Several cases have been reported of neurogenic muscle hypertrophy associated with chronic radiculopathy,1–4 most of them involving the gastrocnemius and/or soleus muscles in the context of ipsilateral S1 radiculopathy.1,3,5 The aetiopathogenesis of this entity is unknown.3,4 A minority of patients with neurogenic muscle hypertrophy present anatomical pathology findings of inflammation of unknown origin.1,2,4–11 Such cases are described as instances of neurogenic focal myositis,1,4,5 an infrequent entity presenting with increased volume in the region of the inflamed muscle and frequently with muscle pain.1 Diagnosis is based on clinical data and complementary test results: moderately elevated serum CPK levels, electromyographic findings of acute denervation in the muscle groups innervated by one peripheral nerve or one nerve root in addition to a pattern of chronic denervation, MRI findings suggestive of inflammation, and anatomical pathology findings indicating inflammatory changes.1 Corticosteroid treatment, normally at low doses and for short periods of time, has been trialled in patients with focal myositis secondary to nerve lesions.5 Although response to this treatment varies,11 it may induce clinical remission and improve neuroimaging findings.10
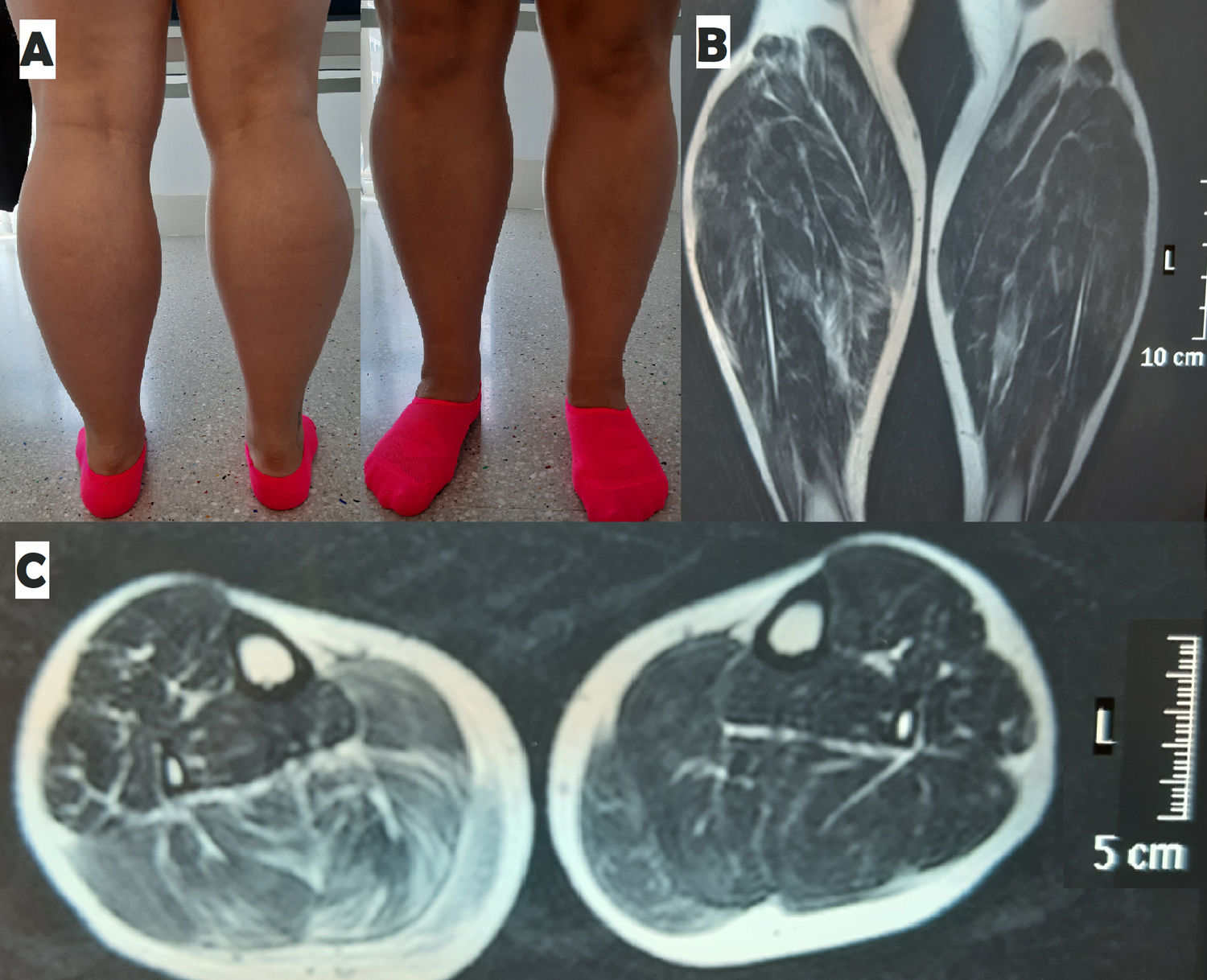
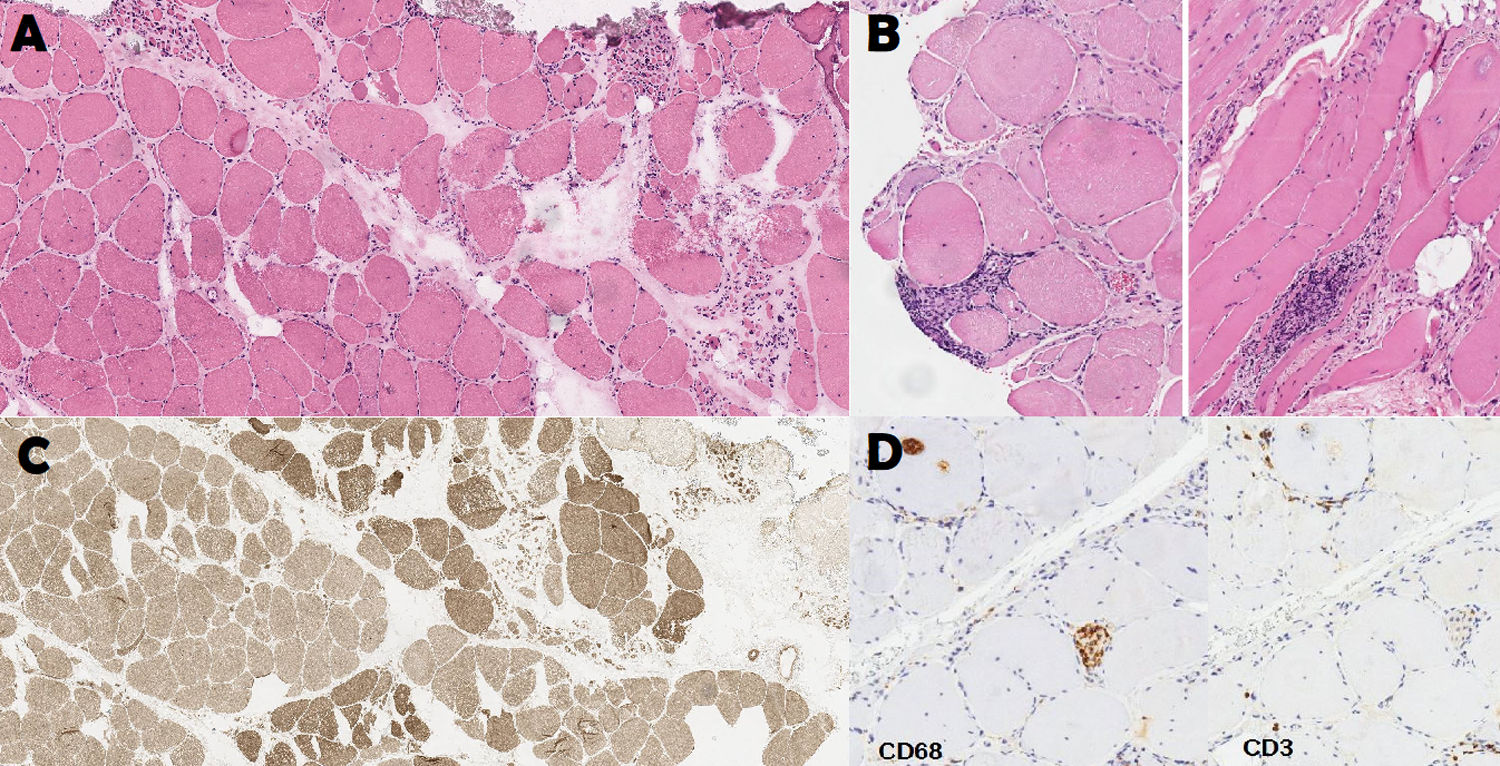
Clinical caseWe present the case of a 35-year-old woman who in 2016 underwent emergency surgery due to cauda equina syndrome secondary to L4-L5 spinal disc herniation associated with compression of the L4, L5, and S1 roots bilaterally. After an initial period with bilateral gastrocnemius muscle atrophy, our patient progressively recovered muscle mass in both legs, although residual