Multiple studies of attention deficit hyperactivity disorder (ADHD) have recognised a heritability factor in that a higher frequency of the disorder is observed in children with an affected relative. Our aim was to determine the association between ADHD symptoms in young children enrolled in five schools in Bogota and a history of ADHD symptoms in their parents using the Wender-Utah Rating Scale.
MethodologyCase–control study of participants selected according to DSM-IV criteria for ADHD and the Behavioral Assessment System for Children (BASC) completed by parents and teachers; the WISC-IV scale was used to exclude children with cognitive deficit. Parents completed the Wender-Utah Rating Scale to retrospectively identify any ADHD symptoms in childhood. A score of 36 was used as a cut-off point.
ResultsThe study included 202 children: 117 cases and 85 controls. A positive history of ADHD symptoms in childhood was identified for 16% of 175 mothers and 20.6% of 141 fathers. The presence of symptoms in either parent, especially the mother, constitutes a significant risk factor for ADHD in children and this relationship persists after controlling for different variables. If both parents have the disorder, the risk tends to increase.
ConclusionAlthough ADHD has been linked to a genetic component, other environmental factors may be involved in the disorder.
En el trastorno por déficit de atención e hiperactividad (TDAH), la heredabilidad ha sido reconocida en múltiples estudios. En este sentido, se ha observado una mayor frecuencia del trastorno en niños con familiares afectados. El objetivo fue determinar la asociación entre la presencia de síntomas de TDAH en niños escolares de 5 instituciones educativas de Bogotá y el antecedente de síntomas de TDAH en sus padres utilizando el cuestionario de Wender-Utah.
MetodologíaEstudio de casos y controles seleccionados de acuerdo con los criterios DSM-IV para TDAH, la escala multifuncional de la conducta (BASC) para padres y maestros y WISC-IV para descartar déficit cognitivo. A los padres se les aplicó un cuestionario de Wender-Utah para identificar de manera retrospectiva síntomas de TDAH en su infancia. Un score de 36 fue tomado como punto de corte.
ResultadosDe 202 niños disponibles, 117 fueron casos y 85 controles. Un 16% de 175 madres y un 20,6% de 141 padres tuvieron antecedentes positivos para síntomas de TDAH en la infancia. La presencia de síntomas en alguno de los progenitores, principalmente en la madre, es un factor de riesgo significativo para la presencia de TDAH en los niños y esta relación persiste si se controla por diferentes variables. Si los 2 progenitores tienen el cuadro, existe una tendencia a que el riesgo aumente.
ConclusiónA pesar de que el TDAH se ha asociado a un componente genético, otros factores del entorno pueden estar involucrados en la génesis del trastorno.
Attention-deficit/hyperactivity disorder (ADHD) is a behavioural disorder characterised by lack of attention, increased motor activity, and impulsiveness. Prevalence in the general population ranges between 5% and 20% depending on the series.1–5
Although this disorder is specific to children, its symptoms and functional deficits may persist into adulthood in 60% of all patients, as follow-up studies show us.6–8 Prevalence in adults ranges from 2.5% to 4.7%.9–12 We do not know which risk factors distinguish children with ADHD whose condition may persist, but associations have been reported with late onset of treatment, more severe symptoms, and the presence of psychiatric comorbidities including personality disorders.13,14
Genetic factors have often been implicated in ADHD aetiology. The disorder is multifactorial, and its estimated heritability is approximately 76%.15 This being the case, the children of a parent affected by ADHD have a 50% chance of exhibiting the same symptoms.16 Assessment of children whose parents were diagnosed with ADHD revealed that 57% of the children met ADHD criteria, and 75% of that latter group were treated for it.16 When using the DSM-IV to diagnose children with ADHD and oppositional behaviours, Smalley et al.17 found a significant association with the presence of one affected parent in 55% of the cases; at 63%, this association was more pronounced in girls than in boys. Nevertheless, we cannot overlook the role of environmental factors in the genesis and maintenance of the disorder over the patient's lifetime.18 It is also possible that children with more severe cases will be more likely to have a parent with ADHD.19
There is no specific and objective marker by which ADHD can be evaluated in children or in adults.2,20 In addition to interviews and direct observation, doctors use evaluation scales with standardised, adapted criteria; some such scales have been translated and validated in Spanish.21 The general medical history can be assessed with Conners’ Adult ADHD Diagnostic Interview for DSM-IV part I(CAADID); current ADHD symptoms, using part II of the CAADID, the Barkley Adult ADHD Rating Scale-IV, Adult Self-Report Scale (ASRS), the Conners’ Adult ADHD Rating Scales (CAARS), and Adult ADHD-Symptom Rating Scale; and the retrospective evaluation of childhood ADHD symptoms, with the Wender-Utah Rating Scale (WURS) and the ADHD-Symptom Rating Scale. Numerous authors have found the WURS to be useful not only for retrospective evaluation of ADHD in adults, but also for detecting related factors or comorbidities.22,23 Furthermore, it provides an interesting model for evaluating the relationship between polymorphisms of candidate genes and ADHD, as established by Pazvantoğlu et al.24 in a study of 228 parents of 146 children with the disorder.
