This study aimed to determine whether encephalopathy is associated with such COVID-19 outcomes as disease severity, mortality, respiratory failure, intensive care unit (ICU) admission, duration of ventilator dependence, and length of ICU and hospital stay.
MethodsWe performed a subgroup analysis comparing outcomes in patients with and without encephalopathy, based on data from a nationwide retrospective cohort study among adult patients hospitalized with COVID-19 at 37 hospital sites in the Philippines. The patient outcomes included for analysis were disease severity, mortality, respiratory failure, ICU admission, duration of ventilator dependence, and length of ICU and hospital stay.
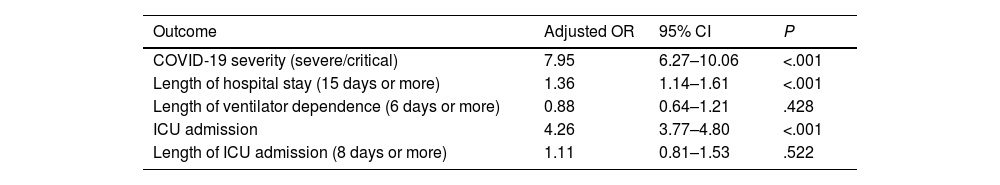
ResultsOf a total of 10881 COVID-19 admissions, 622 patients had encephalopathy. The adjusted hazard ratios (aHR) for mortality among mild and severe cases were 9.26 and 1.63 times greater (P<.001), respectively, in the encephalopathy group compared to the no-encephalopathy group. Encephalopathy was associated with increased risk of severe COVID-19 (adjusted odds ratio [aOR]: 7.95; P<.001), respiratory failure (aHR: 5.40; P<.001), longer hospital stays (aOR: 1.36; P<.001), and admission to the ICU (aOR: 4.26; P<.001). We found no sufficient evidence that encephalopathy was associated with length of ICU stay (aOR: 1.11; P=.522) or duration of ventilator dependence (aOR: 0.88; P=.428).
ConclusionsEncephalopathy was associated with COVID-19 severity, mortality, respiratory failure, ICU admission, and longer hospital stays.
Nuestro estudio tuvo como objetivo determinar si la encefalopatía estaba asociada con los resultados de COVID-19, como la gravedad de la enfermedad, la mortalidad, la insuficiencia respiratoria, el ingreso a la unidad de cuidados intensivos (UCI) y la duración de la dependencia del ventilador, la estancia en la UCI y en el hospital.
MétodosRealizamos un análisis de subgrupos comparando los resultados de los pacientes con encefalopatía frente a los pacientes sin encefalopatía, basado en datos de un estudio de cohorte retrospectivo a nivel nacional entre pacientes adultos hospitalizados con COVID-19 en 37 hospitales en Filipinas. Los resultados del paciente incluidos para el análisis fueron la gravedad de la enfermedad, la mortalidad, la insuficiencia respiratoria, el ingreso a la UCI y la duración de la dependencia del ventilador, la estancia en la UCI y en el hospital.
ResultadosDe las 10.881 admisiones totales por COVID-19, 622 pacientes tenían encefalopatía. Las razones de riesgo ajustadas (aHR) para la mortalidad entre casos leves y graves fueron mayores en 9,26 y en 1,63 (p<0,001), respectivamente, en el grupo de encefalopatía en comparación con el grupo sin encefalopatía. La encefalopatía se asoció con un mayor riesgo de tener COVID-19 grave (razón de posibilidades ajustada [aOR] 7,95, p<0,001), insuficiencia respiratoria (aHR 5,40, p<0,001), estancia hospitalaria más larga (aOR 1,36, p<0,001) e ingreso a la UCI (aOR 4,26, p<0,001). No encontramos suficiente evidencia de que la encefalopatía estuviera asociada con la duración del ingreso a la UCI (aOR 1,11, p=0,522) y la duración de la dependencia del ventilador (aOR 0,88, p=0,428).
ConclusionesLa encefalopatía estuvo asociada con la gravedad de la COVID-19, la mortalidad, la insuficiencia respiratoria, el ingreso a la UCI y una estancia hospitalaria más prolongada.
COVID-19, caused by SARS-CoV-2 infection, primarily affects the respiratory system but is also known to affect the nervous system.1 The neurological manifestations reported in hospitalized patients with COVID-19 include headache, dizziness, anosmia, ageusia, impaired consciousness, seizures, and stroke.2–4 More recently, larger studies on new-onset neurological disorders associated with the disease identified encephalopathy as one of the most common diagnoses, occurring in 20–44% of patients with neurological disorders.4–6
Encephalopathy is a diffuse brain dysfunction characterized by impaired level of consciousness, which can present as delirium, stupor, or coma.7 The most common causes of encephalopathy among patients with COVID-19 were sepsis-associated encephalopathy, uremic encephalopathy, and hypoxic ischemic encephalopathy.8 The underlying causes of encephalopathy may be attributed to multiple mechanisms, such as neurotropism of the SARS-CoV-2 virus, severe inflammatory response leading to multiple organ dysfunction or acute respiratory distress syndrome, coagulopathy, and hypoxia.9,10
In studies among hospitalized patients in general, altered sensorium and delirium were associated with longer hospitalization, cognitive impairment, and increased mortality.11–13 However, data are still limited on the association between encephalopathy and other outcome measures among patients with COVID-19.
In the Philippines, the recently concluded nationwide, multicenter, retrospective study of neurological manifestations and associated outcomes (the Philippine CORONA Study) identified encephalopathy as the most common new-onset neurological symptom associated with COVID-19.3 The present study aims to further elucidate whether encephalopathy is associated with COVID-19 outcomes including disease severity, mortality, respiratory failure, intensive care unit (ICU) admission, duration of ventilator dependence, and duration of ICU and hospital stays.
Materials and methodsThe Philippine CORONA Study design: population and settingThe Philippine CORONA Study was a nationwide, multicenter, comparative, retrospective, cohort study including patients with COVID-19 who were admitted consecutively to 37 hospital sites across the Philippines between February and December 2020.3 All data were collected from patient medical charts and coded using the Epi Info Software (version 7.2.2.16). Encephalopathy is defined and widely accepted as a disease in which brain function is altered, often with depressed or fluctuating sensorium. Due to the retrospective nature of the study, any physician assessment stating “encephalopathy” on the chart was counted as a case. The study obtained approval from the respective research ethics boards of the participating hospital sites and was registered on ClinicalTrials.gov (NCT04386083). Specific details about the research design, patient enrollment, and data collection procedures were discussed in the published protocol.14 We included all eligible participants from the main study and classified the patients into 2 cohort groups: those with encephalopathy and those without encephalopathy.
