In-hospital consultations (IHCs) are essential in clinical practice in tertiary hospitals. The aim of this study is to analyse the impact of neurological IHCs.
Patients and methodOne-year retrospective descriptive study of neurological IHCs conducted from May 2013 to April 2014 at our tertiary hospital.
ResultsA total of 472 patients were included (mean age, 62.1 years; male patients, 56.8%) and 24.4% had previously been evaluated by a neurologist. Patients were hospitalised a median of 18 days and 19.7% had been referred by another hospital. The departments requesting the most in-hospital consultations were intensive care (20.1%), internal medicine (14.4%), and cardiology (9.1%). Reasons for requesting an IHC were stroke (26.9%), epilepsy (20.6%), and confusional states (7.6%). An on-call neurologist evaluated 41.9% of the patients. The purpose of the IHC was to provide a diagnosis in 56.3% and treatment in 28.2% of the cases; 69.5% of the patients required additional tests. Treatment was adjusted in 18.9% of patients and additional drugs were administered to 27.3%. While 62.1% of cases required no additional IHCs, 11% required further assessment, and 4.9% were transferred to the neurology department. Of the patient total, 16.9% died during hospitalisation (in 37.5%, the purpose of the consultation was to certify brain death); 45.6% were referred to the neurology department at discharge and 6.1% visited the emergency department due to neurological impairment within 6 months of discharge.
ConclusionsIHCs facilitate diagnosis and management of patients with neurological diseases, which may help reduce the number of visits to the emergency department. On-call neurologists are essential in tertiary hospitals, and they are frequently asked to diagnose brain death.
Las consultas intrahospitalarias (IC) son fundamentales en la actividad asistencial dentro de un hospital de tercer nivel. El objetivo de este estudio es analizar y cuantificar el impacto de las mismas.
Pacientes y métodoEstudio descriptivo retrospectivo de las IC realizadas a Neurología durante un año (período: mayo del 2013-abril del 2014) en nuestro centro.
ResultadosSe incluyó a 472 pacientes (edad media 62,1, varones 56,8%). Previamente, el 24,4% había sido valorado por un neurólogo. Mediana de 18 días de ingreso y el 19,7% de ellos fueron derivados desde otro hospital. Servicios más demandantes: Medicina Intensiva 20,1%, Medicina Interna 14,4% y Cardiología 9,1%. Motivos IC: ictus 26,9%, epilepsia 20,6% y cuadros confusionales 7,6%. El 41,9% fue valorado por un neurólogo de guardia. Objetivo IC: diagnóstico 56,3% y tratamiento 28,2%. En el 69,5% de los casos fueron necesarias pruebas complementarias. En el 18,9% se ajustó el tratamiento y se introdujo al menos un medicamento en 27,3%. El 62,1% de las IC se resolvieron con una valoración. El 11% precisó revaluación y un 4,9% fue trasladado a Neurología. El 16,9% delos pacientes fallecieron durante ingreso (de ellos, en el 37,5% el motivo fue el diagnóstico de muerte encefálica). El 45,6% fue derivado a Neurología al alta y consultó en Urgencias un 6,1% por motivos neurológicos en los 6 meses posteriores al alta.
ConclusionesLas IC facilitan el diagnóstico y el manejo de pacientes con enfermedades neurológicas, posiblemente disminuyendo las consultas de estos pacientes en Urgencias. En un hospital terciario, es destacable la labor del neurólogo de guardia y la importancia del diagnóstico de muerte encefálica.
Scientific advances in neurology in recent years and the increasing prevalence of neurological diseases due to population ageing (between 13% and 16% of the Spanish population was older than 65 in 20061) underscore that doctors from other specialties need support when managing neurological patients.
In a tertiary hospital, the common means of requesting support is through the in-hospital consultation system. In an in-hospital consultation, the requesting doctor addresses his request to a consultant who must focus on resolving the problem in the most efficient way possible, bearing in mind that the core purpose of this collaborative effort is the patient's well-being. Where possible, the patient should understand the reason for the in-hospital consultation and the role played by each doctor.
