In addition to stent retrievers, direct aspiration has become a reasonable thrombectomy strategy.
ObjectivesWe carried out the thrombectomy by guiding the aspiration catheter fully over the clot and performing immediate manual aspiration; we call this procedure “embed aspiration”.
MethodsIn this prospective, non-randomised, single-centre study, we included all patients treated at a high volume-of-care stroke centre between 2017 and 2018 for the TRIANA (Thrombectomy in Andalusia using Aspiration) registry. Thrombectomy was carried out by embed aspiration. Patients were classified according to the success (eTICI 2b67-2c-3) or failure (eTICI 0-1-2a-2b50) of the procedure. Baseline clinical data and outcomes were compared, and multivariate analysis was performed.
ResultsThe embed aspiration technique was used in 370 patients. Treatment was successful in 90.3% of patients. Mean puncture-to-recanalisation time was 25 minutes. The overall rate of good outcomes (mRS 0–2) at 3 months was 64%.
ConclusionsThis study supports real-life evidence that standardised embed aspiration may be an alternative to stent retrievers for thrombectomy.
Más allá del empleo del stentriever, la aspiración directa se ha convertido en una estrategia razonable para la trombectomía.
ObjetivosEn este estudio se ha realizado la trombectomía capturando el trombo mediante el catéter de aspiración y llevando a cabo una aspiración manual inmediata, esto lo hemos denominado aspiración por captura (embaspiración).
MétodosEn este estudio prospectivo, no aleatorizado y unicéntrico, todos los pacientes de un Centro de Ictus de alto volumen asistencial tratados entre los años 2017 y 2018 fueron reclutados para el registro TRIANA (ThRombectomy In ANdalusia using Aspiration). La trombectomía se realizó mediante aspiración por captura. Establecimos 2 grupos diferentes de estudio en relación con el éxito (eTICI 2b67-2c-3) o fracaso (eTICI 0-1-2a-2b50) de la técnica. Las características clínicas basales y los resultados fueron comparados, y se realizó un análisis multivariante.
ResultadosTrescientos setenta pacientes fueron tratados mediante la técnica de aspiración por captura. La recanalización exitosa se logró en el 90,3% de los casos. El tiempo medio punción-recanalización fue de 25 min. El buen pronóstico global (mRS 0-2) a los 3 meses fue del 64%.
ConclusionesEste estudio aporta experiencia en vida real para la estandarización de la aspiración por captura, pudiendo ser una alternativa al stentriever en la trombectomía.
Endovascular treatment is part of the standard management of patients with acute ischaemic stroke (AIS) due to large vessel occlusion,1 as established in clinical trials using a stent retriever as the main approach.2–4 However, it is yet to be determined whether the benefit observed in these trials persists when a different reperfusion technique is used.
Two non-randomised clinical trials (ASTER5 and COMPASS6) compared contact aspiration against stent retriever thrombectomy as the first-line endovascular approach, considering the possibility of changing to another type of therapy if needed. Other studies have suggested aspiration as a reasonable treatment strategy. In any case, the latest guidelines still recommend using the stent retriever over aspiration in mechanical thrombectomy,7 despite the non-inferiority results shown in some clinical trials.1
One of the greatest disadvantages of aspiration is the lack of a standardised technique. The Direct Aspiration First Pass Technique (ADAPT), which consists of aspirating over the surface of the thrombus,8 was the first to be described, and subsequently became the most popular technique.
In order to aspirate the thrombus, the aspiration catheter must fully engage the thrombus.
This technique was proposed with the aim of minimising distal embolisation, as well as achieving a high rate of first-pass success.9 Numerous articles on the SOFIA™ aspiration catheter show its safety and effectiveness when the contact aspiration technique is applied,10–12 but not with the “embed aspiration” technique used at our centre.
The aim of the study was to assess embed aspiration in clinical practice. We focused on the rate of recanalisation and the duration of the endovascular procedure, as well as its possible influence on clinical outcomes.
Patients and methodsStudy design and participantsThe prospective, non-randomised Thrombectomy in Andalusia using Aspiration (TRIANA) registry (ClinicalTrials.gov identifier: NCT03407092) was conducted between 2017 and 2018. We selected 2 centres from the same region, with both performing a high number of treatment procedures. One of the centres performed embed aspiration thrombectomy using a SOFIA™ catheter as first line treatment. The other centre used the Solumbra technique with a Trevo™ stent retriever in combination with the SOFIA™ aspiration catheter.
In the present study, we exclusively analyse data from the former centre. The initial approach in all patients was embed aspiration using a SOFIA™ catheter, in which the catheter is placed fully over the thrombus with the aim of capturing the thrombus at once.
Unlike the ADAPT technique, embed aspiration fully captures the thrombus inside the catheter. The centre performing this technique serves a total population of 2 458 000.
Patient selectionThe study included patients with AIS of 6 hours’ progression, or who met standard criteria for wake-up stroke, stroke with unknown time of onset, or stroke of 6–24 hours’ progression and meeting advanced imaging criteria (computed tomography [CT] reperfusion).1 Selection criteria were: 1) aged 18 years or older; 2) baseline modified Rankin Scale (mRS) score of 0–2; 3) vascular occlusion in the terminal segment of the internal carotid artery, or M1/M2 segments of the middle cerebral artery with possible tandem occlusions; 4) Alberta Stroke Program Early CT Score (ASPECTS) of 6 or higher, calculated with the support of machine-learning digital imaging processing software (Brainomix® e-ASPECTS)13; and 5) meeting the DAWN3 or DEFUSE 3 criteria4 for wake-up stroke, stroke with unknown time of onset, or stroke of 6–24 hours’ progression.
