Subcortical band heterotopia, also known as double cortex syndrome (DCS), is an infrequent disorder of cortical migration, characterised by a well delimited layer of grey matter within the white matter, between the cerebral cortex and the lateral ventricles. The introduction of magnetic resonance imaging (MRI) in clinical practice made it possible to identify and characterise this entity.1 Most of the reported cases are women; affected men generally present lissencephaly with more severe neurological involvement.2
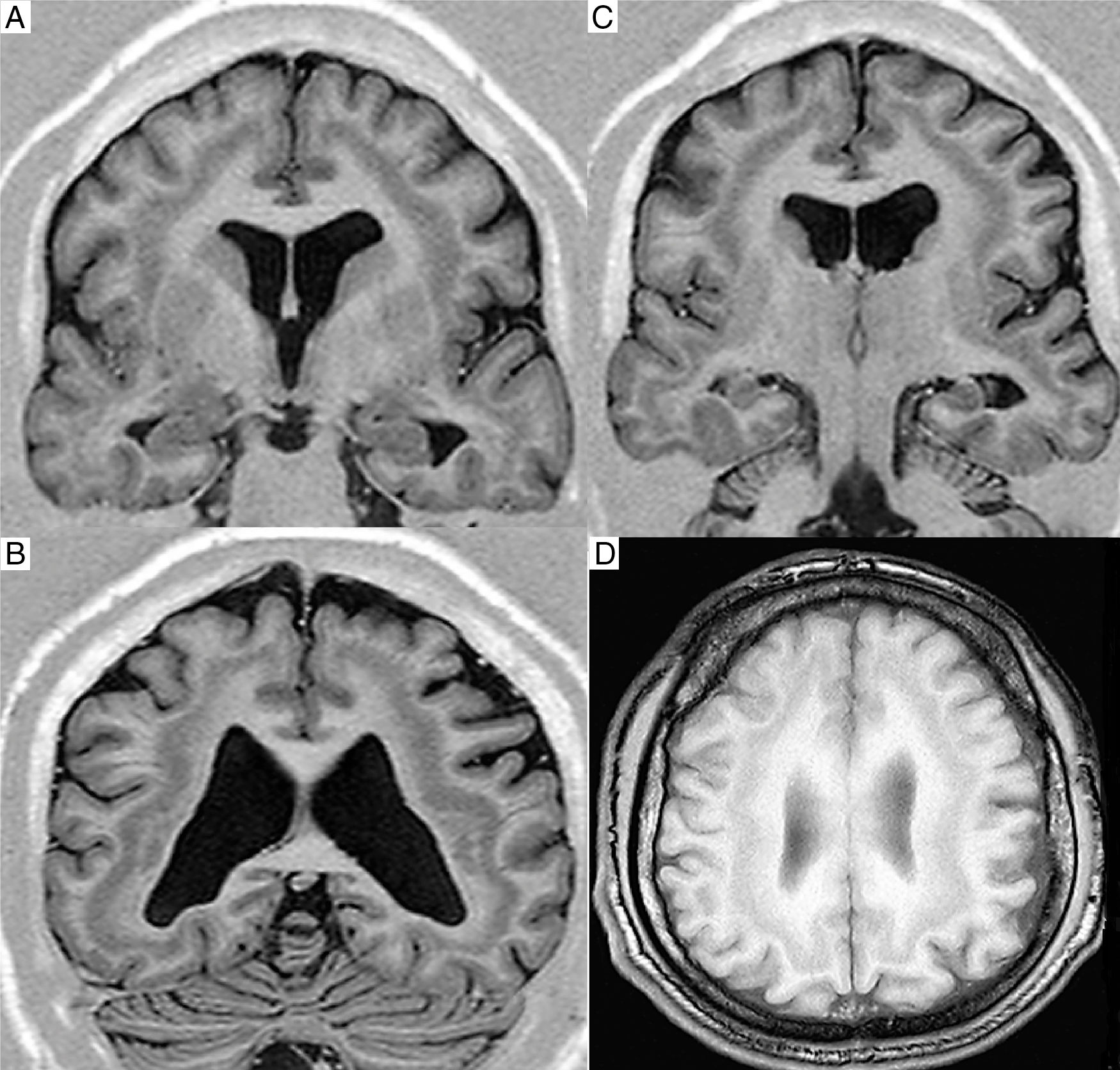
Our patient is a 26-year-old man referred to our centre due to suspected refractory epilepsy. The patient had no relevant prenatal history; he was born to non-consanguineous parents after a full-term pregnancy without complications and his neurodevelopment was normal during his first year of life. He had no family history of epilepsy or intellectual disability. During his first years of education, he presented poor school performance with learning difficulties; a psychological evaluation diagnosed mild-to-moderate intellectual disability. At the age of 6, he began to develop seizures and episodes of disconnection progressing to loss of consciousness with movements in the entire body. Over the past 20 years, seizure frequency increased, and the patient developed myoclonic, generalised tonic–clonic, and atonic seizures. A clinical examination revealed such dysmorphic features as hypertelorism and wide nasal bridge. He was treated with multiple antiepileptic drugs: phenytoin, carbamazepine, clonazepam, clobazam, valproic acid, and lamotrigine in monotherapy, bitherapy, and polytherapy, never achieving adequate control (Figs. 1 and 2). We started rational polytherapy with lamotrigine at 300mg/day, valproic acid at 2.5g/day, and levetiracetam at 3g/day, achieving acceptable control with only 2 partial seizures in the following 6 months.
