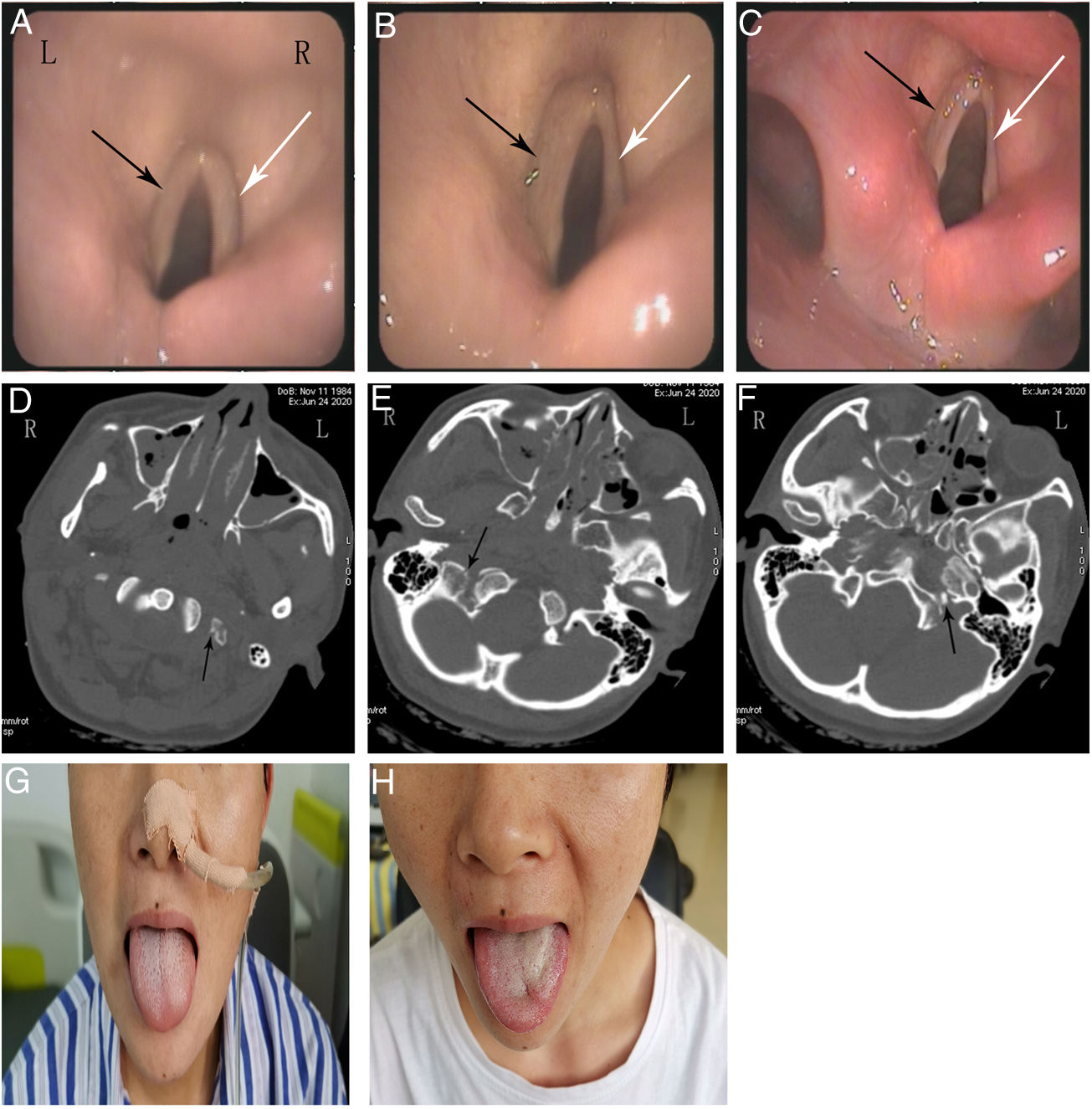
The female patient is 35 years old. The patient was unconscious when she fell from a height of 9 meters on June 24, 2020. The Glasgow Coma Scale score was 8/15 (E2, V1, M5). Computed tomography (CT) showed that occipital fractures on both sides and fractures of left transverse process of atlas. She underwent tracheal intubation twice because she removed the tube by herself. Her consciousness was clear and removed the tube on June 26. She was dysphonic, difficulty swallowing and given a nasogastric tube after swallowing assessment. Neurotrophic therapy was applied when the damage of laryngeal nerve was considered. She accepted swallowing rehabilitation and acupuncture treatment. The electronic fiber laryngoscope (EFL) showed complete bilateral vocal cord paralysis on July 23 (Fig. 1A). The hoarseness of the patient began to improve significantly on July 29. We found the tongue of patient was tilted to the left and the posterior third of the tongue had decreased taste on July 30. The EFL indicated that the right vocal cord was normal, and the left vocal cord was still completely paralyzed on August 21 (Fig. 1B). The patient passed the swallowing assessment successfully and the nasogastric tube was removed on August 28. One month later, the patient still had a hoarse voice, decreased taste, and a crooked tongue. The difficulty swallowing was disappeared. The EFL still showed complete paralysis of the left vocal cord (Fig. 1C).