The purpose of the present study is to determine the association between presence of ADHD symptoms in school-age children attending five educational centres in Bogotá and a history of ADHD symptoms in their parents, using the WURS.20,25
Subjects and methodsWe performed a preliminary case–control study in a sample of lower to middle-class students from public and private schools in Bogotá, Colombia to assess symptoms of ADHD.3,26,27 ADHD was diagnosed according to the DSM-IV checklist and the multidimensional Behavior Assessment System for Children (BASC). We then assessed the children on the WISC IV to exclude any with cognitive deficit (cut-off point for total IQ<70). Controls were selected from among children who attended the same school but did not exhibit ADHD or cognitive impairment.
The parents of cases and controls who were able to participate agreed to sign an informed consent form and take a questionnaire. They then completed the WURS survey as a retrospective means of detecting any childhood history of ADHD.
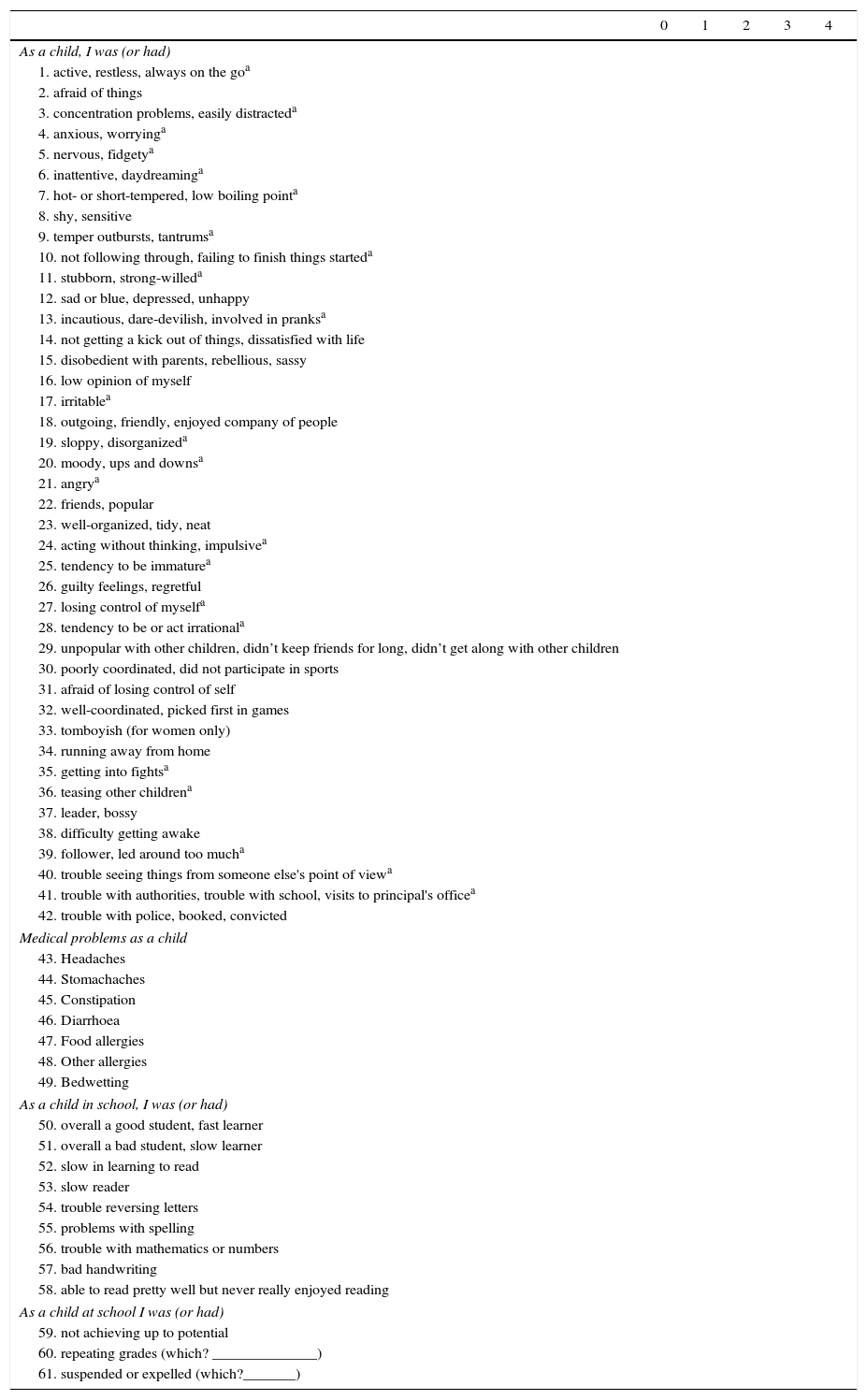
WURS is a 61-item self-assessment scale that examines the following criteria: attention difficulties, hyperactivity, impulsivity, emotional problems, and behavioural problems. All items continued from the heading, ‘As a child, I was (or had)…’. This scale was translated, adapted, and validated for the Spanish population by Rodriguez-Jimenez et al.25 in 2001 (Appendix 1). The validation study for Colombia, performed by Pineda et al.,28 showed that when using the score from all 25 items and a cut-off point of 35.5, the specificity is higher than 90%, although sensitivity is only about 46%. In this study, a score of 36 or higher is considered positive for ADHD.29
The sample size was calculated to accommodate a 23.1% reference prevalence for symptoms among parents of children with ADHD, and a reference prevalence of 3.8% among parents of healthy children.30 After adjusting for losses to follow-up, we obtained a minimum sample size of 128 subjects, or 64 cases and 64 controls, to yield a statistical power of 80% and a confidence interval of 95%.
