The stroke mortality rate in Andalusia is twice that of other autonomous communities. This could be associated with the absence of neurologists in most local hospitals in this community, unlike in the rest of Spain. The objective of this study was to evaluate the impact of incorporating a neurologist to evaluate and monitor stroke patients in a local hospital in Andalusia.
MethodsAn observational study was conducted on stroke cases admitted in the first quarter of 2006. Quality indicators, mortality rates, and incapacity rates at follow-up were analysed, comparing groups with and without neurological care.
ResultsA total of 116 stroke patients were admitted. There were significant differences in tests performed to diagnose patients (Doppler and echocardiography). The mean hospital stay was significantly lower with neurology care. There was a 39.1% absolute decrease in mortality and a 35.7% absolute increase in capacity for daily life activities was also observed. Neurological care and a lower incapacity level at admission were the only two factors independently associated with a decrease in length of hospital stay and mortality.
ConclusionSpecialised care by a neurologist is effective in reducing length of hospital stay, mortality and incapacity. The incorporation of neurologists in local hospitals in Andalusia should be a priority to guarantee equal care in all autonomous communities in Spain. This objective should be included in the Plan Andaluz de Atención al Ictus as a first step in forming a network of stroke units and teams.
En Andalucía la mortalidad por ictus duplica la de otras autonomías lo que podría relacionarse con que, a diferencia del resto de CC. AA., sólo 3 de 17 hospitales comarcales cuentan con neurología. El objetivo de este estudio fue evaluar la repercusión de la introducción de un neurólogo en un hospital comarcal de Andalucía en la evaluación y evolución de pacientes con ictus.
MétodosSe realizó un estudio observacional de los ictus ingresados en el primer trimestre de 2006. Se analizaron indicadores de calidad, mortalidad y dependencia comparando los pacientes atendidos por neurología o medicina general.
ResultadosEn el primer trimestre de 2006 ingresaron 116 pacientes con ictus. Se detectaron diferencias significativas en la realización de las pruebas complementarias necesarias para el diagnóstico (Doppler, ecocardio). La estancia media fue significativamente menor en neurología. Se detectó una reducción absoluta de 39,1% de mortalidad y un incremento absoluto del 35,7% de pacientes independientes al final del seguimiento. Los únicos factores que reducen de forma independiente la estancia y la mortalidad son la atención por neurología durante el ingreso y una menor discapacidad al ingreso.
ConclusiónLa atención especializada por neurología es eficaz y coste-efectiva por la reducción en estancia hospitalaria, mortalidad y dependencia. La implantación de neurología en los hospitales comarcales de Andalucía es prioritaria para garantizar la equidad en el territorio nacional. Este objetivo debería incluirse en el Plan Andaluz de Atención al Ictus como paso previo para constituir una red de equipos/unidades de ictus.
According to the Spanish National Institute of Statistics, acute cerebrovascular disease is the leading cause of death in women and the second cause of death worldwide. It is also the leading cause of disability in adults and the second cause of dementia. It accounts for 3%–4% of all health care spending.1–3
Stroke mortality rate in Andalusia is twice that in other Spanish autonomous communities. As a consequence, this disease is one of the main social and healthcare problems in that region.4–6 Therefore, treatment for this expensive, prevalent, disabling and fatal disease needs to be improved in Andalusia.
Beginning in the 1980s, studies began to be published which reported that specialised stroke care has an impact on patient outcomes. Stroke units (SU) have clearly shown themselves to be effective in reducing mortality rates and delivering better functional recovery (level of evidence I and recommendation level A).7 For all types of stroke, SUs provide long-term benefits that are independent of age and disease severity.8–10
Spain's stroke care plan (PASI in Spanish),11 drawn up by the Spanish Society of Neurology's Study Group for Cerebrovascular Diseases, has recently been revised (PASI II).12 Its objective is to establish an organised system for stroke care in order to meet each patient's needs and optimise the use of healthcare resources, thereby guaranteeing equal care for all stroke patients.13,14 Spain's National Health System stroke care strategy,15 drawn up by the Ministry of Health and Social Policy, uses the type of organisational model for healthcare described by the PASI. The aim of this strategy was to homogenise stroke care by requiring regional Ministries of Health to develop and implement those healthcare plans.