The electronic fiber laryngoscope shows that the bilateral vocal cords were fixed and the glottis could not move on July 23 (A). The left vocal cord (black arrow) was fixed and the right vocal cord (white arrow) was normal on August 21. There was a gap when the bilateral vocal cords closed (B). The left vocal cord (black arrow) was still fixed on September 21 (C). The computed tomography showed that the fracture of the left transverse process of the atlas and right skull base was mild (D, E). Bone fragments were found in the left occiput (F). The tongue tilted to the left on July 30 (G). The muscles of the left tongue were atrophy, and the tongue deviated to the left side on September 21 (H).
The most common cause of Collet-Sicard syndrome is tumor metastasis of skull base, followed by vascular disease and trauma.3 Collet-Sicard syndrome caused by skull base fracture had only been reported 8 times in English literature. The cranial nerves IX–XII near the jugular foramen are damaged when the skull base fractured.3 Some scholars speculated that the pathogenesis was nerve edema or bone fragments directly compressing the nerve.4,5 Since hoarseness and difficulty swallowing are the main symptoms, it is easy for doctors to misdiagnose it as simple VCP. Symptoms of VCP are hoarseness, difficulty swallowing and difficulty breathing.6 Both tracheal intubation and trauma can cause VCP. Arytenoid dislocation or recurrent laryngeal nerve damage is the main cause of VCP after tracheal intubation.7 EFL can be used to observe arytenoid cartilage to determine whether it is dislocated. In this case, the patient received tracheal intubations twice in a coma. So the tracheal intubation was first considered as the cause of VCP. The anesthesiologist reported that the tracheal intubations went smoothly. The EFL did not indicate arytenoid dislocation. Therefore, the anesthesiologist disagreed with the speculation that tracheal intubation caused VCP. Trauma can also lead to VCP. CT showed the left transverse process of atlas was fractured (Fig. 1D). But the transverse and longitudinal diameters of the atlas are large, the atlas fractures rarely cause VCP. VCP is possible exist when the atlas has a Jefferson fracture.8,9 In this case, the degree of atlas fractures was mild. So it was not the responsible of this disease. We were confused until we discovered the tongue of patient was tilted to the left (Fig. 1G). And then, we tested the patient's sense of taste. The patient told us that she lost the taste in the posterior third of the tongue. It was a typical clinical manifestation of cranial nerve IX injury. Both cranial nerve IX and X are damaged at the same time, there will be hoarseness and difficulty swallowing. Cranial nerve XII injury will cause atrophy of the ipsilateral tongue muscles, and the tongue will be deflected to the affected side. There was no clinical manifestation of cranial nerve XI damage in this patient. We suspected that the cranial nerve XI damage might be mild, or the course of the disease might be short and had not been manifest. CT indicated that bilateral skull base fractures (Fig. 1E and F). Collet-Sicard syndrome was diagnosed successfully.
In conclusion, when patients with head trauma have hoarseness and difficulty swallowing, CT examination of the skull base must be performed. The doctor must check the taste, tongue muscle and sternocleidomastoid muscle of patient. If the condition is stable, conservative treatment is recommended. Nutritional nerve therapy and swallowing rehabilitation are necessary.2 This case reports our incorrect diagnosis process, in order to young doctors to have a deeper and comprehensive understanding of Collet-Sicard syndrome.
DisclosureInformed consent was obtained for publication of the pafient's details described in this report.
This work was supported by the Basic Medical and Health Technology Project of Wenzhou Science and Technology Bureau [grant numbers Y20190198] and the Scientific Research Incubation Project of The First Affiliated Hospital of Wenzhou Medical University [grant numbers FHY2019021].