Outcome variablesThe main outcomes were disease severity (mild: presence of mild pneumonia or absence of pneumonia; severe: presence of dyspnea, respiratory rate>30, hypoxia or SpO2<93%, or 50% lung involvement on imaging within 24–48h), mortality, respiratory failure (patients with signs or symptoms of respiratory insufficiency: increased work of breathing/respiratory rate of ≥22, a need for supplemental oxygen, or abnormal blood gases), ICU admission, duration of ventilator dependence, duration of ICU stay, and duration of hospital stay, among patients with encephalopathy compared to the no-encephalopathy group.
Statistical analysisThe different variables of interest were summarized according to the independent variable: encephalopathy versus no encephalopathy. Numerical variables are expressed as median and interquartile range (IQR), while the categorical variables are expressed as count and percentage. Comparison of the different clinical characteristics between the 2 groups was conducted using the Mann–Whitney U test for numerical variables, to determine differences in median/ranks, and the Chi-square test of homogeneity for categorical variables, to determine differences in proportion.
Associations between the different individual dichotomous outcome variables and the independent variable were determined by binary logistic regression. The logistic regression model was adjusted for the following confounders: age, sex, hypertension, diabetes mellitus, smoking, coronary artery disease, cerebrovascular disease, dementia, epilepsy, and COVID-19 severity. The associations between the independent variable and the time to event for different outcome variables were determined by Cox proportional hazards regression. A stratified analysis of mortality between COVID-19 severity types was also performed. All statistical analyses were conducted using Stata version 17.1.
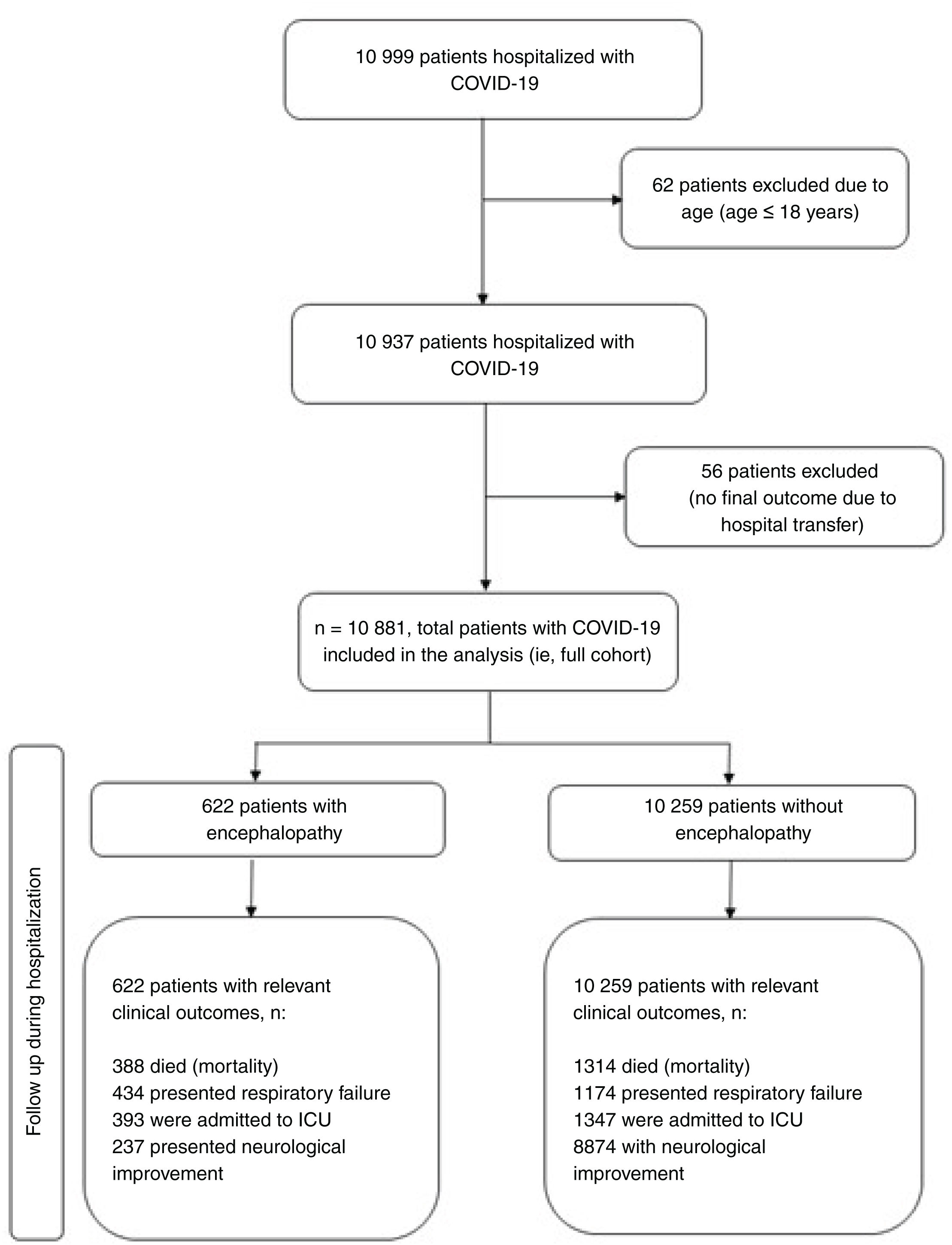
ResultsStudy participantsA total of 10 999 patients consecutively admitted due to confirmed COVID-19 from the 37 participating hospital sites were gathered, with 10 881 patients included in the final analysis. The prevalence of encephalopathy among patients with COVID-19 was 5.72% (95% confidence interval [CI], 5.29–6.17). The encephalopathy group comprised 622 patients, whereas the no-encephalopathy group comprised 10259 patients (Fig. 1). Among patients aged 60 years or older, the prevalence of encephalopathy was higher, at 9.59% (368 of 3834 patients).