In common practice, little value is placed on consulting work, which is normally undertaken at the expense of other activities, such as specialist consultations, the labours of the on-call neurologist, or research. Although these consultations are essential for hospitals to function correctly, little importance is attached to learning how to perform this activity properly. Most doctors learn by trial and error, and the interpretations of consultants frequently differ from those of the requesting doctors.2
Hospital Universitari Vall d’Hebron is a tertiary care hospital with more than 1000 beds and providing care to a population of more than 400000 inhabitants. This is a national and international centre of reference in different areas. The department of neurology has a 24-hour on-call neurologist and provides other hospital departments with a rotating consultation service consisting of senior doctors and residents.
The aim of this study is to describe and analyse the activities carried out by this team, which works in a specific setting. Furthermore, we deemed it relevant to quantify this activity and try to better understand it with a view to improving daily practice, the relationships between different departments, and care for our patients.
Patients and methodsWe conducted a retrospective, descriptive study of the in-hospital consultations performed by the neurology department at Hospital Universitari Vall d’Hebron over one year (May 2013–April 2014). We assessed a total of 472 patients and reviewed all their medical histories to record different variables (demographic, administrative, care-related, and mortality-related). During this period, our department admitted 1328 patients.
Statistical analysis was performed using SPSS software version 17.0. Results from the descriptive analysis are shown as number of cases (percentage), mean±standard deviation, or median (interquartile range), according to the distribution of each variable.
The chi-square test was used to compare categorical variables. Continuous variables were compared using the t-test except for those whose distribution is not approximately normal, which were compared using the Mann–Whitney U test.
Differences with a significance level below .05 were considered statistically significant. Specific diagnoses were considered to be those diagnoses with a clearly defined aetiology and treatment and provided by neurologists.
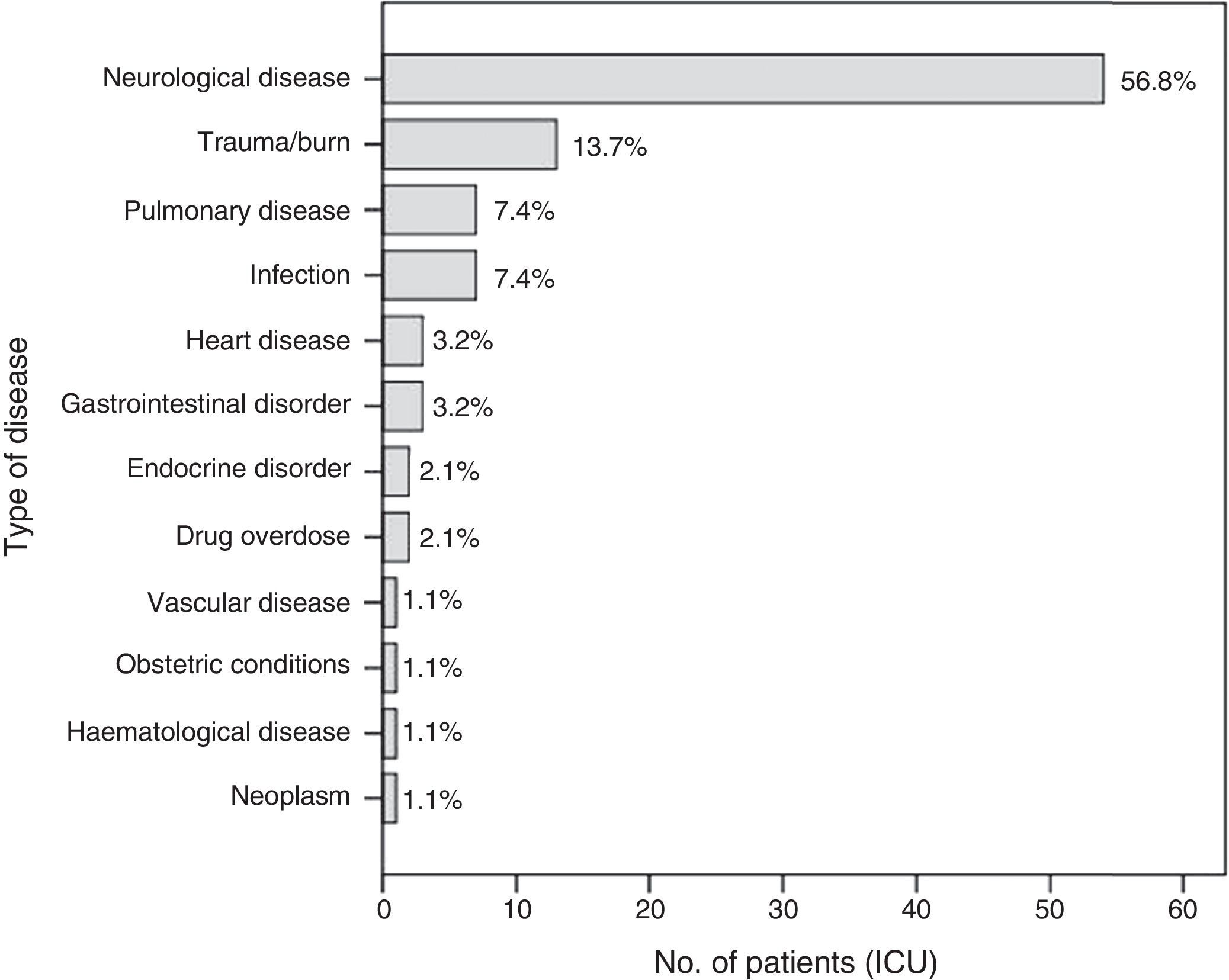
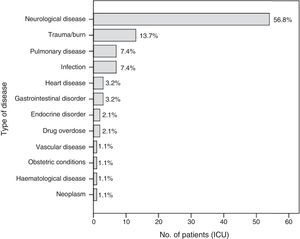
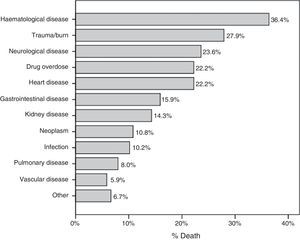
ResultsMean age of our patients was 62.1 years; 56.8% were men (n=268), and they were significantly younger than women at 60.6 vs 64 years (P=.038). The mean number of patients examined per month was 39.3 (range, 24–56). Of the sample, 19.7% (n=93) had been referred by another centre; in 89.5% of the cases (n=77), the reason was the need for specialised care. In 26.4% (n=125) of the cases, admissions had been scheduled. The conditions responsible for the hospitalisation of these patients were neurological/neurosurgical (excluding head trauma) in 22.5% (n=106), cardiac in 13.3% (n=63), infectious in 12.5% (n=59), digestive in 9.3% (n=44), head trauma in 9.1% (n=43), and other aetiologies in 33.3%. Of the patient total, 45.3% (n=214) needed to be transferred to a specialised unit at some point during hospitalisation. Fig. 1 shows the reason for hospitalisation of patients treated by the intensive care unit (ICU) and assessed by a consulting doctor. The median hospital stay was 18 days (range, 1–298).