In the first half of 2009, a survey was carried out with the aim of evaluating the real situation of neurological care for acute stroke. According to this survey, Andalusia is behind all other regions in stroke care, and failing to progress according to the lines of the SNS stroke care strategy.16,17 There is only 1 SU bed for every 1,037,500 inhabitants in Andalusia, whereas other regions such as Aragon, Catalonia, the Balearic Islands, the Canary Islands, Cantabria, Castile-Leon, Madrid, Navarre and the Basque Country have at least 1 bed for every 200000 inhabitants. This lack of equality in care is accentuated by the fact that neurologists are absent from half of all Andalusian hospitals; only 3 of the 17 local hospitals (known as level III and IV hospitals in Andalusia) include neurologists in their internal medicine departments.18
The aim of this study was to evaluate the impact of the 2006 decision to include a neurologist among the personnel at Hospital Infanta Elena (HIE) for the care and monitoring of stroke patients.
Patients and methodsRetrospective cohort study of the incident cases of stroke admitted to HIE during the first quarter of 2006. We evaluated all the patients admitted to the hospital due to ischaemic stroke, haemorrhagic stroke, or transient ischaemic attack (TIA) between 1 January and 31 March 2006. Patients with TIA were excluded from later analyses. When selecting patients, we took into account the diagnosis on the discharge report.
The main study variable was whether care was provided by a neurologist or a general practitioner during the patient's hospital stay. Patients were admitted by one department or another depending on the age and severity of the patient's clinical state, and on whether or not there was a neurologist in the hospital. According to the procedure, the youngest patients and the ones in the most serious condition were referred to the neurology department, unless there was no neurologist in the hospital on the day of admission.
We analysed stroke subtype, age, hospital stay, dependence upon admission and mortality rate during hospitalisation for each of the groups. We also analysed other quality indicators for the integrated care process for cerebrovascular accidents19 (thorough clinical assessment, Doppler ultrasound during the hospital stay, and echocardiography in suspected cases of cardioembolic stroke).
The neurology department retrospectively collected this data from patient's medical histories according to the definitions below.Patients described as having had a thorough clinical assessment were those who had undergone at least 1 complete neurological examination during the hospital stay (assessment of language, cranial nerves, motor and sensory systems). The discharge report was required to include the stroke subtype (ischaemic or haemorrhagic), topographic diagnosis (hemispheric or vertebrobasilar in ischaemic stroke; lobar, in basal ganglia, in brainstem or cerebellum in haemorrhagic stroke) and aetiological diagnosis (lacunar, thrombotic, cardioembolic, or artery-to-artery embolism in ischaemic stroke; hypertensive, amyloid angiopathy, arteriovenous malformation, etc. in haemorrhagic stroke). We also accepted other synonyms or terms more specific than those listed above.Dependence upon admission was measured using the modified Rankin scale20 extrapolated from clinical assessments. This score took into account motor impairment only, as follows: 0 (asymptomatic), 1 (clumsiness in one hand), 2 (4/5 limb weakness; patient is able to walk unaided), 3 (0–3/5 limb weakness; patient needs help walking), 4 (patient unable to walk, but fully conscious and able to interact with others), 5 (patient unable to walk, suffers from decreased levels of consciousness and interaction, and cannot be left alone at any time) and 6 (death).
We also completed a prospective cohort study in December 2006 by reviewing patients. Those patients who did not attend their appointments were contacted by telephone. Variables analysed at the end of the follow-up period were dependence in activities of daily living, mortality rate, and institutionalisation rate. The information was collected from a direct interview with the patient and/or family members. Degree of disability was determined by using the modified Rankin scale.
We also compared the monthly gross mortality rate among stroke patients admitted to HIE between January and December 2006 and the percentage of patients treated by general practitioners. Inclusion criteria for these patients were the same as those described above. The recruitment period was extended to 15 December 2006.
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS, Chicago, IL), version 14.0. The sample was described using absolute and relative frequencies from each category for qualitative variables. Quantitative variables were described using the median and standard deviations (for the Rankin scale, we used the median and the interquartile range). Bivariate correlations were analysed using the Pearson correlation coefficient. The differences among qualitative variables were studied with the chi-square test. We used Fisher's exact test when the expected frequency of any of the cells was less than 5. The t-test for independent data was used to compare the means of quantitative variables after comparing equality of variances using Levene's test. In the follow-up study, we used the cumulative incidence of expected events to calculate their relative risk for a 95% confidence interval. Alpha error was set at 0.05.
In the multivariate study, we used a logistic regression analysis with simultaneous introduction of all covariates.