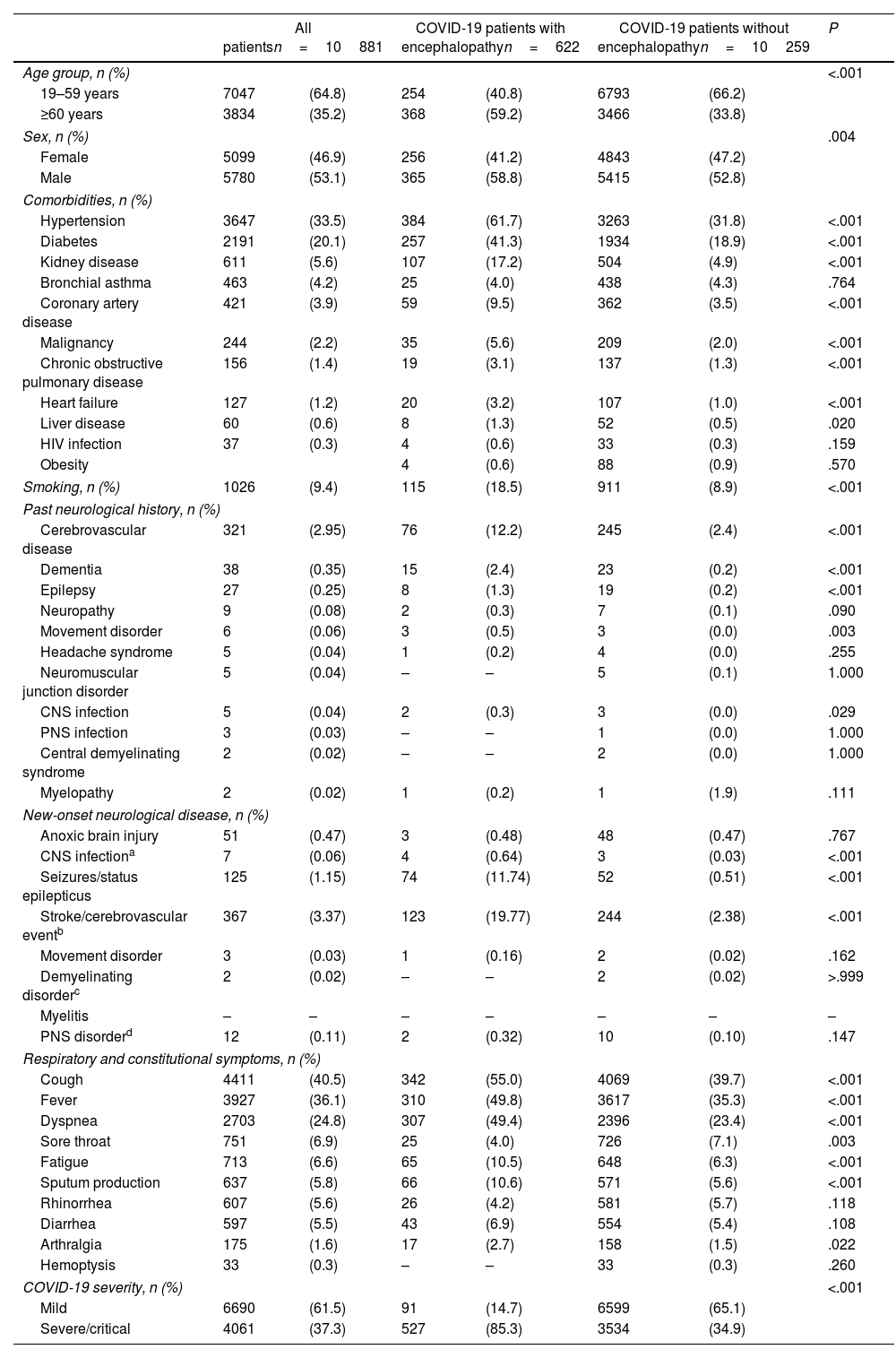
Demographic and clinical characteristicsTable 1 shows the comparison of demographic and clinical characteristics in the encephalopathy and no-encephalopathy groups. The median (IQR) age of the entire cohort was 52 years (36–64). The encephalopathy group had a higher proportion of males (P=.004) and patients aged 60 years and above (P<.001). Presence of hypertension (61.7% vs 31.8%, P<.001), diabetes mellitus (41.3% vs 18.9%, P<.001), kidney disease (17.2% vs 4.9%, P<.001), coronary artery disease (9.5% vs 3.5%, P<.001), malignancy (5.6% vs 2.0%, P<.001), chronic obstructive pulmonary disease (3.1% vs 1.3%, P<.001), and heart failure (3.2% vs 1.0%, P=.02) were more frequent in the encephalopathy group compared to the no-encephalopathy group. Smoking was also more common in the encephalopathy group (18.5% vs 8.9%, P<.001).
Comparison of the clinico-demographic profiles of the encephalopathy and no-encephalopathy groups.