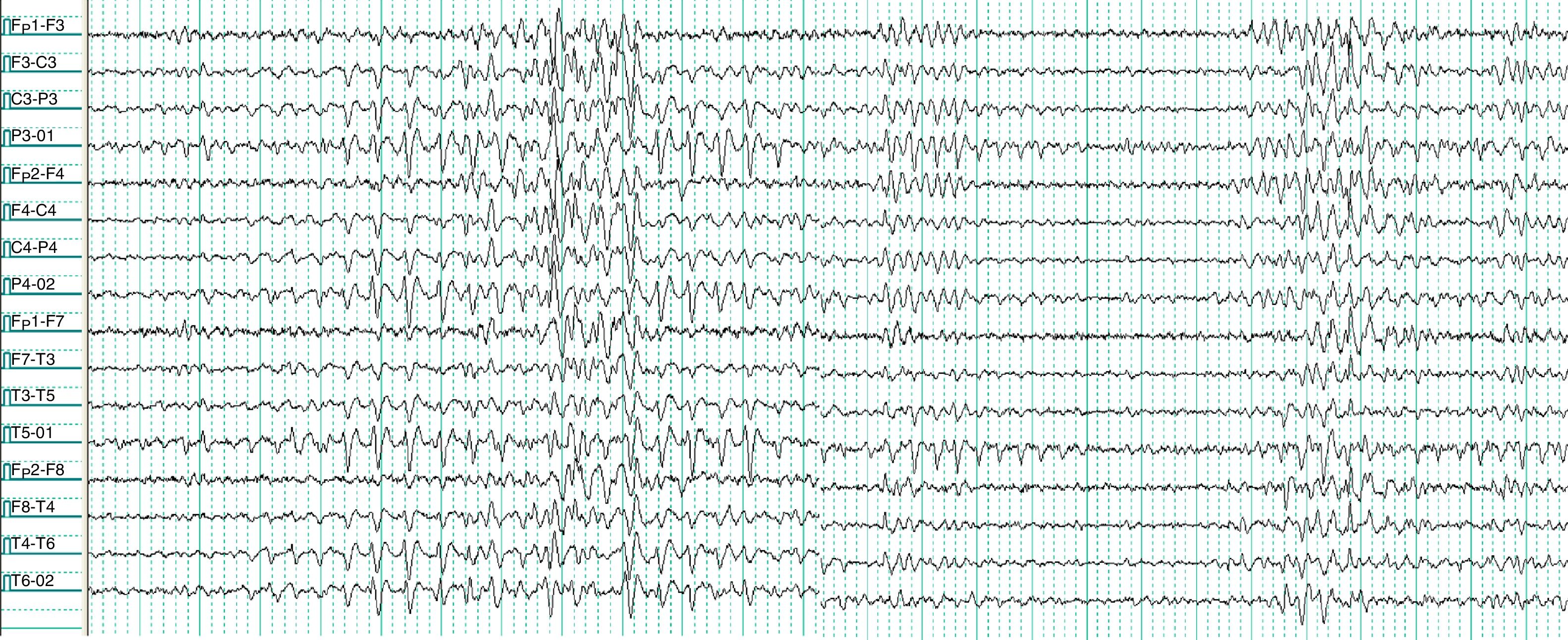
Waking electroencephalogram (10-20 international system, longitudinal bipolar montage). The recording shows several stages, with paroxysmal activity starting in the left occipital area, subsequently extending to frontal areas; the activity persists independently in occipital regions, especially in the left hemisphere, along the entire trace.
DCS is an infrequent disorder of cortical migration associated with mutations of chromosomes 17p13.3 (LIS1) and Xq22.3-q23 (DCX or XLIS). Mutations in the doublecortin gene (DCX) account for 85% of sporadic cases in women and 25% in men.1,3 This gene plays an important role in the coding of microtubule-associated proteins participating in neuronal migration during brain development; mutations in this gene cause severe damage to the structure of the cerebral cortex.4 The clinical characteristics justifying suspicion of DCS are the onset of epileptic seizures during the first decade of life, progressively becoming resistant to treatment, presence of multiple types of seizures, and intellectual disability.5 Subcortical band heterotopia is more frequent in women; male patients usually present lissencephaly or agyria/pachygyria complex predominantly involving frontal regions.2,6 These alterations were not observed in our patient. There are few reports of men with DCS with no lissencephaly or agyria/pachygyria. Mosaicism for DCX mutation is a possible explanation for the reduced severity of clinical manifestations in men.6 There is little evidence regarding the treatment of this condition when rational polytherapy fails. Although these patients present epilepsy with focal activity, surgery has shown discouraging results.7 It has recently been reported that bilateral stimulation of the anterior thalamic nuclei may help improve seizure control.8
Please cite this article as: Rivero Rodríguez D, Scherle Matamoros C, Dicapua Sacoto D, Maldonado Samaniego N. Síndrome de doble corteza en paciente masculino adulto sin lisencefalia. Neurología. 2020;35:144–145.