The differential diagnosis of bilateral lower limb weakness includes a wide range of disorders; in these cases, central and peripheral causes of weakness (vascular, neoplastic, traumatic, or neuromuscular causes) must be sequentially ruled out. Unilateral quadriceps tendon rupture is rare, with a prevalence of 1.37 cases per 100 000 population; it is more common in men and in the fifth decade of life, and is associated with thyroid or kidney disorders.1–6 Bilateral quadriceps tendon rupture is even rarer, with only isolated cases reported in the literature.2–7
We present the case of a 50-year-old man with personal history of arterial hypertension and obesity who was receiving doxazosin, bisoprolol, enalapril, and hydrochlorothiazide. He visited the emergency department due to thoracolumbar trauma following an accidental fall at his home from a height of approximately 2 metres. After the fall, he reported weakness in both lower limbs, which prevented him from walking. He did not report pain, sphincter dysfunction, or loss of sensitivity. He was assessed by the traumatology department; the initial examination revealed no signs of fracture or joint lesions, and radiography of the joints and lumbar region revealed no alterations.
A lumbar spine MRI scan also detected no significant alterations. Three weeks later, the patient visited the neurology department due to persistent inability to walk and a burning sensation in the suprapatellar region bilaterally, with kneecap swelling and quadriceps atrophy.
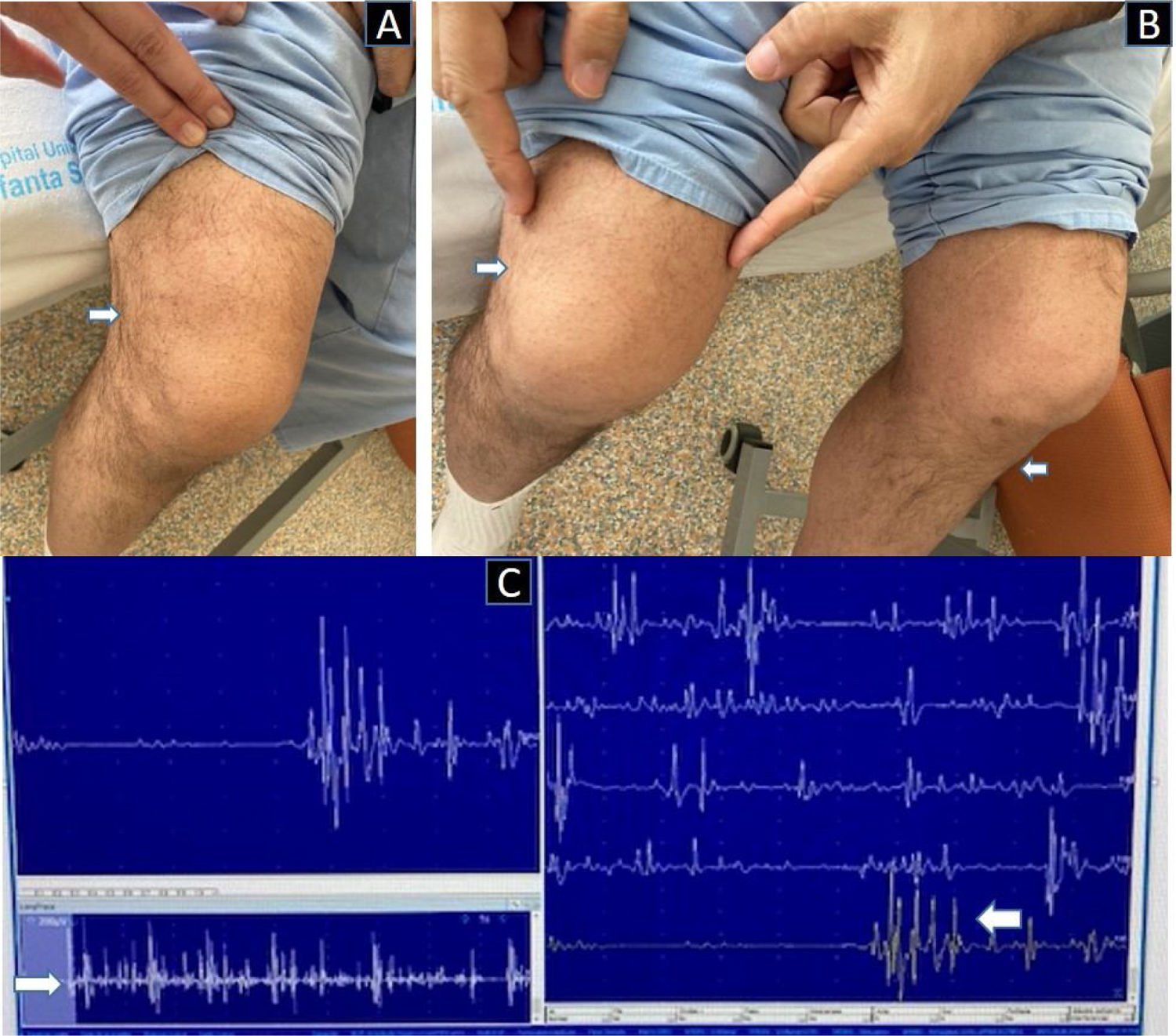
The clinical examination revealed 4+/5 strength in hip flexion and knee extension, and 5/5 strength in distal lower limb muscles, with no claudication in antigravity movements, bilateral flexor plantar reflex, and abolished patellar and Achilles reflexes bilaterally. Tactile and vibratory sensitivity were preserved. Gait could not be assessed due to the patient’s inability to stand. No alterations were observed in the upper limbs, cranial nerves, or higher cortical functions (Fig. 1).
