Balo concentric sclerosis (BCS) is a rare type of inflammatory/demyelinating disease first described by Joszef Balo in the early 19th century.1 Balo reported several cases of neurological deficits with a fulminant progression in which autopsy studies revealed demyelinating lesions arranged in concentric rings. At present, this entity is easier to diagnose and treat in its early stages thanks to MRI.2 However, the pathophysiology of BCS is still to be determined and there is no consensus on the most suitable treatment in acute stages or in the long term.
We present the case of a young patient with BCS who was first suspected of having ischaemic stroke; MRI was the key to diagnosing BCS.
Our patient was a 42-year-old woman who arrived at our hospital's emergency department after code stroke activation due to a 2-hour history of weakness and hypoaesthesia in the right hand. She had a history of hypertriglyceridaemia and was an active smoker (consuming one pack of cigarettes daily). At the age of 32, she started hormone replacement therapy with a vaginal ring due to early menopause. She had no family history of interest. Upon arriving at the emergency department, her vital signs, including blood pressure, heart rate, temperature, oxygen saturation, and glucose levels, were normal. The initial neurological examination revealed paresis of the right upper limb with preserved reflexes; our patient scored 2 on the NIHSS. An emergency CT scan displayed a hypodense lesion in the left corona radiata. A neurosonology study (transcranial and supra-aortic trunks) revealed no stenosis or large-vessel occlusion. The ECG showed sinus rhythm and results from a blood test were normal. The patient was initially diagnosed with probable ischaemic stroke; reperfusion treatment was ruled out in view of the scarce focal neurological signs and the signs of established lesion. As a result, she started treatment with antiplatelet drugs and statins and was admitted to the stroke unit of our hospital.
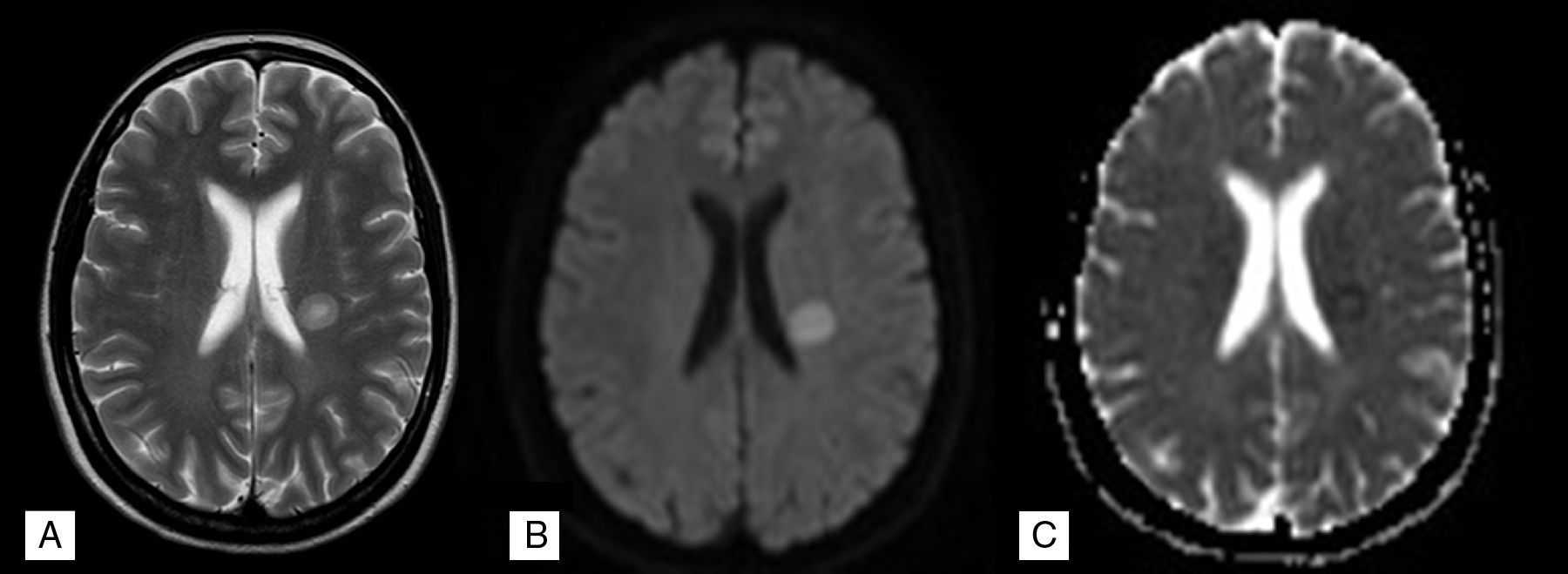
The initial aetiological study included transoesophageal echocardiography, which revealed patent foramen ovale. A complete blood count, including an immunological test, a test for tumour markers, serology tests, and a coagulation study, revealed no relevant findings. However, our patient's condition worsened progressively, reaching a 0/5 muscle strength rating in the right upper limb and ipsilateral central facial palsy. A brain MRI scan performed 4 days after admission revealed signal alterations arranged in layers in T2-weighted and diffusion sequences (Fig. 1A and B): the edge of the lesion showed apparent diffusion coefficient (ADC) restriction (Fig. 1C) whereas the centre displayed increased ADC (Fig. 1C), which is typical of BCS. The suspicion of a demyelinating/inflammatory disease required a lumbar puncture; the only relevant finding was presence of IgG oligoclonal bands. We started treatment with a bolus of 1g methylprednisolone daily. The patient was responding favourably to treatment by the third day and was discharged after 5 days of treatment due to symptom resolution.
Twelve months later, she remained asymptomatic. Two follow-up MRI scans at 6 and 12 months revealed a decrease in the size of the lesion, which no longer had a layered appearance. The absence of new lesions rules out dissemination. We decided not to administer immunomodulatory drugs but rather to conduct follow-up clinical and radiological studies.
BCS is a rare form of demyelinating disease whose clinical presentation and lesion distribution may vary.
In our case, ischaemic stroke was the main differential diagnosis given the sudden onset of symptoms and our patient's medical history. Co-presence of vascular risk factors, use of hormonal contraceptives, and patent foramen ovale suggested paradoxical embolism. MRI was decisive for diagnosis as it revealed a lesion with a characteristic layered appearance. Lesions consisting of concentric rings of demyelination are regarded as a pathognomonic sign of BCS by some authors.3
This form of presentation of BCS has only rarely been described in the literature.4 In a recent review article of stroke mimics treated with rTPA, only 5% of the cases were finally diagnosed with inflammatory or demyelinating diseases, well behind such other conditions as epilepsy and psychogenic disorders.5 The most characteristic feature of BCS is the presence of hypodense lesions in emergency cranial CT images, which may be located in a single vascular territory and resembling ischaemia, unlike other stroke mimics. In light of the above, and given the low incidence of BCS, MRI evaluation by an expert neuroradiologist is essential.6
In conclusion, our case demonstrates that BCS may present and progress with features similar to those of ischaemic stroke. BCS is a rare disease characterised by extensive, non-specific lesions on CT, which differentiate it from other stroke mimics in the acute phase. However, interpreting MRI findings is not easy, which may lead to misdiagnosis followed by administration of unnecessary secondary prevention treatments. In differential diagnosis, we should also consider other less frequent causes of neurological deficits; in MR images, all that glitters is not stroke.
Please cite this article as: Aracil-Bolaños I, Prats-Sánchez L, Gómez-Ansón B, Querol-Gutiérrez L, Núñez-Marín F, Martí-Fàbregas J. Esclerosis concéntrica de Balo: una presentación que simula un ictus isquémico. Neurología. 2017;32:60–61.