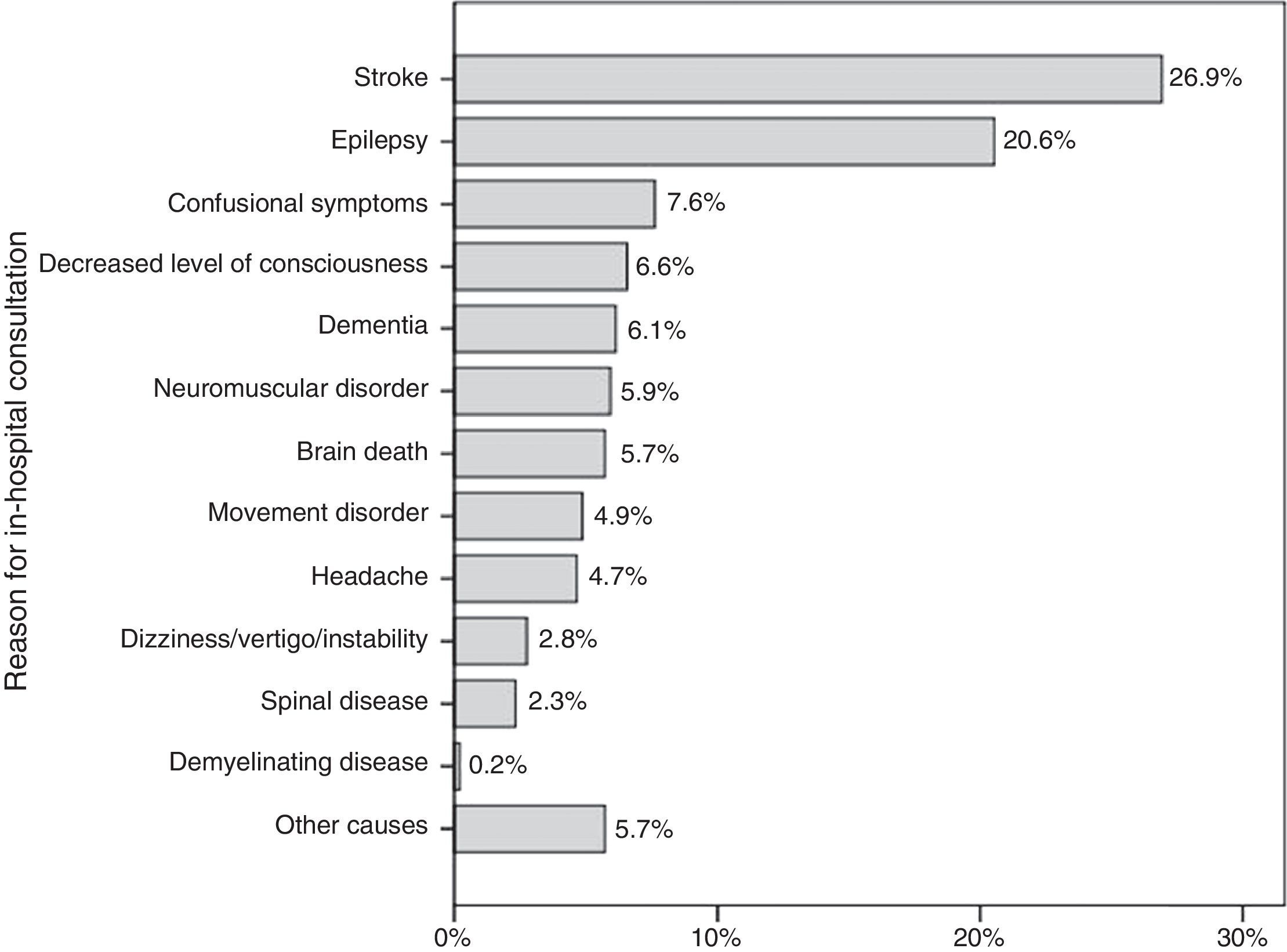
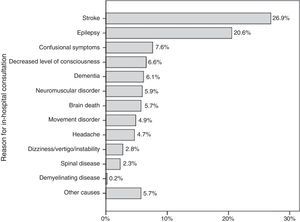
Departments presenting the most requests were intensive care (or ICU), with 20.1% of the in-hospital consultations (n=95), internal medicine with 14.4% (n=68), cardiology with 9.1% (n=43), general surgery with 7.6% (n=36), oncology with 6.4% (n=30), cardiac surgery with 5.5% (n=26), and others with 37.5%. Fig. 2 shows the reasons why different medical teams requested in-hospital consultations, with suspected stroke (26.9%), epileptic seizures (20.6%), confusional symptoms (7.6%), and decreased level of consciousness (6.6%) being the most frequent. The in-hospital consultations were requested for diagnostic purposes in 56.3% of the cases, therapeutic purposes in 28.2%, to limit treatment in 6.8%, and to provide a prognosis as a guide for further procedures in 8.7%. Of the patients, 24.4% (n=115) had previously been assessed by a neurologist for the same reason that motivated the consultation.