A) Bilateral suprapatellar depression, more marked in the right knee. B) Amyotrophy of the tibialis anterior and quadriceps muscles, with inability to extend both knees. C) Needle electromyography of the right vastus lateralis muscle, showing reduced motor unit potentials interspersed with polyphasic motor unit potentials, and a pattern of reduced maximal effort.
An electromyoneurography study did not detect neuropathy in the peroneal, tibial, or sural nerves, or any sign of underlying plexopathy. However, it did detect bilateral chronic denervation with polyphasic potentials in proximal leg muscles (adductor longus and vastus lateralis muscles bilaterally), and possible disuse muscle atrophy, with no signs of chronic or active denervation, at the distal level (L4-S1) bilaterally (Fig. 1).
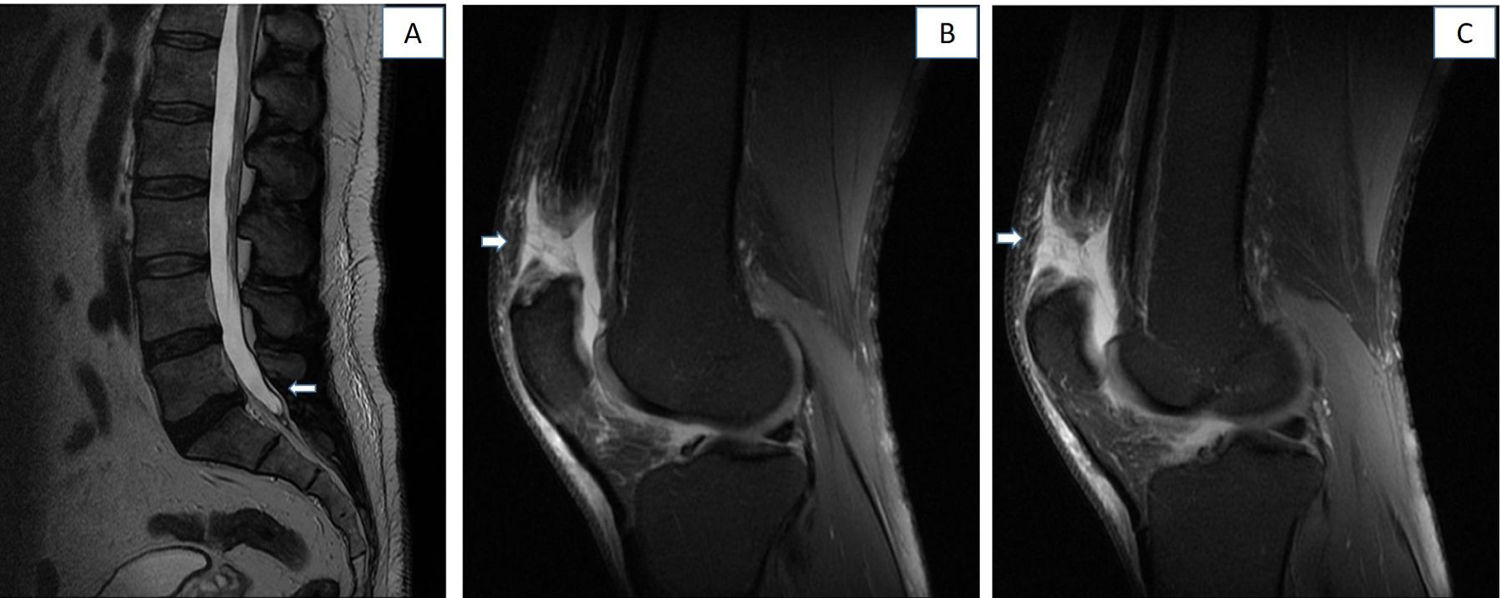
A contrast-enhanced thoracolumbar MRI scan revealed left subarticular T6-T7 disc protrusion, causing mild spinal cord compression, with no signs of myelopathy, as well as smaller protrusions at L4-L5 and L5-S1 (Fig. 2).
Lumbar spine and knee MRI (T2-weighted sequence, sagittal plane). A) Lumbar spine MRI revealing a small protrusion at L5-S1, and a smaller one at L4-L5. B) Right knee MRI revealing rupture of 90% of the fibres of the quadriceps tendon. C) Left knee MRI revealing full-thickness rupture of the quadriceps tendon.
We performed another physical examination, noticing a gap in the quadriceps bilaterally (suprapatellar depression or “hack sign”), which was more pronounced in the right knee, and bilateral joint effusion (Fig. 1). An MRI scan of both knees revealed a full-thickness tear in both quadriceps tendons (> 90% of fibres in the right tendon and complete rupture in the left), with signs of calcific enthesopathy in the preserved fibres, and haematoma in the area of the rupture (Fig. 2).