Study group analysisTo determine the outcomes of this technique, we divided the sample in 2 study groups:
- a)
Patients in whom the embed aspiration technique was sufficient;
- b)
Patients who required a rescue intervention with a stent retriever following unsuccessful embed aspiration.
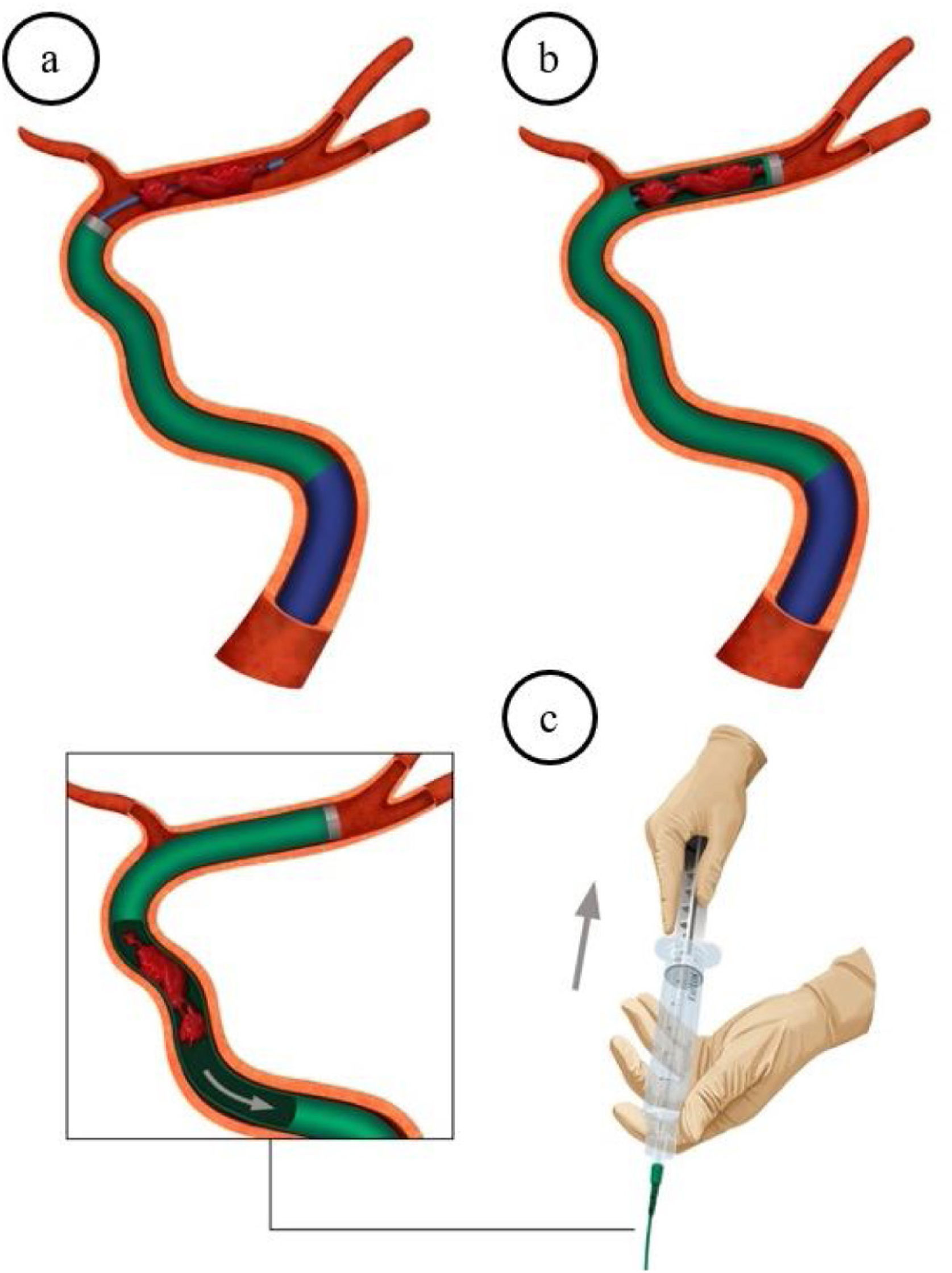
In the embed aspiration technique (Fig. 1), the transfemoral approach is used to insert an 8 F guide catheter (NeuronMax™ 088) as distally as possible into the internal carotid artery of the affected side. Subsequently, a SOFIA™ catheter is carefully guided to the occlusion site, usually over a Rebar™ 0.027″/0.021″ microcatheter and a Transend™ 0.014″ guidewire, with both reaching beyond the occlusion. Next, the aspiration catheter is placed over the whole thrombus with the aim of capturing it at once. Finally, the microcatheter and guidewire are removed, and manual aspiration is performed with a 60 mL VacLock™ aspiration syringe, which is directly connected. The aspiration catheter is immediately and slowly withdrawn until flow appears in the system. If this does not occur, then the thrombus is inside the catheter, and the aspiration catheter would be fully removed using simultaneous manual aspiration through the guide catheter.
Embed aspiration technique.
a) NeuronMax™ 088 is inserted as distally as possible in the internal carotid artery. The SOFIA™ 6 F/5 F aspiration catheter is advanced to the occlusion, using a Rebar™ 0.027″/0.021″ microcatheter and a Transend™ 0.014″ guidewire. b) The aspiration catheter is placed over the whole thrombus with the aim of capturing it at once. c) The microcatheter and guidewire are removed after the SOFIA™ catheter is placed. Manual aspiration is performed with a directly connected 60 mL VacLock™ syringe.
At least 3 passes are made with this technique as first line treatment.
In the event of failure of embed aspiration, the interventional neurologist decides whether to proceed with a stent retriever or discontinue the procedure.