ResultsEvaluation of patients admitted to hospital due to cerebrovascular pathology during the first quarter of 2006.
During the first quarter of 2006, 116 patients were admitted to HIE due to cerebrovascular pathology. Similar-sized groups of patients were treated by neurologists and by general practitioners, but stroke types differed between the 2 groups. Patients treated by neurologists had significantly higher numbers of intracranial haemorrhages and fewer TIAs. Mean age was significantly lower and degree of disability was significantly higher in patients treated by neurologists (Tables 1 and 2).
Characteristics of patients with a cerebrovascular disease admitted to the hospital during the first quarter of 2006.
| Total group (n=116) | Neurology (n=56) | General medicine (n=60) | P | |
| Types of stroke | ||||
| Ischaemic stroke | 85 | 73.2% (41) | 73.3% (44) | NS |
| ICH | 17 | 23.2% (13) | 6.7% (4) | 0.001 |
| TIA | 14 | 3.6% (2) | 20% (12) | 0.001 |
| Age (years), mean±SD | 70.72±13.5 | 65.6±13.6 | 75.7±11.5 | <0.001 |
| Hospital stay (days), mean±SD | 6.62±5 | 5.38±3.9 | 7.83±5.5 | 0.007 |
TIA: transient ischaemic attack; ICH: Intracranial haemorrhage; NS: not significant.
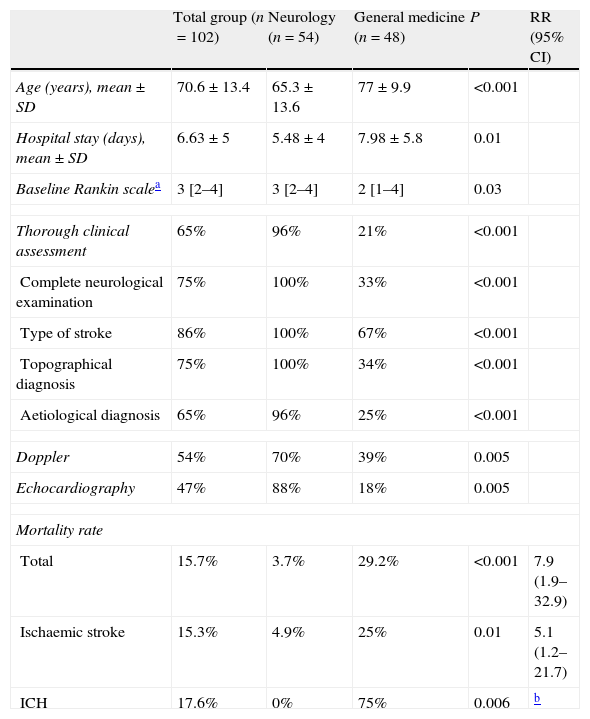
Characteristics of ischaemic and haemorrhagic strokes and quality indicators at admission.
| Total group (n=102) | Neurology (n=54) | General medicine (n=48) | P | RR (95% CI) | |
| Age (years), mean±SD | 70.6±13.4 | 65.3±13.6 | 77±9.9 | <0.001 | |
| Hospital stay (days), mean±SD | 6.63±5 | 5.48±4 | 7.98±5.8 | 0.01 | |
| Baseline Rankin scalea | 3 [2–4] | 3 [2–4] | 2 [1–4] | 0.03 | |
| Thorough clinical assessment | 65% | 96% | 21% | <0.001 | |
| Complete neurological examination | 75% | 100% | 33% | <0.001 | |
| Type of stroke | 86% | 100% | 67% | <0.001 | |
| Topographical diagnosis | 75% | 100% | 34% | <0.001 | |
| Aetiological diagnosis | 65% | 96% | 25% | <0.001 | |
| Doppler | 54% | 70% | 39% | 0.005 | |
| Echocardiography | 47% | 88% | 18% | 0.005 | |
| Mortality rate | |||||
| Total | 15.7% | 3.7% | 29.2% | <0.001 | 7.9 (1.9–32.9) |
| Ischaemic stroke | 15.3% | 4.9% | 25% | 0.01 | 5.1 (1.2–21.7) |
| ICH | 17.6% | 0% | 75% | 0.006 | b |
TIA: transient ischaemic attack; ICH: intracranial haemorrhage; CI: confidence interval; NS: not significant; RR: relative risk.