Information was analysed using SPSS version 20.0 for Windows. Frequency distributions and percentages were used in the descriptive analysis of qualitative variables. Measures of central tendency and variability and their respective coefficients of variation were used to measure data homogeneity in quantitative variables (t-test was used for homogeneous samples). In addition, we evaluated a child's risk of having ADHD given the presence of that disease in a parent using the odds ratio (OR) and the corresponding 95% confidence interval (95% CI). Quantitative variables were compared using the t-test for the means of two independent groups, after using the Levene test to verify that the groups met the assumption of normality with P>.05. Where the Kolmogorov–Smirnov test did not show a normal distribution, the non-parametric Mann–Whitney U test was used to assess the difference between cases and controls. Lastly, a forward stepwise bi/multinomial regression analysis was performed to determine which variables would have affected ADHD status in each child if a parent had also presented ADHD in childhood. The level of statistical significance was set at 5% (P<.05).
This was a no-risk study which complied with our country's legal and ethical directives as well as those stated in the latest version of the World Medical Association's Declaration of Helsinki. Families participated voluntarily and the parents of all participating children signed an informed consent form; children also assented. The study was approved by our Ethics Committee for Institutional Research, and school authorities gave permission for students to be assessed at their educational centres. All data and records generated were stored in such a way as to maintain the subjects’ confidentiality.