Thrombectomy was performed using local anaesthesia as first option, and general anaesthesia or conscious sedation when necessary, mainly due to the need for reduced level of consciousness or excess movement, which would impede performing endovascular treatment safely.
Data collection and assessmentWe prospectively gathered all data, including clinical and laboratory variables and details of the endovascular procedure, from the A Registry for Thrombectomy In Stroke Therapy from Andalusia (ARTISTA) registry, jointly developed by interventional neuroradiologists and vascular neurologists.
Our primary objective was to assess the rate of recanalisation and functional independence at 3 months. Our secondary aims were to analyse the duration of the procedure and identify possible predictors of poor outcomes.
Successful recanalisation was defined as an expanded Thrombolysis In Cerebral Ischemia (eTICI) grade 2b67-2c-3, meaning a reperfusion of 67% or more of the territory in the final angiography study.14
The presence of symptomatic or asymptomatic cerebral haemorrhage (any haemorrhagic transformation associated with a neurological deterioration of ≥ 4 points in the National Institutes of Health Stroke Scale [NIHSS]) was assessed using the European Cooperative Acute Stroke Study (ECASS) classification.15
Clinical outcomes were assessed by neurologists not involved in the endovascular treatment and with extensive experience in cerebrovascular disease. The NIHSS was used to assess patients’ neurological status at baseline, after the procedure and at discharge, and 3-month functional outcomes were assessed with the mRS score. To determine patients’ neurological prognosis, we used the mRS score at 90 days; favourable prognosis was defined as mRS score ≤ 2.
Ethical considerations and external validityThe protocol and informed consent forms of the TRIANA registry were approved by the local research ethics committee (ID 0992-N-17).
The informed consent of patients’ families was obtained before the procedure.
Brain arteriography images were anonymised and sent to a laboratory in the Digital Imaging and Communication in Medicine (DICOM) format for an external assessment of the eTICI. The central laboratory was in the charge of one of the co-authors (Luis San Román) of the HERMES collaboration.
Statistical analysisAll categorical variables were expressed as absolute values and frequencies (%), whereas continuous variables were expressed as means (SD) or median (Q1–Q3). For the bivariate analysis, we used the chi-square test, Fisher exact test, t test, Mann–Whitney U test, Kruskal–Wallis test, or ANOVA, as appropriate.
We used the univariate logistic regression model to determine the association between prognostic predictors (mRS at 90 days, divided into mRS 0–2 and mRS 3–6). Those variables significantly associated with favourable outcomes (P < .1) in the univariate analysis were included in the multivariate models.
We used the IBM SPSS Statistics software (version 23, IBM®) for all statistical analysis. Statistical significance was set at P < .05.
ResultsBaseline patient characteristicsThis study gathered data from 370 patients with AIS and large vessel occlusion. Embed aspiration was the only technique used in 283 (76.5%) patients. The remaining 87 (23.5%) patients underwent rescue therapy with a stent retriever after initial unsuccessful treatment with embed aspiration.
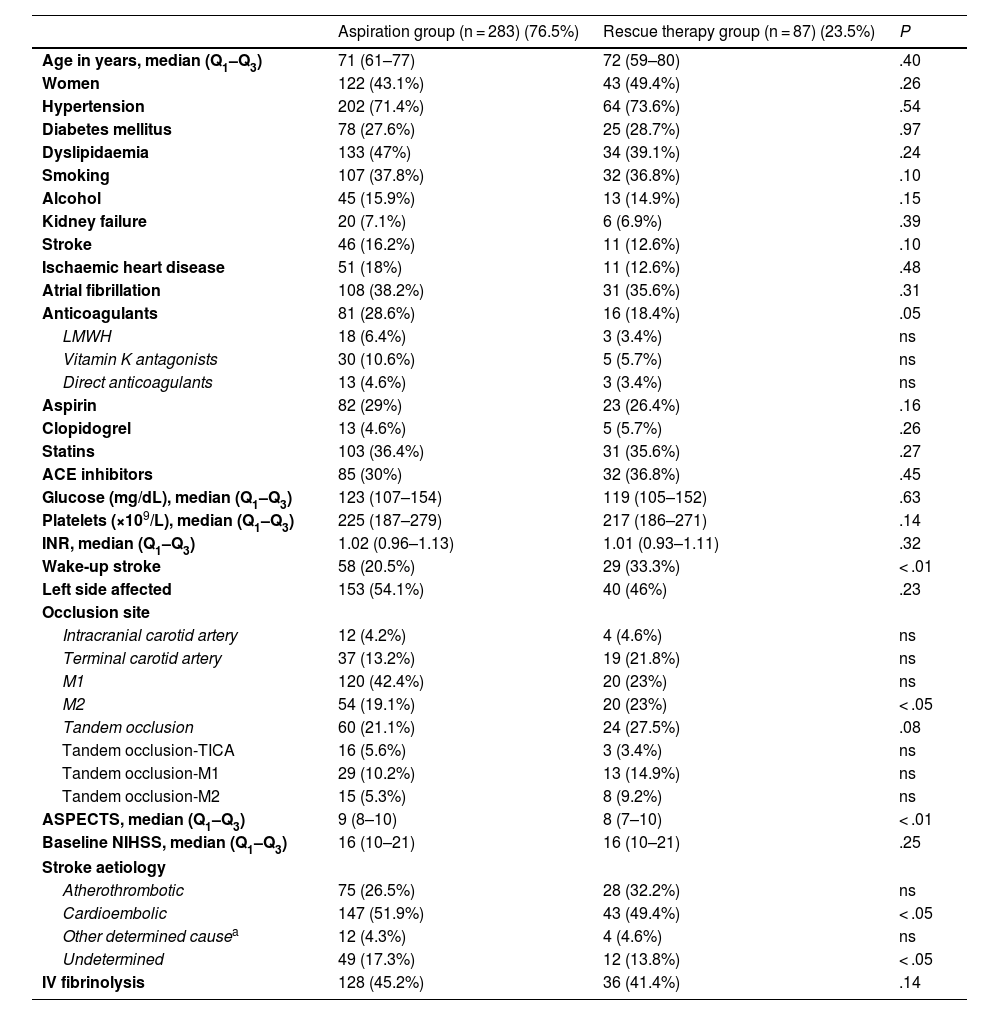
Table 1 shows the baseline data from both study groups. The median baseline mRS score was 0 in both groups.