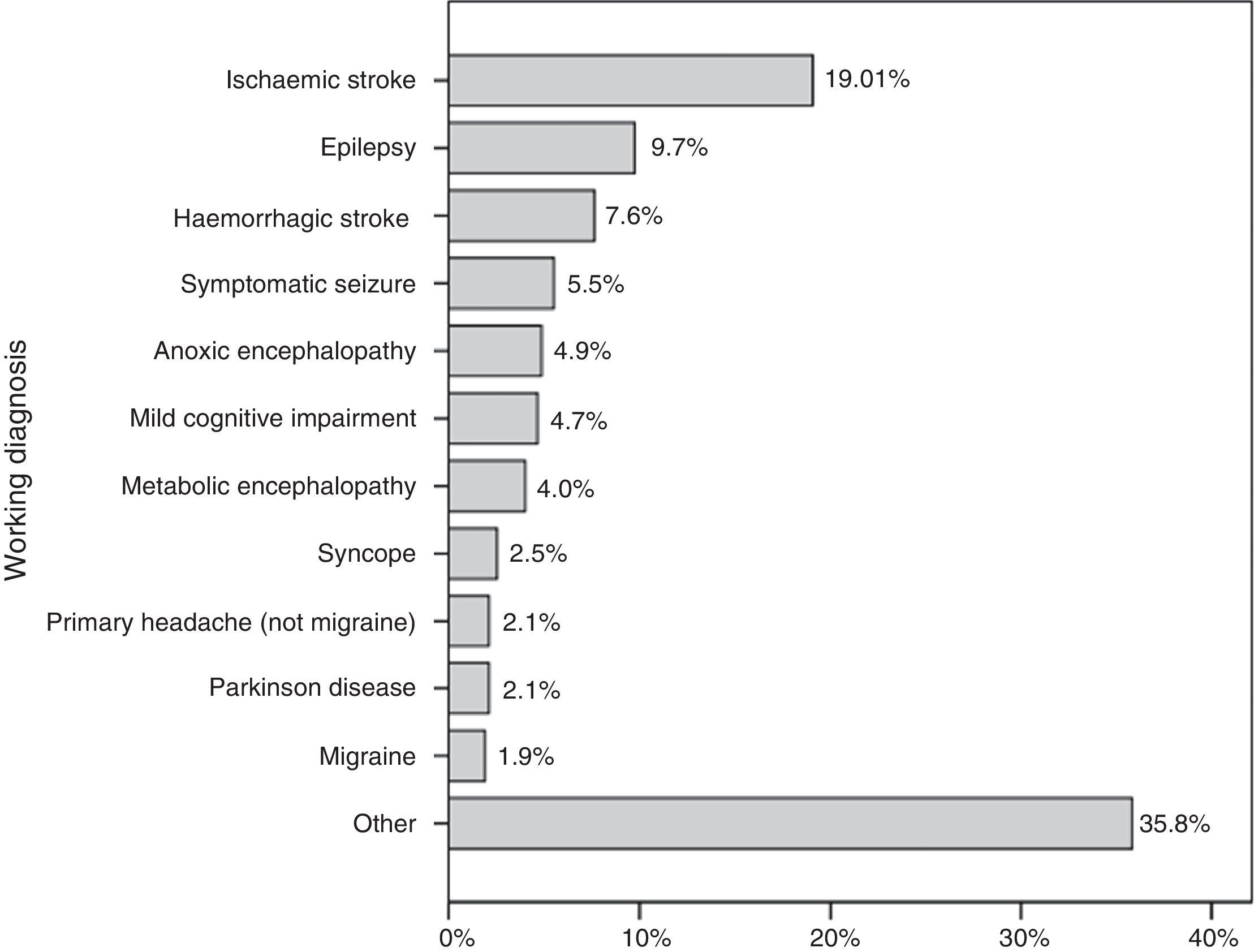
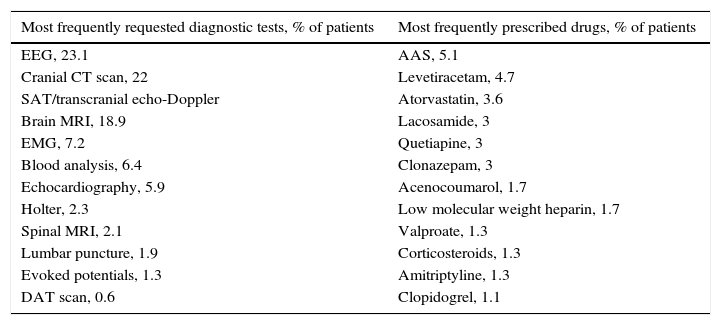
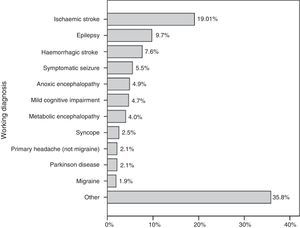
Fig. 3 shows the working diagnoses provided by the consultant; the most frequent were ischaemic stroke (19.1%), epilepsy (9.7%, including status epilepticus), haemorrhagic stroke (7.6%), and symptomatic seizures (5.5%). A specific aetiological diagnosis could be established in 46.6% of the cases (n=220), while the remaining received a syndromic diagnosis. No diagnostic tests were necessary in 30.5% (n=144) of the cases, one test was used in 39%, 2 tests in 20.6%, and more than 2 tests in 9.9%. Table 1 lists the most frequently requested diagnostic tests.
Most frequently requested tests and most frequently prescribed drugs.
| Most frequently requested diagnostic tests, % of patients | Most frequently prescribed drugs, % of patients |
|---|---|
| EEG, 23.1 | AAS, 5.1 |
| Cranial CT scan, 22 | Levetiracetam, 4.7 |
| SAT/transcranial echo-Doppler | Atorvastatin, 3.6 |
| Brain MRI, 18.9 | Lacosamide, 3 |
| EMG, 7.2 | Quetiapine, 3 |
| Blood analysis, 6.4 | Clonazepam, 3 |
| Echocardiography, 5.9 | Acenocoumarol, 1.7 |
| Holter, 2.3 | Low molecular weight heparin, 1.7 |
| Spinal MRI, 2.1 | Valproate, 1.3 |
| Lumbar puncture, 1.9 | Corticosteroids, 1.3 |
| Evoked potentials, 1.3 | Amitriptyline, 1.3 |
| DAT scan, 0.6 | Clopidogrel, 1.1 |
Previous treatment was adjusted in 18.9% (n=80) and one or more drugs were withdrawn in 10% (n=47). Reasons for discontinuing medication were lack of efficacy in 50% of the cases; adverse effects accounted for the other 50%. The neurologist prescribed medication in 27.3% (n=29); in 64.9% of these cases (n=81), only one drug was prescribed. Table 1 lists the most frequently prescribed drugs. Furthermore, we observed that establishing a specific diagnosis was significantly associated with starting drug treatment (P=.008).
Of the patient total, 4.9% (n=23) were transferred to the neurology department; the reasons for transferral were ischaemic stroke in 43.5% (n=10), epilepsy in 8.7% (n=2), study of parkinsonism in 8.7%, and other pathologies in 39.1%. In 62.1% (n=293) of the cases, patients were assessed on a single occasion, with no need for follow-up. The 75th and 95th percentiles (P) for days of follow-up were 3 and 12 days, respectively. Eleven per cent (n=52) were assessed on an additional occasion, and the working diagnosis changed in 5.8% of the cases (n=3).