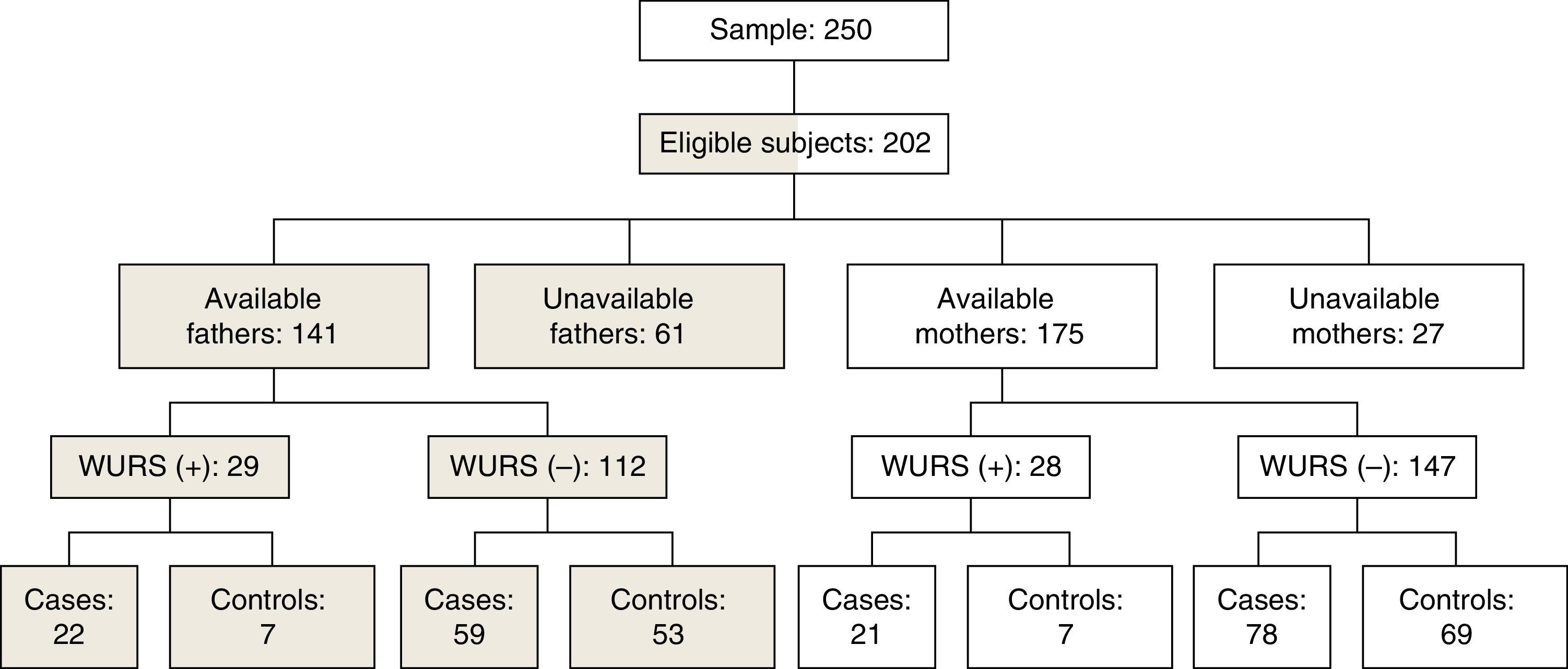
ResultsThe parents of 250 children signed informed consent forms for the study. Of this number, 37 were excluded due to data being incomplete or inconclusive for ADHD; and 11 due to having an IQ below 70. The final sample consisted of 202 children (146 boys and 56 girls): there were 117 cases and 85 controls (Fig. 1). According to the criteria established based on the BASC and the checklist, 107 cases could be classified into ADHD subgroups: 35 presented symptoms of lack of attention, 11 of hyperactivity/impulsivity, and 61 of a mixed disorder.
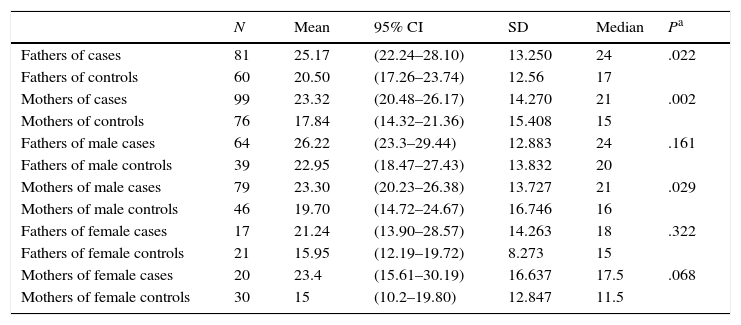
The WURS was applied to 175 mothers and 141 fathers; mean scores on this scale were 20.94 (95% CI, 18.71–23.18) and 23.18 (95% CI, 21–25.37) for each sex respectively. The means and medians in the parent group were significantly higher among mothers (P=.002) than among fathers (P=.022). The analysis of index cases broken down by the sex of the parent showed the same tendency, although differences were only significant for the mothers of male children (Table 1).