muscle atrophy was more marked in the right leg. Approximately one year later, she consulted due to a progressive increase in the volume of both calves, associated with bilateral calf muscle pain. The examination revealed bilateral gastrocnemius muscle hypertrophy, predominantly affecting the right leg (Fig. 1), with marked tension upon palpation of the calves, weakness in right toe flexion, painful contracture of the right gastrocnemius muscles upon plantar flexion of the right foot, and inability to toe walk. Muscle strength was otherwise normal (5/5 on the Medical Research Council scale). The Achilles reflexes was absent bilaterally, with the remaining deep tendon reflexes being normal (3/5 symmetrical). A blood analysis revealed a CPK level of 514 U/L, with normal CRP and ESR values. The patient tested negative for autoimmune myositis. An electromyoneurography study revealed fibrillations and fasciculations in the gastrocnemius and tibialis anterior muscles bilaterally, although predominantly in the right leg. Muscle MRI of both legs revealed hypertrophy of the bilateral triceps surae, as compared to the remaining muscles. Hypertrophy was more marked in the right leg, showing increased signal intensity on T2-weighted sequences, suggesting diffuse muscle oedema (Fig. 1). A biopsy study of the right gastrocnemius muscles revealed small endomysial inflammatory foci, mainly composed of CD3+ lymphocytes and macrophages, compatible with focal myositis (Fig. 2). After a month of treatment with oral prednisone dosed at 15 mg/day followed by 2 months with the same treatment on alternate days, the patient reported improvements in pain when walking, and decreases were observed in the volume of the left calf and in muscle tension upon palpation of both legs. CPK levels decreased to 256 U/L.