| All patientsn=10881 | COVID-19 patients with encephalopathyn=622 | COVID-19 patients without encephalopathyn=10259 | P | ||||
|---|---|---|---|---|---|---|---|
| Age group, n (%) | <.001 | ||||||
| 19–59 years | 7047 | (64.8) | 254 | (40.8) | 6793 | (66.2) | |
| ≥60 years | 3834 | (35.2) | 368 | (59.2) | 3466 | (33.8) | |
| Sex, n (%) | .004 | ||||||
| Female | 5099 | (46.9) | 256 | (41.2) | 4843 | (47.2) | |
| Male | 5780 | (53.1) | 365 | (58.8) | 5415 | (52.8) | |
| Comorbidities, n (%) | |||||||
| Hypertension | 3647 | (33.5) | 384 | (61.7) | 3263 | (31.8) | <.001 |
| Diabetes | 2191 | (20.1) | 257 | (41.3) | 1934 | (18.9) | <.001 |
| Kidney disease | 611 | (5.6) | 107 | (17.2) | 504 | (4.9) | <.001 |
| Bronchial asthma | 463 | (4.2) | 25 | (4.0) | 438 | (4.3) | .764 |
| Coronary artery disease | 421 | (3.9) | 59 | (9.5) | 362 | (3.5) | <.001 |
| Malignancy | 244 | (2.2) | 35 | (5.6) | 209 | (2.0) | <.001 |
| Chronic obstructive pulmonary disease | 156 | (1.4) | 19 | (3.1) | 137 | (1.3) | <.001 |
| Heart failure | 127 | (1.2) | 20 | (3.2) | 107 | (1.0) | <.001 |
| Liver disease | 60 | (0.6) | 8 | (1.3) | 52 | (0.5) | .020 |
| HIV infection | 37 | (0.3) | 4 | (0.6) | 33 | (0.3) | .159 |
| Obesity | 4 | (0.6) | 88 | (0.9) | .570 | ||
| Smoking, n (%) | 1026 | (9.4) | 115 | (18.5) | 911 | (8.9) | <.001 |
| Past neurological history, n (%) | |||||||
| Cerebrovascular disease | 321 | (2.95) | 76 | (12.2) | 245 | (2.4) | <.001 |
| Dementia | 38 | (0.35) | 15 | (2.4) | 23 | (0.2) | <.001 |
| Epilepsy | 27 | (0.25) | 8 | (1.3) | 19 | (0.2) | <.001 |
| Neuropathy | 9 | (0.08) | 2 | (0.3) | 7 | (0.1) | .090 |
| Movement disorder | 6 | (0.06) | 3 | (0.5) | 3 | (0.0) | .003 |
| Headache syndrome | 5 | (0.04) | 1 | (0.2) | 4 | (0.0) | .255 |
| Neuromuscular junction disorder | 5 | (0.04) | – | – | 5 | (0.1) | 1.000 |
| CNS infection | 5 | (0.04) | 2 | (0.3) | 3 | (0.0) | .029 |
| PNS infection | 3 | (0.03) | – | – | 1 | (0.0) | 1.000 |
| Central demyelinating syndrome | 2 | (0.02) | – | – | 2 | (0.0) | 1.000 |
| Myelopathy | 2 | (0.02) | 1 | (0.2) | 1 | (1.9) | .111 |
| New-onset neurological disease, n (%) | |||||||
| Anoxic brain injury | 51 | (0.47) | 3 | (0.48) | 48 | (0.47) | .767 |
| CNS infectiona | 7 | (0.06) | 4 | (0.64) | 3 | (0.03) | <.001 |
| Seizures/status epilepticus | 125 | (1.15) | 74 | (11.74) | 52 | (0.51) | <.001 |
| Stroke/cerebrovascular eventb | 367 | (3.37) | 123 | (19.77) | 244 | (2.38) | <.001 |
| Movement disorder | 3 | (0.03) | 1 | (0.16) | 2 | (0.02) | .162 |
| Demyelinating disorderc | 2 | (0.02) | – | – | 2 | (0.02) | >.999 |
| Myelitis | – | – | – | – | – | – | – |
| PNS disorderd | 12 | (0.11) | 2 | (0.32) | 10 | (0.10) | .147 |
| Respiratory and constitutional symptoms, n (%) | |||||||
| Cough | 4411 | (40.5) | 342 | (55.0) | 4069 | (39.7) | <.001 |
| Fever | 3927 | (36.1) | 310 | (49.8) | 3617 | (35.3) | <.001 |
| Dyspnea | 2703 | (24.8) | 307 | (49.4) | 2396 | (23.4) | <.001 |
| Sore throat | 751 | (6.9) | 25 | (4.0) | 726 | (7.1) | .003 |
| Fatigue | 713 | (6.6) | 65 | (10.5) | 648 | (6.3) | <.001 |
| Sputum production | 637 | (5.8) | 66 | (10.6) | 571 | (5.6) | <.001 |
| Rhinorrhea | 607 | (5.6) | 26 | (4.2) | 581 | (5.7) | .118 |
| Diarrhea | 597 | (5.5) | 43 | (6.9) | 554 | (5.4) | .108 |
| Arthralgia | 175 | (1.6) | 17 | (2.7) | 158 | (1.5) | .022 |
| Hemoptysis | 33 | (0.3) | – | – | 33 | (0.3) | .260 |
| COVID-19 severity, n (%) | <.001 | ||||||
| Mild | 6690 | (61.5) | 91 | (14.7) | 6599 | (65.1) | |
| Severe/critical | 4061 | (37.3) | 527 | (85.3) | 3534 | (34.9) | |
To include sensory ganglionitis, radiculitis, anterior horn syndrome, peripheral neuritis (GBS, other than GBS), neuromuscular disorder, myositis.
HIV: human immunodeficiency virus; CNS: central nervous system; PNS: peripheral nervous system; CVD: cerebrovascular disease; GBS: Guillain– Barre Syndrome.
Among patients with previous neurological history, cerebrovascular disease (12.2% vs 2.4%, P<.001), dementia (2.4% vs 0.2%, P<.001), epilepsy (1.3% vs 0.2%, P<.001), movement disorder (0.5% vs 0%, P=.003), and central nervous system (CNS) infection (0.3% vs 0%, P=.029) were more frequent in the encephalopathy group than in the no-encephalopathy group.
Encephalopathy is significantly associated with the development of new-onset CNS infection (0.64% vs 0.03%, P<.001), seizures (11.74% vs 0.51%, P<.001), and stroke or cerebrovascular events (11.74% vs 2.38%, P<.001) in patients with COVID-19 and encephalopathy, compared to those without encephalopathy.
The presence of cough (55% vs 39.7%, P<.001), fever (49.8% vs 35.3%, P<.001), dyspnea (49.4% vs 23.4%, P<.001), fatigue (10.5% vs 6.3%, P<.001), sputum production (10.6% vs 5.6%, P<.001), and arthralgia (2.7% vs 1.5%, P=.02) was more frequent among patients with encephalopathy than among those without encephalopathy.