Parents’ mean score on WURS. Differences between cases/controls, differences between sexes.
| N | Mean | 95% CI | SD | Median | Pa | |
|---|---|---|---|---|---|---|
| Fathers of cases | 81 | 25.17 | (22.24–28.10) | 13.250 | 24 | .022 |
| Fathers of controls | 60 | 20.50 | (17.26–23.74) | 12.56 | 17 | |
| Mothers of cases | 99 | 23.32 | (20.48–26.17) | 14.270 | 21 | .002 |
| Mothers of controls | 76 | 17.84 | (14.32–21.36) | 15.408 | 15 | |
| Fathers of male cases | 64 | 26.22 | (23.3–29.44) | 12.883 | 24 | .161 |
| Fathers of male controls | 39 | 22.95 | (18.47–27.43) | 13.832 | 20 | |
| Mothers of male cases | 79 | 23.30 | (20.23–26.38) | 13.727 | 21 | .029 |
| Mothers of male controls | 46 | 19.70 | (14.72–24.67) | 16.746 | 16 | |
| Fathers of female cases | 17 | 21.24 | (13.90–28.57) | 14.263 | 18 | .322 |
| Fathers of female controls | 21 | 15.95 | (12.19–19.72) | 8.273 | 15 | |
| Mothers of female cases | 20 | 23.4 | (15.61–30.19) | 16.637 | 17.5 | .068 |
| Mothers of female controls | 30 | 15 | (10.2–19.80) | 12.847 | 11.5 |
Given a cut-off point of 36 on the WURS, 16% of the mothers tested positive for a history of ADHD (Fig. 1). There was a statistically significant association between presence of ADHD in children and presence of ADHD in their mothers in the group of cases (P=.002). The risk of having a child with the disorder if the mother tested positive on the WURS was 2.65 times as high (95% CI, 1.063–6.624). The logistic regression model adjusted for the children's sex, type of school, age, and level continued to show a significant relationship between positivity for ADHD on the WURS in the mother and presence of ADHD in her child (P=.049). Total IQ did not affect this model.
Additionally, 20.6% of the children's fathers were identified as having ADHD according to the WURS (Fig. 1). We identified an association between a positive result for parents of children with ADHD that was not present in controls (P=.022); given a father with ADHD, the child's risk of having the disorder is 2.82 times greater (95% CI, 1.12–7.14). The logistic regression model adjusted for the children's sex continued to show a significant relationship between WURS-positive ADHD in the father and presence of ADHD in his child (P=.049). The child's age, type of school, total IQ, and level did not affect the model.
The analysis of a history of ADHD affecting one or both parents showed that if this condition was met, the child's risk was 2.579 times as high (95% CI, 1.223–5.441). Risk was even higher when both parents had a history of ADHD (OR=3.688, 95% CI, 0.420–32.400); nevertheless, the sample size (n=6) was too small to affirm that these differences were significant.
Evaluating ADHD subgroups using a multinomial logistic regression model revealed that history of the disorder in the patient's mother was related to the mixed disorder after adjusting for sex, age, type of school, and grade level (P=.033). In contrast, fathers with the disorder showed an association with the inattentive subgroup after controlling for sex, age, and grade level (P=.046). If one of the two parents had a history of the disorder, that condition was associated with the mixed ADHD subtype after controlling for sex (P=.037), grade level (P=.044), or type of school (P=.039).
DiscussionADHD is a childhood-onset condition that remains present throughout the patient's life; it has multiple consequences for academic and job performance and in family and other social settings. Its origin has to do with multiple factors, ranging from the environmental to the genetic.
Parental history of ADHD in children presenting the same disorder has been described in earlier studies31,32 and the heritability pattern has been shown to be between 65% and 75%.33 Evaluating the association between children with ADHD and the possibility that one of their parents also had it will help researchers draw up strategies with clear academic recommendations.