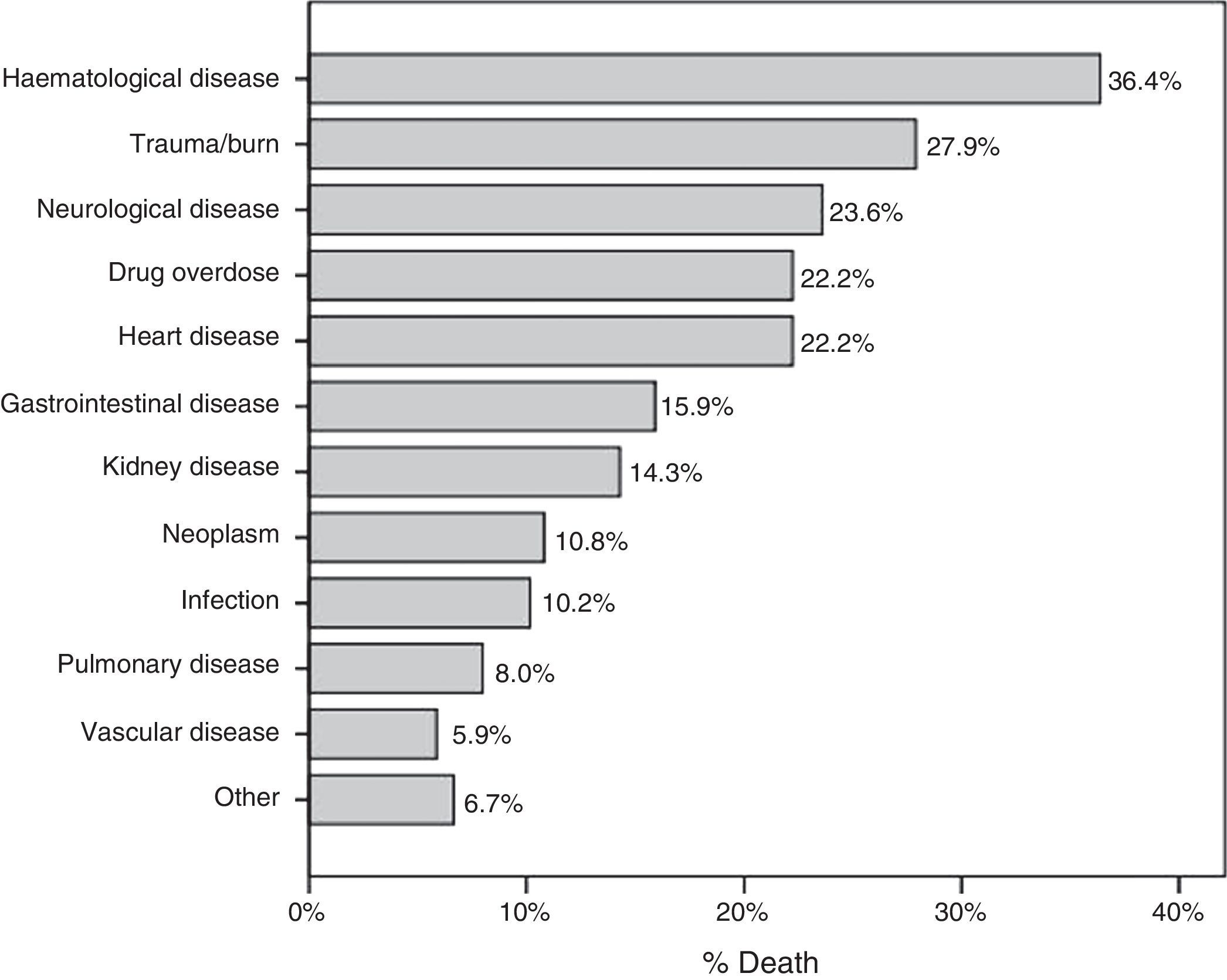
Eighty patients (16.9%) died during admission, and in 37.5% of these cases (n=30), the reason for consultation was to diagnose brain death. Fig. 4 shows the percentage of deaths broken down by the disease giving rise to hospitalisation. After discharge, 45.6% (n=215) were referred to the outpatient neurology service (in our hospital or to a neurologist in the patient's area). One hundred nine patients (23.1%) could not be discharged and were transferred to another hospital instead. In the 6 months after discharge, 6.1% of the patients came to the emergency department with a neurological problem. No significant differences were found between those transferred to another hospital and those who were not (3.7% vs 6.9%, P=.220).