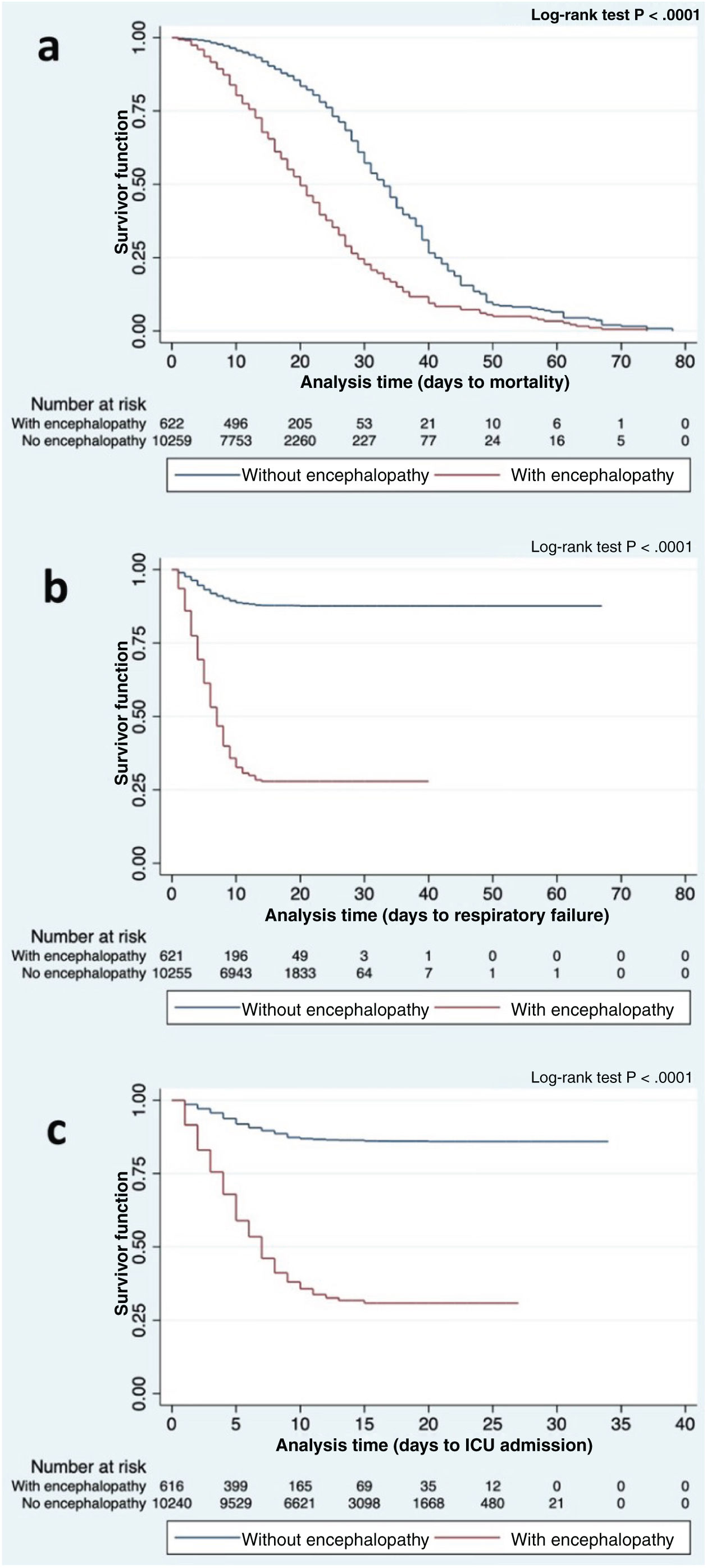
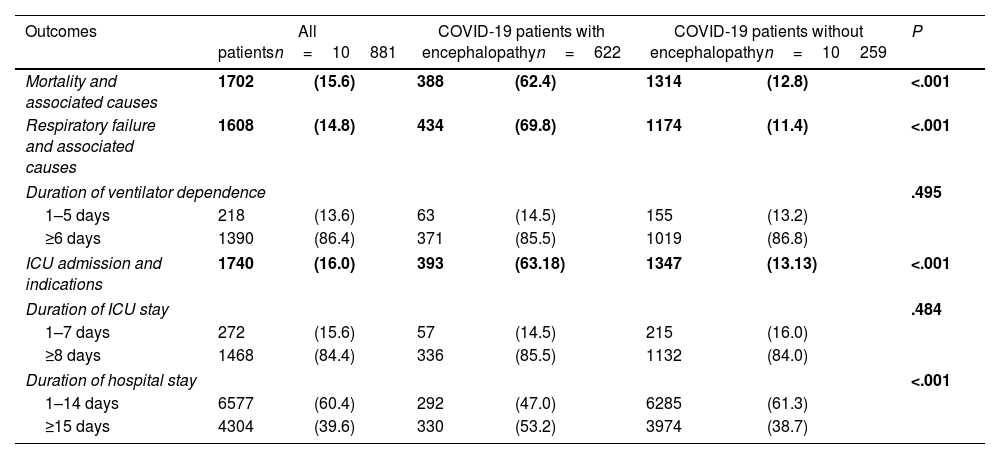
COVID-19 outcomesTable 2 summarizes the comparison of outcomes between the encephalopathy group and the no-encephalopathy group. Overall, mortality, respiratory failure, and number of ICU admissions were higher in the encephalopathy group compared to the no-encephalopathy group (P<.001). Table 3 shows the association between encephalopathy and the outcomes of interest. Fig. 2 shows the Kaplan–Meier curves for the encephalopathy and no-encephalopathy groups for mortality, respiratory failure, and ICU admission.
Comparison of outcomes in patients with COVID-19, with and without encephalopathy.
| Outcomes | All patientsn=10881 | COVID-19 patients with encephalopathyn=622 | COVID-19 patients without encephalopathyn=10259 | P | |||
|---|---|---|---|---|---|---|---|
| Mortality and associated causes | 1702 | (15.6) | 388 | (62.4) | 1314 | (12.8) | <.001 |
| Respiratory failure and associated causes | 1608 | (14.8) | 434 | (69.8) | 1174 | (11.4) | <.001 |
| Duration of ventilator dependence | .495 | ||||||
| 1–5 days | 218 | (13.6) | 63 | (14.5) | 155 | (13.2) | |
| ≥6 days | 1390 | (86.4) | 371 | (85.5) | 1019 | (86.8) | |
| ICU admission and indications | 1740 | (16.0) | 393 | (63.18) | 1347 | (13.13) | <.001 |
| Duration of ICU stay | .484 | ||||||
| 1–7 days | 272 | (15.6) | 57 | (14.5) | 215 | (16.0) | |
| ≥8 days | 1468 | (84.4) | 336 | (85.5) | 1132 | (84.0) | |
| Duration of hospital stay | <.001 | ||||||
| 1–14 days | 6577 | (60.4) | 292 | (47.0) | 6285 | (61.3) | |
| ≥15 days | 4304 | (39.6) | 330 | (53.2) | 3974 | (38.7) | |
ICU: intensive care unit.