Tools that can be used to assess the familial component of this disorder are currently available. Nevertheless, results have been highly variable; this may be due to the diagnostic methods, sources of information (parents, teachers, carers) and to social and cultural variables (sex, ethnicity, type of population, place of residence, socioeconomic level). Using the WURS to retrospectively identify any history of ADHD in the parents may be useful; it can be applied quickly and its sensitivity and specificity are sufficient to ensure a reliable screening.20,25,34 One of the limitations of using this scale is recall bias, since symptoms of lack of attention, hyperactivity, and impulsivity generally appear before the age of 7. Likewise, it is possible that the parents were not observed to have symptoms, mainly attention-related symptoms, or other associated traits.
A cut-off point of 36 on the WURS identified 16% of the mothers and 20.06% of the fathers as having had symptoms of attention deficit or hyperactivity as children. These results were similar to those reported by Romero Ogawa et al.30 in a study with a similar population and methodology; here, WURS results showed that 23% of the fathers and 19% of the mothers scored positive for ADHD.
Genetic factors have been identified as part of the aetiology of ADHD.35,36 This study of parents and children showed that ADHD has a significant heritable component. For that reason, a diagnosis of ADHD in one of the parents is a factor to be considered during the child's growth and development assessments. When using the DSM-IV to diagnose children with ADHD and oppositional behaviours, Smalley et al.17 found a significant association between having ADHD and the presence of one affected parent in 55% of the total cases; at 63%, this association was more pronounced in girls than in boys, indicating that a more marked family influence is required for girls to develop the disorder. It is not common for both parents to score positive on the WURS, as our study shows, but this situation could compound the risk.
Furthermore, the presence of environmental and social factors could precipitate and aggravate ADHD symptoms. Disruptive family environments or those affected by psychosocial disadvantages including poverty, parental mental illness, conflictive relationships, and unemployment, contribute to this disorder manifesting in susceptible children.37–39 This being said, it is interesting that our study would detect a higher risk of ADHD when the mother was the affected parent. The explanation might be that the mother, whose actions modulate the child's behaviour, might fail to intervene correctly if she herself is affected by an attention deficit disorder. One of the limitations of this study was that fewer fathers than mothers participated, and this might be a source of bias in the study, considering that the syndrome is more prevalent in men than in women. It is possible that the number of fathers who chose not to participate masks a high number of cases with persistent symptoms of attention deficit and hyperactivity.
On the other hand, ADHD interferes in proper behavioural development and may be associated with different behaviours that are disruptive for society. Studies of adult subjects exhibiting alcoholism or delinquency clearly show a high frequency of ADHD cases in childhood. Ponce Alfaro et al. studied alcoholic patients assessed on the WURS to estimate the frequency of possible cases of childhood ADHD. They found that a large percentage of alcoholic patients had high scores on the WURS, which is indicative of ADHD symptoms in childhood.40 On the other hand, Vegue-Gonzalez et al.,13 who studied a population of 100 prison inmates in order to measure the prevalence of childhood ADHD and investigate any associations with behavioural disorders, used the WURS and determined that 50% of the cases they evaluated met the criteria for ADHD in childhood.
Considering that suspected ADHD cases in the case–control study were first identified based on parent-reported questionnaires, we might ask whether fathers and mothers with WURS-positive ADHD might be more tolerant of their children's behaviour. If this is the case, they may have evaluated them less strictly than other parents did, meaning that these children would have been excluded from the ADHD group. Based on the above, we stress that detection, recognition, and treatment of ADHD are important steps at all levels of development and at any time of life. This disorder will have a significant impact not only on the patient, but on all members of the patient's family.2 We therefore deem it necessary to continue researching associations with heredity in ADHD and identify the tools with the greatest sensitivity and specificity in order to deliver more useful answers and approaches.
Regarding therapy, we recommend psychosocial interventions with a cognitive-behavioural approach that will recognise the key role parents play in the treatment of their children. This training should include areas including education in issues related to the disorder, understanding parent–child relationships, teaching effective communication skills that promote positive behaviour, and increasing student motivation through the use of reward systems for good behaviour and time-outs for undesirable behaviour.