In view of these findings, the patient was referred to the traumatology department and underwent surgery for tendon repair, progressing favourably after the intervention.
Bilateral quadriceps tendon rupture is rare even after accidental falls, and requires early diagnosis and surgical management. Its prevalence increases with age, and it may be associated with history of hyperuricaemia, thyroid or kidney disorders, diabetes, and corticotherapy.
Our patient had no history of any of these conditions. We first screened for any causes of acute compression (spinal cord compression, vertebral fractures, dural fistulas, psoas haematoma, and post-traumatic plexopathy), detecting no abnormalities. We also considered Guillain-Barré syndrome or acute nutritional polyneuropathy, but electromyography and laboratory tests yielded no results supporting those diagnostic hypotheses. Repeated physical examinations by different specialists detected a rare sign, which guided diagnosis.
The diagnostic triad of quadriceps tendon rupture is acute pain, inability to extend the knee, and a palpable suprapatellar gap.8–10 An MRI scan of both knees confirmed the diagnosis. Treatment for quadriceps tendon rupture is conservative in case of partial rupture, whereas full-thickness rupture requires surgical management, as in the case presented.11
These clinical signs should be considered in the neurological examination of patients with acute paraparesis.
Conflicts of interestThe authors have no conflicts of interest to declare and have approved the content of the manuscript.
Please cite this article as: González Martín L, Abenza Abildua MJ, Almarcha Menargues ML, Martínez Brandulas P. La rotura del tendón cuadricipital bilateral como causa inhabitual de paraparesia aguda. Neurología. 2022;37:606–608.