It is worth mentioning that 41.9% of the patients (n=198) were assessed at some point by the on-call neurologist. In our series, assessment by the on-call neurologist (P<.001) and a higher number of tests performed by the consulting doctor (P=.005) were associated with a specific neurological diagnosis.
DiscussionThe in-hospital consultation system is complex and involves multiple variables, both human and organisational. English-speaking countries were the first to study this phenomenon; as early as in 1983, Goldman et al.3 published the 10 commandments for effective consultations. Later, Marshall4 and Cohn5 also explored the topic. Due to increasing knowledge and the emergence of new techniques in the different medical specialties over the past 20 years, in-hospital consultations have been adopted as the method of choice to offer the best in-hospital healthcare, with the legal consequences they entail. Cost effectiveness is another goal for in-hospital consultations, given the limited financial resources of healthcare systems.
Respect for the work of other professionals and effective communication are the keys to this process. It begins with the requesting doctor, who assesses the degree of necessity and urgency associated with the in-hospital consultation, which will finally affect the patient's state of health. Consultants must be aware of what is expected of them, their available means and necessary limitations, and their work should focus on the patient's well-being. If outcomes are to be improved, the intervention should be clear, adapted to the situation, and include appropriate follow-up, where necessary.5
The first studies on in-hospital consultations were conducted in surgical departments; however, there is increasing demand for in-hospital consultations with neurology departments due to the complexity of this specialty and the high prevalence of neurological diseases. This being the case, the United Kingdom and Ireland, which are countries with low numbers of neurologists per population, have been the first to perform studies.6,7 In Spain, 4 studies are deserving of mention: one conducted in Granada (Barrero-Hernández et al.),8 2 in Madrid (Cruz-Velarde et al. and García-Ramos et al.)9,10 and one conducted in Badajoz (Ramírez-Moreno et al.)11 This last study is especially relevant since it included a follow-up period of 5 years, and so is the study by García-Ramos et al.10 thanks to the data it provides and the accompanying literature review.
Returning to our own study, which is relevant for being the first of its type in Catalonia, it is clear that our data are strongly influenced by the organisational distribution within our centre. For example, our hospital has an on-call neurologist who is especially important for proper functioning of the hospital, as well as readily accessible (41.9% of the patients assessed in our study have been seen by this neurologist). Additionally, we have a team of neurologists specialising in neurocritical care. This explains the high volume of requests for in-hospital consultations to be performed by this department, unlike in other studies with similar characteristics. Other relevant results were diagnosis of brain death (in 37.5% of the cases resulting in death, the neurologist had to perform that function), the lack of complementary tests in 30.5% of all patients, and the low percentage of patients visiting the emergency department due to neurological causes after discharge (whether to home or another location). Also significant was the fact that the initial working diagnosis was changed in only 3 cases.
Regarding the importance of the neurologist in a general ICU, a recently conducted study12 states that most neurological problems can be managed by a general neurologist.
The limitations of our study include its retrospective design and its study period of only one year; also, the opinions of other doctors and patients have not been considered. In this sense, if we are to avoid such situations as those observed by Roberts et al.13 in their study, in which 22.7% of those patients surveyed (n=37) did not know they had been seen by a neurologist, hospital neurologists must focus on their educational role.
We conclude that neurological in-hospital consultations facilitate management of neurological patients, potentially improving their outcomes (in 46.6% of the cases, a specific diagnosis was assigned and the appropriate treatment measures were implemented) and decreasing the probability of an emergency department visit. Furthermore, in tertiary hospitals, neurologists are essential for on-call work and diagnosing brain death.
Conflicts of interestThe lead author of this article, on behalf of himself and of all authors, states that there are no potential conflicts of interest related to this study.
Please cite this article as: Aller-Alvarez JS, Quintana M, Santamarina E, Álvarez-Sabín J. Análisis descriptivo de las consultas intrahospitalarias dirigidas a Neurología en un hospital terciario. Neurología. 2017;32:152–157.
This database was presented orally at the 66th Annual Meeting of the Spanish Society of Neurology (Valencia, November 2014).