In conclusion, although ADHD has a major genetic component, other environmental factors may be involved in the emergence of the disorder. This study found a significant association between ADHD and the probability of a parent testing positive on the WURS; risk was 2.36 times higher. This association remains after adjusting by different variables. The WURS is a useful tool for evaluating adults and it should be applied when we diagnose a child with ADHD. If the parent tests positive, the best approach is to provide an integral treatment that involves all family members.
FundingThis article forms part of the research project titled ‘Caracterización familiar, molecular y evaluación de la función ejecutiva en población escolar diagnosticada con déficit de atención e hiperactividad’ and financed by the Foundation for the Promotion of Research and Technology at the Bank of the Republic of Colombia, the Research Fund of Universidad del Rosario (FIUR), and Universidad del Rosario.
Conflicts of interestThe authors have no conflicts of interest to declare.
| 0 | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| As a child, I was (or had) | |||||
| 1. active, restless, always on the goa | |||||
| 2. afraid of things | |||||
| 3. concentration problems, easily distracteda | |||||
| 4. anxious, worryinga | |||||
| 5. nervous, fidgetya | |||||
| 6. inattentive, daydreaminga | |||||
| 7. hot- or short-tempered, low boiling pointa | |||||
| 8. shy, sensitive | |||||
| 9. temper outbursts, tantrumsa | |||||
| 10. not following through, failing to finish things starteda | |||||
| 11. stubborn, strong-willeda | |||||
| 12. sad or blue, depressed, unhappy | |||||
| 13. incautious, dare-devilish, involved in pranksa | |||||
| 14. not getting a kick out of things, dissatisfied with life | |||||
| 15. disobedient with parents, rebellious, sassy | |||||
| 16. low opinion of myself | |||||
| 17. irritablea | |||||
| 18. outgoing, friendly, enjoyed company of people | |||||
| 19. sloppy, disorganizeda | |||||
| 20. moody, ups and downsa | |||||
| 21. angrya | |||||
| 22. friends, popular | |||||
| 23. well-organized, tidy, neat | |||||
| 24. acting without thinking, impulsivea | |||||
| 25. tendency to be immaturea | |||||
| 26. guilty feelings, regretful | |||||
| 27. losing control of myselfa | |||||
| 28. tendency to be or act irrationala | |||||
| 29. unpopular with other children, didn’t keep friends for long, didn’t get along with other children | |||||
| 30. poorly coordinated, did not participate in sports | |||||
| 31. afraid of losing control of self | |||||
| 32. well-coordinated, picked first in games | |||||
| 33. tomboyish (for women only) | |||||
| 34. running away from home | |||||
| 35. getting into fightsa | |||||
| 36. teasing other childrena | |||||
| 37. leader, bossy | |||||
| 38. difficulty getting awake | |||||
| 39. follower, led around too mucha | |||||
| 40. trouble seeing things from someone else's point of viewa | |||||
| 41. trouble with authorities, trouble with school, visits to principal's officea | |||||
| 42. trouble with police, booked, convicted | |||||
| Medical problems as a child | |||||
| 43. Headaches | |||||
| 44. Stomachaches | |||||
| 45. Constipation | |||||
| 46. Diarrhoea | |||||
| 47. Food allergies | |||||
| 48. Other allergies | |||||
| 49. Bedwetting | |||||
| As a child in school, I was (or had) | |||||
| 50. overall a good student, fast learner | |||||
| 51. overall a bad student, slow learner | |||||
| 52. slow in learning to read | |||||
| 53. slow reader | |||||
| 54. trouble reversing letters | |||||
| 55. problems with spelling | |||||
| 56. trouble with mathematics or numbers | |||||
| 57. bad handwriting | |||||
| 58. able to read pretty well but never really enjoyed reading | |||||
| As a child at school I was (or had) | |||||
| 59. not achieving up to potential | |||||
| 60. repeating grades (which? ______________) | |||||
| 61. suspended or expelled (which?_______) | |||||
These 25 items were selected based on their ability to distinguish patients with ADHD in childhood.
0: not at all or very slightly; 1: mildly; 2: moderately; 3: quite a bit; 4: very much.
Source: Rodriguez-Jimenez et al.25
Please cite this article as: Vélez-van-Meerbeke A, Talero-Gutiérrez C, Zamora-Miramón I, Guzmán-Ramírez GM. Trastorno por déficit de atención e hiperactividad: de padres a hijos. Neurología. 2017;32:158–165.