Anatomical pathology study of the right gastrocnemius muscle. (A) Denervation atrophy pattern. Group atrophy. Haematoxylin-eosin stain, 9×. (B) Foci of endomysial inflammatory infiltrate. Haematoxylin-eosin stain, 10×. (C) Fibre type grouping. ATPase pH 9.4 stain, 6×. Macrophages in the endomysium and within fibres. CD3+ lymphocytes in the endomysium and surrounding fibres. Immunohistochemical staining of CD68 and CD3, 10×.
We present the first published case of bilateral denervating focal myositis. The lack of systemic symptoms or involvement of any other muscle group, together with the history of cauda equina syndrome, led us to rule out an underlying systemic process and suggested 2 concomitant processes of neurogenic focal myositis. Although MRI did not reveal muscle oedema in the left triceps surae, and the biopsy study revealed pathological findings in the right gastrocnemius muscle, the patient presented bilateral symptoms and response to corticosteroid therapy was more marked on the left side. The fact that such an infrequent process presented bilaterally and was circumscribed to the triceps surae muscles in a patient with lesions to several nerve roots suggests that some individuals and certain muscles may have a predisposition for this condition. As in previously reported cases, our patient responded to corticosteroid therapy, which improved pain and muscle tension and decreased CPK levels.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González Toledo GR, Pérez Pérez H, Brage Martín L, Castro López-Tarruella V. Miositis focal de tríceps sural bilateral post-síndrome de cola de caballo. Neurología. 2021;36:647–649.