Baseline clinical characteristics.
| Aspiration group (n = 283) (76.5%) | Rescue therapy group (n = 87) (23.5%) | P | |
|---|---|---|---|
| Age in years, median (Q1–Q3) | 71 (61–77) | 72 (59–80) | .40 |
| Women | 122 (43.1%) | 43 (49.4%) | .26 |
| Hypertension | 202 (71.4%) | 64 (73.6%) | .54 |
| Diabetes mellitus | 78 (27.6%) | 25 (28.7%) | .97 |
| Dyslipidaemia | 133 (47%) | 34 (39.1%) | .24 |
| Smoking | 107 (37.8%) | 32 (36.8%) | .10 |
| Alcohol | 45 (15.9%) | 13 (14.9%) | .15 |
| Kidney failure | 20 (7.1%) | 6 (6.9%) | .39 |
| Stroke | 46 (16.2%) | 11 (12.6%) | .10 |
| Ischaemic heart disease | 51 (18%) | 11 (12.6%) | .48 |
| Atrial fibrillation | 108 (38.2%) | 31 (35.6%) | .31 |
| Anticoagulants | 81 (28.6%) | 16 (18.4%) | .05 |
| LMWH | 18 (6.4%) | 3 (3.4%) | ns |
| Vitamin K antagonists | 30 (10.6%) | 5 (5.7%) | ns |
| Direct anticoagulants | 13 (4.6%) | 3 (3.4%) | ns |
| Aspirin | 82 (29%) | 23 (26.4%) | .16 |
| Clopidogrel | 13 (4.6%) | 5 (5.7%) | .26 |
| Statins | 103 (36.4%) | 31 (35.6%) | .27 |
| ACE inhibitors | 85 (30%) | 32 (36.8%) | .45 |
| Glucose (mg/dL), median (Q1–Q3) | 123 (107–154) | 119 (105–152) | .63 |
| Platelets (×109/L), median (Q1–Q3) | 225 (187–279) | 217 (186–271) | .14 |
| INR, median (Q1–Q3) | 1.02 (0.96–1.13) | 1.01 (0.93–1.11) | .32 |
| Wake-up stroke | 58 (20.5%) | 29 (33.3%) | < .01 |
| Left side affected | 153 (54.1%) | 40 (46%) | .23 |
| Occlusion site | |||
| Intracranial carotid artery | 12 (4.2%) | 4 (4.6%) | ns |
| Terminal carotid artery | 37 (13.2%) | 19 (21.8%) | ns |
| M1 | 120 (42.4%) | 20 (23%) | ns |
| M2 | 54 (19.1%) | 20 (23%) | < .05 |
| Tandem occlusion | 60 (21.1%) | 24 (27.5%) | .08 |
| Tandem occlusion-TICA | 16 (5.6%) | 3 (3.4%) | ns |
| Tandem occlusion-M1 | 29 (10.2%) | 13 (14.9%) | ns |
| Tandem occlusion-M2 | 15 (5.3%) | 8 (9.2%) | ns |
| ASPECTS, median (Q1–Q3) | 9 (8–10) | 8 (7–10) | < .01 |
| Baseline NIHSS, median (Q1–Q3) | 16 (10–21) | 16 (10–21) | .25 |
| Stroke aetiology | |||
| Atherothrombotic | 75 (26.5%) | 28 (32.2%) | ns |
| Cardioembolic | 147 (51.9%) | 43 (49.4%) | < .05 |
| Other determined causea | 12 (4.3%) | 4 (4.6%) | ns |
| Undetermined | 49 (17.3%) | 12 (13.8%) | < .05 |
| IV fibrinolysis | 128 (45.2%) | 36 (41.4%) | .14 |
ACE: angiotensin-converting enzyme; ASPECTS: Alberta Stroke Program Early Computed Tomography Score; INR: International Normalized Ratio; IV: intravenous; LMWH: low molecular weight heparin; NIHSS: National Institutes of Health Stroke Scale; Q1–Q3: quartiles 1 and 3; TICA: terminal internal carotid artery.
Overall, recanalisation was successful (eTICI 2b67-2c-3) in 334 patients (90.3%).
The median puncture-to-recanalisation time was 25 minutes (Q1–Q3, 13–52 min). A median of 2 (Q1–Q3, 1–3) passes were needed to achieve revascularisation.
Local anaesthesia was used in 88.2% of the patients. Conscious sedation was used in approximately 3.2% of cases. General anaesthesia was required in 8.6%.
The overall rate of good functional prognosis was 64%. The mortality rate amounted to 11.1%.
Haemorrhagic transformation was detected in 51 patients (13.7%), but only 21 (5.7%) were symptomatic.