Association between encephalopathy and the different outcomes of interest.
| Outcome | Adjusted OR | 95% CI | P |
|---|---|---|---|
| COVID-19 severity (severe/critical) | 7.95 | 6.27–10.06 | <.001 |
| Length of hospital stay (15 days or more) | 1.36 | 1.14–1.61 | <.001 |
| Length of ventilator dependence (6 days or more) | 0.88 | 0.64–1.21 | .428 |
| ICU admission | 4.26 | 3.77–4.80 | <.001 |
| Length of ICU admission (8 days or more) | 1.11 | 0.81–1.53 | .522 |
| Adjusted HR | 95% CI | P value | |
|---|---|---|---|
| Mortality | 1.72 | 1.53–1.94 | <.001 |
| Among patients with mild/moderate COVID-19 | 9.26 | 5.75–14.92 | <.001 |
| Among patients with severe/critical COVID-19 | 1.63 | 1.45–1.84 | <.001 |
| Respiratory failure | 5.40 | 4.80–6.07 | <.001 |
Adjusted for age, sex, hypertension, diabetes mellitus, smoking, coronary artery disease, cerebrovascular disease, dementia, epilepsy, and COVID-19 severity (as appropriate).
95% CI: 95% confidence interval; HR: hazard ratio; ICU: intensive care unit; OR: odds ratio.
Severe/critical COVID-19 was observed in a higher proportion of patients with encephalopathy, compared to the no-encephalopathy group (85.3% vs 34.9%, P<.001). After adjusting for confounders, those with encephalopathy were 7.95 times (95% CI, 6.27–10.06) more likely to present severe/critical COVID-19, among patients admitted with COVID-19.
Mortality and associated causesThe mortality rate was higher in the encephalopathy group (62.4%) than in the no-encephalopathy group (12.8%, P<.001). The risk of mortality was 1.72 times greater (95% CI, 1.53–1.94) in the encephalopathy group. Acute respiratory distress syndrome and septic shock were the most common causes of mortality. On stratified analysis, among patients with mild COVID-19, those with encephalopathy presented 9.26 times (95% CI, 5.75–14.92) greater mortality risk than those without encephalopathy. Among patients with severe/critical COVID-19, those with encephalopathy presented a risk of mortality 1.63 times (95% CI, 1.45–1.84) higher than those without encephalopathy. As seen in the Kaplan–Meier curve (Fig. 2), patients with COVID-19 and presenting encephalopathy had shorter survival times than those without encephalopathy (log-rank test, P<.001).
Respiratory failure and duration of ventilator dependenceThere was a higher frequency of respiratory failure in the encephalopathy group (69.8% vs 11.4%, P<.001), with an adjusted hazard ratio (HR) of 5.4 (95% CI, 4.8–6.07). Patients with COVID-19 and encephalopathy presented a shorter time to respiratory failure than those without encephalopathy (log-rank test, P<.001) (Fig. 2). Meanwhile, encephalopathy was not found to be associated with duration of ventilator dependence among patients with respiratory failure (P=.428).
ICU admissions and duration of ICU and hospital staysPatients with encephalopathy presented 4.26 times (95% CI, 3.77–4.80) greater risk of ICU admission. Among patients with encephalopathy, 63.2% were admitted to the ICU, compared to only 13.3% among the no-encephalopathy group (P<.001). Based on the Kaplan–Meier curve (Fig. 2), patients with COVID-19 and encephalopathy presented a shorter time to ICU admission compared to those without encephalopathy (log-rank test, P<.001). Those with encephalopathy tended to have longer hospital stays compared to the no-encephalopathy group, with 1.36 times (95% CI, 1.14–1.61) higher odds of staying 15 days or more in hospital.
However, there was no difference in the length of ICU stay between the encephalopathy and no-encephalopathy groups (P=.522).
DiscussionThe results of the Philippine CORONA Study identified encephalopathy as the most common new-onset neurological disorder among patients with COVID-19.3 Overall, our findings suggested that encephalopathy was associated with COVID-19 severity, mortality, respiratory failure, ICU admission, and longer hospital stays; this is consistent with findings of previous studies.8,15,16 It is worth mentioning that several studies on delirium and COVID-19 have also established an association with poor clinical outcomes, such as longer duration of mechanical ventilation and mortality.16–19
The 5.7% prevalence of encephalopathy in our cohort is comparable to the rates reported in the recent prospective, multicenter study in New York (6.8%)20 and in the TriNetX COVID-19 Research Network database consisting of 12601 hospitalized patients (8.7%).21 Other studies with smaller sample sizes reported rates of encephalopathy and/or delirium of up to 32–33%.15,16 In the ICU setting, a prospective study of 2 ICU cohorts comprising 140 patients from France reported a 79.5% incidence rate of delirium diagnosed with the Confusion Assessment Method-ICU score.17 These discrepancies in the rate of occurrence of encephalopathy may be due to differences in study design, sample size and demographic characteristics, ICU or special unit admission, and inclusion criteria. For instance, our cohort presented a high proportion of mild COVID-19 cases, which may explain the lower prevalence rate of encephalopathy.
Encephalopathy and delirium in patients with COVID-19 may be caused by a myriad of factors, such as metabolic, respiratory, and coagulation alterations caused either by the direct effects of SARS-CoV-2 on the brain, remote effects, or systemic inflammation affecting the blood-brain barrier.22 Older age, male sex, presence of comorbidities (hypertension, diabetes mellitus, kidney disease, coronary artery disease, malignancy, heart failure), smoking, and previous neurological history (cerebrovascular disease, dementia, epilepsy, movement disorders, CNS infection) were more frequent in the encephalopathy group compared to the no-encephalopathy group. These findings are congruent with those of 2 previous large-scale studies of COVID-19 patient cohorts.8,15 In the general acute medical setting, older age, male sex, and presence of cognitive disorder are among the known risk factors for encephalopathy.23 The higher incidence of encephalopathy among elderly patients and those with history of neurological disorders may be explained by decreased cognitive reserve, making the brain vulnerable to such insults as hypoxia and other metabolic alterations.24 Moreover, the majority of our patients in the encephalopathy group were elderly. Polypharmacy is also common in elderly people and can easily predispose to delirium, a feature of encephalopathy.23 Furthermore, studies in elderly patients with dementia found that delirium is a common initial presentation of COVID-19 in this population, and is associated with a higher mortality rate.18,25
Our findings showed that the adjusted HR for mortality among patients with encephalopathy was higher among patients with mild COVID-19 than among those with severe/critical COVID-19. The presence of encephalopathy may not have markedly contributed to the risk of mortality in patients with severe and critical COVID-19, as other factors such as presence of underlying diseases and several complications like acute respiratory distress syndrome, acute kidney injury, shock, secondary infections, and arrythmias were found to increase the risk of mortality among patients admitted to the ICU.26–28 The increased risk of mortality among patients with mild COVID-19 and encephalopathy suggests that encephalopathy may play a role as a prognostic marker.
