We read with great interest the article by López Perales et al.,1 who present a masterful description of a clinical case to address a long-standing debate in cardiology: should anticoagulation be administered to patients with advanced interatrial block (IAB) but no clinical evidence of atrial fibrillation (AF)?
IAB is a disorder of conduction between both atria caused by replacement fibrosis in the Bachmann bundle.2 It has traditionally been classified as partial, advanced, or intermittent,3 although a new category, atypical advanced IAB, has recently been included.4 Several studies have shown an association between advanced IAB and subsequent development of AF, which is known as Bayés syndrome.2 However, recent evidence suggests that the presence of IAB (and particularly advanced IAB) may increase the risk of cardioembolic events, mainly stroke.5 Carrillo-Loza et al.6 showed that presence of IAB predicts stroke recurrence in patients with history of embolic stroke of undetermined source, revealing the following independent risk factors for stroke: advanced AIB (P<.001), male sex (P=.028), and age over 50 years (P=.039).6
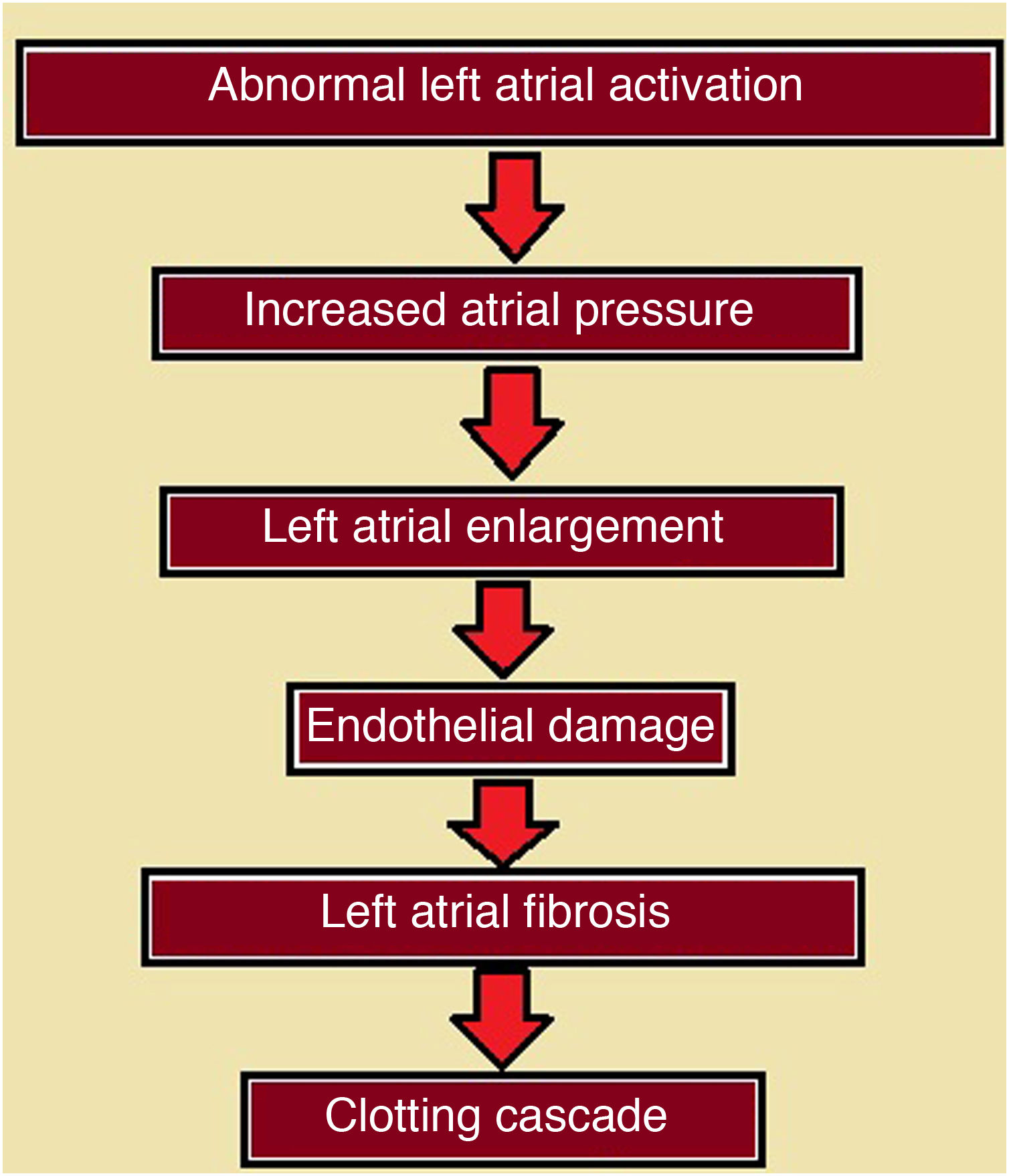
Several mechanisms have been reported to play a role in the pathophysiology of thromboembolic events secondary to IAB, including atrial dyssynchrony, endothelial damage, and atrial fibrosis, all of which appear sequentially and promote activation of the clotting cascade (Fig. 1).7 Atrial fibrosis, an important marker of atrial dysfunction, may be studied with such techniques as two-dimensional speckle tracking echocardiography, a non-Doppler technique enabling quantification of atrial deformation based on standard two-dimensional images and the measurement of longitudinal strain (ε, expressed as a percentage) and longitudinal strain rate (SR, expressed as the number of deformations per second) of the left atrium during a cardiac cycle.8 This happens to have been the technique used by López Perales et al.1 in their excellent report.
Schematic representation of the sequential process by which presence of interatrial block may trigger a series of phenomena leading to the activation of the clotting cascade and consequently the development of thromboembolic events. Modified from Martínez Sellés et al.7