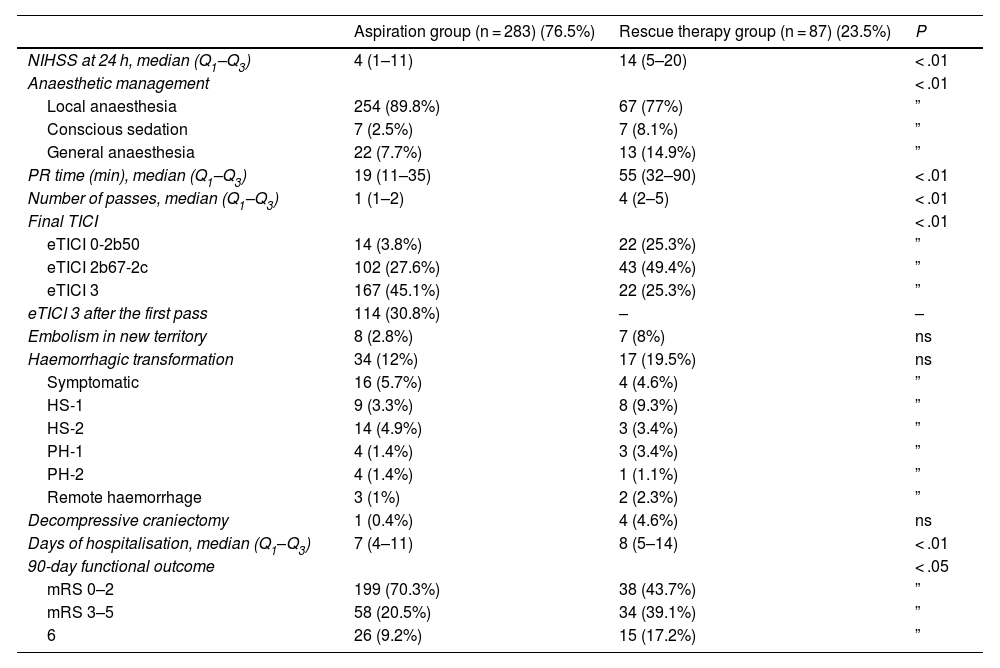
Table 2 shows the clinical and procedure outcomes in each group.
Clinical and procedure outcomes and anaesthetic management.
| Aspiration group (n = 283) (76.5%) | Rescue therapy group (n = 87) (23.5%) | P | |
|---|---|---|---|
| NIHSS at 24 h, median (Q1–Q3) | 4 (1–11) | 14 (5–20) | < .01 |
| Anaesthetic management | < .01 | ||
| Local anaesthesia | 254 (89.8%) | 67 (77%) | ” |
| Conscious sedation | 7 (2.5%) | 7 (8.1%) | ” |
| General anaesthesia | 22 (7.7%) | 13 (14.9%) | ” |
| PR time (min), median (Q1–Q3) | 19 (11–35) | 55 (32–90) | < .01 |
| Number of passes, median (Q1–Q3) | 1 (1–2) | 4 (2–5) | < .01 |
| Final TICI | < .01 | ||
| eTICI 0-2b50 | 14 (3.8%) | 22 (25.3%) | ” |
| eTICI 2b67-2c | 102 (27.6%) | 43 (49.4%) | ” |
| eTICI 3 | 167 (45.1%) | 22 (25.3%) | ” |
| eTICI 3 after the first pass | 114 (30.8%) | – | – |
| Embolism in new territory | 8 (2.8%) | 7 (8%) | ns |
| Haemorrhagic transformation | 34 (12%) | 17 (19.5%) | ns |
| Symptomatic | 16 (5.7%) | 4 (4.6%) | ” |
| HS-1 | 9 (3.3%) | 8 (9.3%) | ” |
| HS-2 | 14 (4.9%) | 3 (3.4%) | ” |
| PH-1 | 4 (1.4%) | 3 (3.4%) | ” |
| PH-2 | 4 (1.4%) | 1 (1.1%) | ” |
| Remote haemorrhage | 3 (1%) | 2 (2.3%) | ” |
| Decompressive craniectomy | 1 (0.4%) | 4 (4.6%) | ns |
| Days of hospitalisation, median (Q1–Q3) | 7 (4–11) | 8 (5–14) | < .01 |
| 90-day functional outcome | < .05 | ||
| mRS 0–2 | 199 (70.3%) | 38 (43.7%) | ” |
| mRS 3–5 | 58 (20.5%) | 34 (39.1%) | ” |
| 6 | 26 (9.2%) | 15 (17.2%) | ” |
eTICI: expanded Thrombolysis In Cerebral Ischemia score; HS: haemorrhagic stroke; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; PH: parenchymal haemorrhage; PR: puncture-to-recanalisation; Q1–Q3: quartiles 1 and 3.
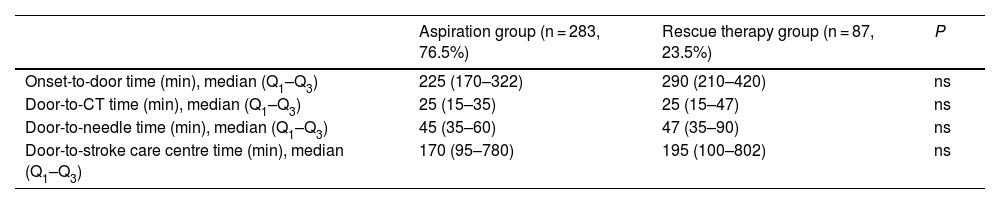
Table 3 presents the management times.
Intervention times.
| Aspiration group (n = 283, 76.5%) | Rescue therapy group (n = 87, 23.5%) | P | |
|---|---|---|---|
| Onset-to-door time (min), median (Q1–Q3) | 225 (170–322) | 290 (210–420) | ns |
| Door-to-CT time (min), median (Q1–Q3) | 25 (15–35) | 25 (15–47) | ns |
| Door-to-needle time (min), median (Q1–Q3) | 45 (35–60) | 47 (35–90) | ns |
| Door-to-stroke care centre time (min), median (Q1–Q3) | 170 (95–780) | 195 (100–802) | ns |
Q1–Q3: quartiles 1 and 3.