Some results have shown that patients with encephalopathy present significantly higher rates of ICU admission than those without encephalopathy. ICU admissions, along with presentation of stupor or coma, have been shown in turn to be predictors of worse outcome at discharge,29 with patients aged>65 years having a markedly increased risk for persistent and new sequelae of various clinical conditions, including chronic respiratory failure, cardiac rhythm disorders, acute coronary syndrome, stroke, and kidney injury.30 Thus, further studies on the follow up of elderly patients with encephalopathy may be prudent to explore long-term complications of COVID-19.
In the current study, no association was observed between length of ICU stay and encephalopathy. Several factors influence length of ICU stay, such as social and institutional factors and the presence of a specialized team at the ICU31; as these factors were not taken into consideration during our data collection, the lack of association cannot be fully explained by our study.
The limitations of the present study lie in the retrospective nature of the research, due to the inherent risks of recording bias. The onset of encephalopathy, its duration, and correlation with other events such as sepsis, strokes, seizures, and the notorious cytokine storm would likewise clarify the underlying mechanism better. No additional data on cerebrospinal fluid were recorded. Nevertheless, this was the first large-scale nationwide study of COVID-19 in the Philippines, providing valuable information on the incidence of encephalopathy and its associations with clinical outcomes. A prospective study to reduce recording bias may provide more accurate data and remove confounding variables affecting the outcomes of COVID-19 patients with encephalopathy.
ConclusionOur study showed that encephalopathy was associated with COVID-19 severity, mortality, respiratory failure, ICU admission, and longer hospital stays. Further studies to determine specific risk factors for the development of encephalopathy in COVID-19 may help in improving the outcomes of patients admitted to hospital with COVID-19 in our setting.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This study used data from the Philippine CORONA Study which was funded by the (1) Philippine Neurological Association, Room 1006, Rear Tower Cathedral Height Building Complex, St. Luke's Medical Center, E. Rodriguez Avenue, Manila, Philippines (Grant number: Not applicable); and (2) Expanded Hospital Research Office, Philippine General Hospital, University of the Philippines Manila, Taft Avenue, Manila, Philippines (Grant number: Not applicable).
Institutional review board statementThe study was conducted in accordance with the Declaration of Helsinski, and approved by the local institutional review boards (code) of: Asian Hospital and Medical Center, Muntinlupa City (2020-010-A); Baguio General Hospital and Medical Center (BGHMC), Baguio City (BGHMC-ERC-2020-13); Cagayan Valley Medical Center (CVMC), Tuguegarao City; Capitol Medical Center, Quezon City; Cardinal Santos Medical Center (CSMC), San Juan City (CSMC REC 2020-020); Chong Hua Hospital, Cebu City (IRB 2420-04); De La Salle Medical and Health Sciences Institute (DLSMHSI), Cavite (2020-23-02-A); East Avenue Medical Center (EAMC), Quezon City (EAMC IERB 2020-38); Jose R. Reyes Memorial Medical Center, Manila; Jose B. Lingad Memorial Regional Hospital, City of San Fernando, Pampanga; Dr. Jose N. Rodriguez Memorial and Sanitarium Hospital, Caloocan City; Lung Center of the Philippines (LCP), Quezon City (LCP-CT-010-2020); Manila Doctors Hospital, Manila (MDH IRB 2020-006); Makati Medical Center, Makati City (MMC IRB 2020-054); Medical Center Manila, Manila (MMERC 2020-09); Northern Mindanao Medical Center, Cagayan de Oro City (025-2020); Quirino Memorial Medical Center (QMMC), Quezon City (QMMC REB GCS 2020-28); Ospital ng Makati, Makati City; Philippine General Hospital, University of the Philippines Manila (2020-314-01 SJREB); Philippine Heart Center, Quezon City; Research Institute for Tropical Medicine, Muntinlupa City (RITM IRB 2020-16); San Lazaro Hospital, Manila; San Juan De Dios Educational Foundation Inc – Hospital, Pasay City (SJRIB 2020-0006); Single Joint Research Ethics Board of the DOH, Philippines (SJREB-2020-24); Southern Isabela Medical Center, Santiago City (2020-03); Southern Philippines Medical Center (SPMC), Davao City (P20062001); St. Luke's Medical Center, Quezon City (SL-20116); St. Luke's Medical Center, Bonifacio Global City, Taguig City (SL-20116); Southern Philippines Medical Center, Davao City; The Medical City, Pasig City; University of Santo Tomas Hospital, Manila (UST-REC-2020-04-071-MD); University of the East Ramon Magsaysay Memorial Medical Center, Inc, Quezon City (0835/E/2020/063); Veterans Memorial Medical Center (VMMC), Quezon City (VMMC2020-025) and Vicente Sotto Memorial Medical Center, Cebu City (VSMMC-REC-O-2020-048).
Informed consent statementInformed consent was not necessary since the study design was a retrospective cohort study employing medical chart review. All data obtained were completely anonymized.
Submission declaration and verificationThis manuscript has never been published in part and is not under consideration for publication elsewhere. All authors have read and agreed to the published version of the manuscript. If accepted, this manuscript will not be published elsewhere in the same form, in English or in any other language, including electronically, without the consent of the copyright holder.
Conflict of interestNone.
Data availability statementData not published within this article are available upon request from the corresponding author.