The BAYES registry, a recent multicentre study conducted between 2017 and 2020, found IAB to be a powerful predictor of AF and stroke in non-hospitalised older patients with underlying structural heart disease. The study included data from 556 patients, who were classified into 3 groups (group A, P wave<120ms; group B, partial IAB; group C, advanced IAB). Patients were followed up for a mean of 694 days: 16.7% developed AF, 5.4% presented stroke, and 6.1% died during follow-up. The incidence of AF in groups A, B, and C was 24%, 29%, and 40%, respectively, and the incidence of stroke was 9%, 9%, and 12%. After performing univariate and multivariate analyses, the authors concluded that advanced IAB was an independent predictor of AF and stroke, and that P-wave duration showed a linear correlation with increases in the incidence of AF, stroke, and mortality (Fig. 2).9
Kaplan-Meier curves from the BAYES registry representing the percentage of patients who develop atrial fibrillation (A), stroke (B), and atrial fibrillation or stroke (C), as a function of time. Group A: solid blue line. Group B: dashed red line. Group C: dashed green line. AF: atrial fibrillation; IAB: interatrial block. Reproduced with authorisation from Martínez-Sellés et al.9
Despite the available evidence, the answer to the question posed by López Perales et al.1 of whether oral coagulation should be administered in patients with no evidence of AF is “no,” or at least “not for the time being.” Two studies on the topic are currently underway: Atrial Cardiopathy and Antithrombotic Drugs in Prevention after Cryptogenic Stroke (ARCADIA)10 and Anticoagulation Management in Interatrial Block with Long-term Evaluation (AMIABLE). Both seek to evaluate the efficacy of anticoagulation in preventing stroke recurrence (in the former) and first stroke (in the latter) in patients with atrial dysfunction, including IAB.5
In this context, ambulatory external electrocardiography monitoring is becoming increasingly important in the study of patients in whom AF is strongly suspected.11 Such long-term monitoring techniques as Holter monitoring over periods of weeks and ambulatory cardiovascular telemetry are examples of the wide range of non-invasive monitoring methods showing great effectiveness in different clinical scenarios.11 When correctly used, these tools may be extremely useful in the study of patients with IAB, enabling early detection of AF and, consequently, early implementation of oral anticoagulation with a view to preventing cardioembolic events.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Iomini PA, Baranchuk A. Bloqueo interauricular avanzado y accidente cerebrovascular: esperando la evidencia para decidir anticoagulación. Neurología. 2022;37:604–606.