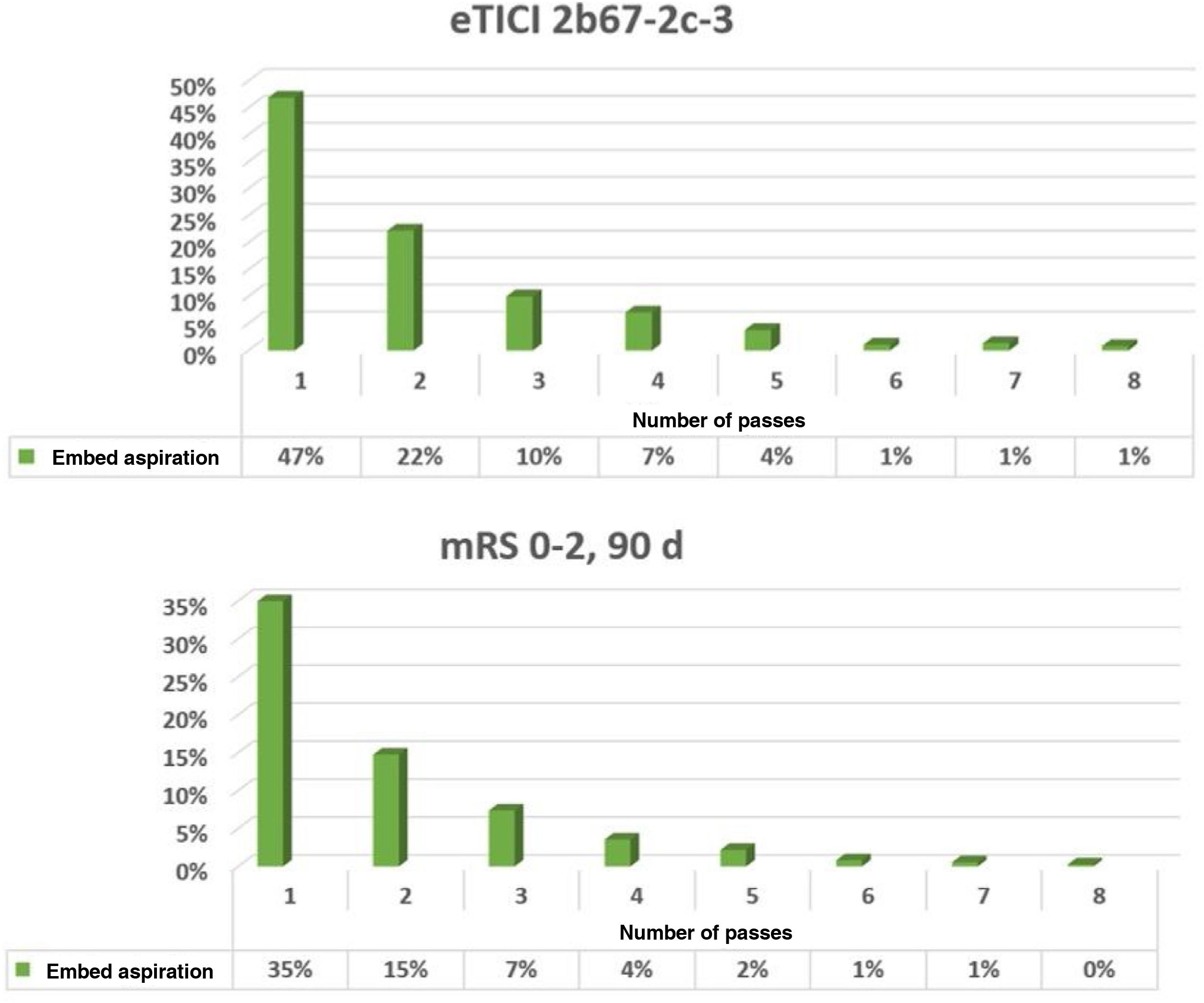
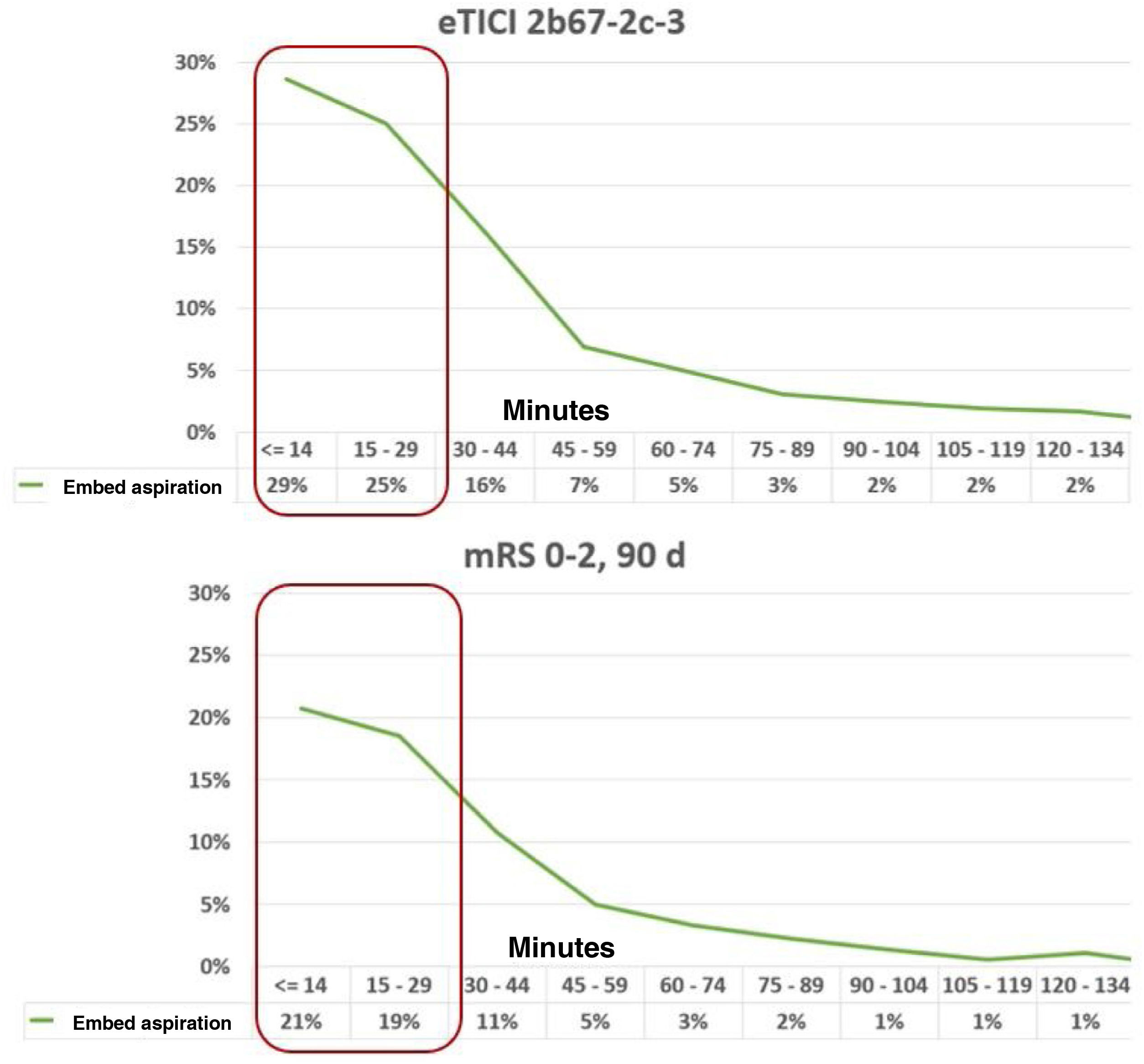
Figs. 2 and 3 show the relationship between angiography and clinical results and the number of passes and puncture-to-recanalisation time.
Relationship between angiography and clinical results and number of passes.
In patients requiring one aspiration pass, the rate of successful recanalisation was 47%, with a corresponding good functional prognosis rate of 35%.
d: Days; eTICI: expanded Treatment In Cerebral Ischemia; mRS: modified Rankin Scale.
Relationship between angiography and clinical results and puncture-to-recanalisation time. The first 30 minutes are shown inside red rectangles.
For puncture-to-recanalisation times of 30 minutes or less, the rate of successful recanalisation amounted to 54%, with good functional outcomes at 3 months in 40%.
d: days; eTICI: expanded Treatment In Cerebral Ischemia; mRS: modified Rankin Scale.
In patients requiring one aspiration pass, the rate of successful recanalisation was 47%, with a corresponding good functional prognosis rate of 35%.