Statement on artificial intelligence and artificial intelligence-assisted technologiesDuring the preparation of this work the primary authors only used ChatGPT to translate the title, abstract, and keywords from English to Spanish. After using this tool/service, the primary authors reviewed and edited the Spanish translation of the title, abstract, and keywords and take full responsibility for the content of the publication.
The authors would like to thank The Philippine CORONA Study Group Investigators and their respective hospital sites for their contribution in the data collection: Asian Hospital and Medical Center, Muntinlupa City (Corina Maria Socorro A. Macalintal, MD; Joanne B. Robles, MD), Baguio General Hospital and Medical Center, Baguio City (Paulo L. Cataniag, MD; Manolo Kristoffer C. Flores, MD, MBA), Cagayan Valley Medical Center, Tuguegarao City (Noreen Jhoanna T. Trinidad, MD), Capitol Medical Center, Quezon City (Dan Neftalie A. Juangco, MD; Giuliani Renz G. Paas, MD), Cardinal Santos Medical Center, San Juan City (Audrey Marie U. Chua, MD, Valmarie S. Estrada, MD, Philip Rico P. Mejia, MD, Therese Franz B. Reyes, MD), Chong Hua Hospital, Cebu City (Maria Teresa A. Cañete, MD; Ferdinand Renfred A. Zapata, MD), De La Salle University Medical and Health Sciences Institute, Dasmariñas City, (Franko Eugenio B. Castillo, MD; Romulo U. Esagunde, MD; Jean B. Gantioque, MD), Dr. Jose N. Rodriguez Memorial and Sanitarium Hospital, Caloocan City (Maritoni C. Abbariao, MD; Geramie M. Acebuque, MD), Dr. Pablo O. Torre Memorial Hospital, Bacolod City (Evram V. Corral, MD), East Avenue Medical Center, Quezon City (Marian Irene C. Escasura, MD; Marissa T. Ong, MD), Jose B. Lingad Memorial Regional Hospital, City of San Fernando (Arnold Angelo M. Pineda, MD; Khasmeen D. Aradani, MD), Jose R. Reyes Memorial Medical Center, Manila (Joseree-Ann S. Catindig, MD; Mark Timothy T. Cinco, MD; Mark Erving H. Ramos, MD), Lung Center of the Philippines, Quezon City (Romulus Emmanuel H. Cruz, MD; Marita B. Dantes, MD; Norberto A. Francisco, MD; Rosalia A. Teleg, MD), Makati Medical Center, Makati City (Krisverlyn B. Bellosillo, MD; Jean Paolo M. Delfino, MD; Cid Czarina E. Diesta, MD; Rosalina E. Picar, MD; Julie Anne V. Gamboa, MD; Cara Camille M. Matute, MD; Franzelle P. Padilla, MD; John Joshua Q. Punsalan, MD), Manila Doctors Hospital, Manila (Ma. Epifania V. Collantes, MD; Charmaine B. Que, MD; Hanifa A. Sampao, MD; Maxine Camela S. Sta. Maria, MD), Medical Center Manila, Manila (Marita M. Fuentes, MD; Jennifer Justice F. Manzano, MD; Rizza J. Umali, MD), New Era General Hospital, Quezon City (Marc Conrad C. Molina, MD), Northern Mindanao Medical Center, Cagayan de Oro City (Hazel Claire M. Ang, MD; Arturo F. Surdilla, MD; Loreto P. Talabucon Jr., MD; Natasha F. Wabe, MD), Ospital ng Makati, Makati City (Christian Paul B. Banday, MD; Christopher C. Cipriano, MD; Nehar A. Pangandaman, MD; Avery Gail C. Wasil, MD), Perpetual Succor Hospital, Cebu City (Elrey P. Inocian, MD; Jarungchai Anton S. Vatanagul, MD), Philippine General Hospital, Manila (Almira Doreen Abigail O. Apor, MD; Carissa Paz C. Dioquino, MD), Philippine Heart Center, Quezon City (Prinz Andrew M. Dela Cruz, MD; Maricar P. Yumul, MD), Quirino Memorial Medical Center, Quezon City (Maria Victoria G. Manuel, MD; Al Inde John A. Pajantoy, MD; Josephine Cecilia V. Roque, MD; Paul Emmanuel L. Yambao, MD), Research Institute for Tropical Medicine, Muntinlupa City (Ma. Alma C. Concepcion, MD), San Juan De Dios Educational Foundation Inc. Hospital, Pasay City (Ma. Caridad V. Desquitado, MD; Carl Kevin L. Julao, MD), San Lazaro Hospital, Manila (Dante P. Bornales, MD), Southern Isabela Medical Center, Santiago City (Generaldo D. Maylem, MD; Mark Joseph F. Cuntapay, MD), Southern Philippines Medical Center, Davao City (Annabelle Y. Lao-Reyes, MD; Aileen Mae B. Lee, MD; Nadia O. Manlegro, MD; Dave Mar L. Pelere, MD), St. Luke's Medical Center – Global City, Taguig City (Lina C. Laxamana, MD; Diana-Lynn S. Que, MD; Jeryl Ritzi T. Yu, MD), St. Luke's Medical Center, Quezon City (Ma. Socorro C. Martinez, MD; Alexandria E. Matic, MD; John Angelo Luigi S. Perez, MD), The Medical City, Pasig City (Glenn Anthony A. Constantino, MD; Aldanica R. Olano, MD; Liz Edenberg P. Quiles, MD; Artemio A. Roxas, Jr., MD; Jo Ann R. Soliven, MD; Michael Dorothy Frances Montojo-Tamayo, MD), University of Santo Tomas Hospital, Manila (Ma. Lourdes C. Joson, MD; Jojo R. Evangelista, MD), University of the East Ramon Magsaysay Memorial Medical Center Inc., Quezon City (Ma. Clarissa B. Nuñez, MD; Marietta C. Olaivar, MD; Dominique Q. Perez, MD), Veterans Memorial Medical Center, Quezon City (Mark Deneb O. Armeña, MD; Robert A. Barja, MD), Vicente Sotto Memorial Medical Center, Cebu City (Joshua Emmanuel E. Abejero, MD; Maritzie R. Eribal, MD), Western Visayas Medical Center, Iloilo City (Ryndell G. Alava, MD), Zamboanga City Medical Center, Zamboanga City (Muktader A. Kalbi, MD; Nasheera W. Radja, MD; Mohammad Elshad S. Sali, MD).