Furthermore, when the puncture-to-recanalisation time was 30 minutes or less, the rate of successful recanalisation amounted to 54%, with 40% of patients presenting good functional outcomes at 3 months.
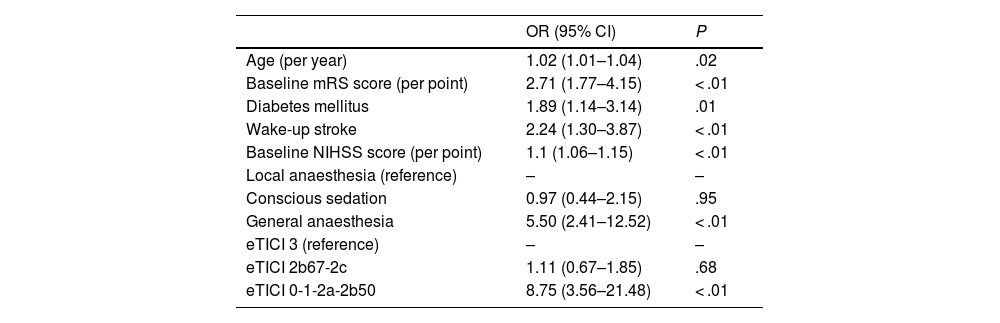
Multivariate logistic regression analysisTable 4 shows the results of the multivariate logistic regression analysis. The multivariate analysis of all patients confirmed that a poor functional prognosis (mRS 3–6) was associated with age (odds ratio [OR]: 1.02; 95% confidence interval [95% CI], 1.01–1.04; P = .02), poorer baseline mRS score (OR: 2.71; 95% CI, 1.77–4.15; P < .01), diabetes (OR: 1.89; 95% CI, 1.14–3.14; P = .01), wake-up stroke (OR: 2.24; 95% CI, 1.30–3.87; P < .01), pre-intervention NIHSS score (OR: 1.1; 95% CI, 1.06–1.15; P < .01), general anaesthesia (OR: 5.50; 95% CI, 2.41–12.52; P < .01), eTICI score of 0-2b50 (OR: 8.75; 95% CI, 3.56–21.48; P < .01), and failed embed aspiration (OR: 2.33; 95% CI, 1.18–4.59; P = .01).
Multivariate logistic regression analysis of predictors of poor prognosis (mRS 3–6) at 90 days.
| OR (95% CI) | P | |
|---|---|---|
| Age (per year) | 1.02 (1.01–1.04) | .02 |
| Baseline mRS score (per point) | 2.71 (1.77–4.15) | < .01 |
| Diabetes mellitus | 1.89 (1.14–3.14) | .01 |
| Wake-up stroke | 2.24 (1.30–3.87) | < .01 |
| Baseline NIHSS score (per point) | 1.1 (1.06–1.15) | < .01 |
| Local anaesthesia (reference) | – | – |
| Conscious sedation | 0.97 (0.44–2.15) | .95 |
| General anaesthesia | 5.50 (2.41–12.52) | < .01 |
| eTICI 3 (reference) | – | – |
| eTICI 2b67-2c | 1.11 (0.67–1.85) | .68 |
| eTICI 0-1-2a-2b50 | 8.75 (3.56–21.48) | < .01 |
95% CI: 95% confidence interval; eTICI: expanded Thrombolysis In Cerebral Ischemia score; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; OR: odds ratio.
Our results show a successful recanalisation rate of 72.7% with embed aspiration only, increasing to 90.3% with rescue therapy. The ASTER5 and COMPASS6 trials compared aspiration against stent retriever thrombectomy in the endovascular treatment of AIS. In the ASTER5 trial, the rate of recanalisation achieved with contact aspiration was 63%, reaching 85.4% after rescue therapy. However, in the stent retriever group, the successful recanalisation rate amounted to 67.7%, increasing to 83.1% when rescue therapy was used. The COMPASS6 trial reported rates of 83% and 92% in the aspiration group and 82% and 89% in the stent retriever group. Current evidence supporting endovascular treatment for AIS is based on clinical trials that have used the stent retriever as the main approach, with no possibility of rescue therapy.2–4
The “first-pass effect” has become a new measure of success for thrombectomy devices.16 In the TRIANA registry, the rate of successful recanalisation after the first pass with embed aspiration amounted to 47%. In the COMPASS trial,6 a TICI of 2b or higher was achieved after the first pass in 57% of the patients in the aspiration group and 51% in the stent retriever group.
It is possible that such other factors as the duration of the procedure may significantly influence clinical results.17–19 These benefits, observed in real-life data,20 may be explained by the optimisation resulting from the experience of stroke care centres performing a large number of thrombectomies and with highly experienced interventional neurologists. In our study, the puncture-to-recanalisation time amounted to a median of 25 minutes for aspiration overall, close to the times reported in the ASTER5 (38 min) and COMPASS6 trials (25 min). The successful recanalisation rate was 29% in the first 15 minutes and 54% in the first 30. This may have contributed to the good functional prognosis. The COMPASS6 trial reported a TICI 2b or better within the first 45 minutes in 76% of patients in the aspiration group, and 68% in the stent retriever group.
Embolism in new territories amounted to 4%, similar to the rates observed in the aspiration groups in the ASTER5 trial (3.7%) and the COMPASS trial (3%).6
The rates of functional independence at 3 months after endovascular treatment in the ASTER5 trial amounted to 45.3% in the aspiration group and 50% in the stent retriever group, whereas the COMPASS6 trial reported rates of 52% in the aspiration group and 51% in the stent retriever group. In our study, 64% of patients presented mRS scores of 0–2 at 3 months.
The need for rescue therapy with a stent retriever extended the puncture-to-recanalisation time from 19 to 55 minutes, which had a considerable impact on clinical outcomes that may not be attributed to the use of the technique.
In the future, we may perform a procedure adapted to each patient to avoid this situation. Although first-line treatment with aspiration and with stent retriever could not be compared, the data included in the tables may inform future studies to identify factors affecting such procedures.
The use of general anaesthesia has not been clearly associated with prognosis.21–23 In our study, local anaesthesia was used in 88.2% of the total sample. Although anaesthetic management was governed by the centre’s protocols, the small number of patients requiring general anaesthesia may be explained by the fast performance and versatility of the aspiration technique. In any case, the use of general anaesthesia was a significant prognostic factor associated with poorer clinical outcomes. We cannot rule out that the circumstances leading to the use of general anaesthesia (low level of consciousness, excess movement during the procedure), which are difficult to control for in logistic regression analysis, had some kind of impact on these results. Avoiding general anaesthesia whenever possible may be related with better functional outcomes.24
Finally, better results have been observed in the endovascular treatment of large vessel occlusion of cardioembolic origin vs non-cardioembolic origin.25 In our study, cardioembolic aetiology was observed in 51.9% of patients in the aspiration group. However, these results did not show a statistically significant difference in the multivariate logistic regression analysis.
Our study presents some strengths and limitations that should be mentioned. This is a non-randomised, single-centre study that does not compare aspiration against standard treatment with stent retriever. Although the neurological examination was performed by neurologists not involved in the procedure and with extensive experience in the management of acute cerebrovascular disease, the assessment of functional independence at 3 months was open and performed by neurologists from the same centre. Nevertheless, this is a pragmatic study with real-world data that may generate relevant evidence on the embed aspiration technique.
ConclusionThis study provides real-world evidence that the embed aspiration technique may achieve good results when used as the only treatment.
It may represent a starting point for the design of new clinical trials analysing the standardisation of aspiration approaches in the endovascular treatment of stroke.
FundingThis study was financed by a grant from the Andalusian Regional Department of Health (PI-0374-2017).
Conflicts of interestGrifols® and Medtronic® partially funded the TRIANA project, but did not participate in the design, interpretation of data, or approval of the manuscript.
ContributionsA. de Albóniga-Chindurza and A. González drafted the manuscript.
J. Montaner and A. González designed the study.
A. de Albóniga-Chindurza, J. Montaner, and A. González analysed and interpreted data.
L. San Román, of the Laboratorio Central Angiográfico, analysed all angiography studies.
A. Cayuela and A. González performed the statistical analysis.
F. Moniche, L. San Román, I. Escudero-Martínez, and J. Montaner reviewed the manuscript.
All authors participated in data collection and approved the final version of the article.
We would like to thank Alan Campbell, PhD (Middle Tennessee State University) for his help editing the manuscript. We would like to thank Julián Baena for the design of the figures.