Table 2 shows the data from the quality indicator analysis during hospitalisation in the total group of patients with ischaemic or haemorrhagic stroke, broken down by specialty.
The mean hospital stay for stroke patients was significantly shorter among those treated by neurologists (P=.001).
A complete diagnostic evaluation was performed in 96% of the patients treated by a neurologist vs 21% of patients treated by a general practitioner (P<.001).
A cervical Doppler ultrasound was performed during hospitalisation in 70% of the cases of ischaemic stroke treated by a neurologist, and in only 39% of those cases treated by a general practitioner (P=.005).
Echocardiography was performed in 88% of the suspected cases of cardioembolic stroke treated by neurologists and in only 18% of the cases treated by general practitioners (P=.005).
The mortality rate was significantly lower in the neurology department, (3.7% vs 29.2%) for cases of both ischaemic stroke (4.9% vs 25%) and haemorrhagic stroke (0% vs 75%); the relative risk of death was 7.9 for patients treated by a general practitioner (P<.001).
Patients with ischaemic and haemorrhagic stroke admitted to hospital during the first quarter of 2006 were monitored during a mean follow-up period of 9.1±3.4 months. At the end of follow-up, rates of mortality, dependence, and admission to assisted living centres were significantly higher in the group of patients who were not treated by a neurologist during hospitalisation. The relative risks of death, dependence, and being institutionalised were 6.5, 2.15, and 5 respectively (Table 3).
Quality indicators of stroke during patient follow-up.
| Total group (n=102) | Neurology (n=54) | General medicine (n=48) | P | RR (95% CI) | |
| Follow-up time (months), mean±SD | 9.1±3.4 | 8.5±3.8 | 10.3±2.3 | NS | |
| Dependence for ADLsa | 48.1% | 31% | 66.7% | 0.001 | 2.15 (1.3–3.56) |
| Mortality rate | 25.9% | 7.1% | 46.2% | <0.001 | 6.5 (2.1–20.2) |
| Institutionalisation | 13.2% | 5% | 25% | 0.02 | 5 (1.1–22.3) |
CI: confidence interval; NS: not significant; RR: relative risk.
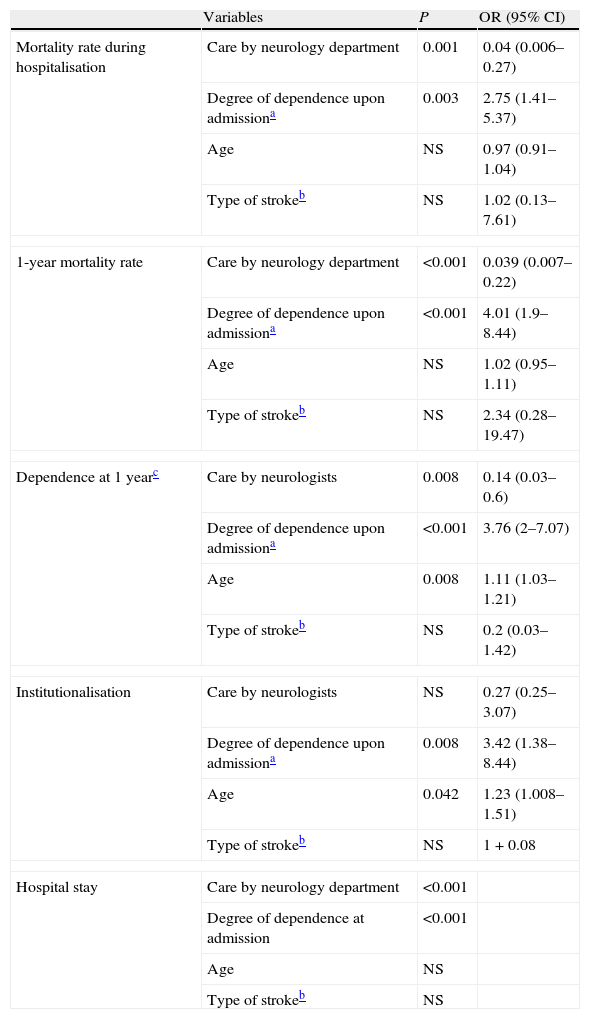
After scores were adjusted for the patient's age and stroke type, the multivariate analysis (Table 4) revealed that neurological care during hospitalisation and a low degree of disability upon admission are the factors associated with independent and significant decreases in hospital stay length, mortality rate (during hospitalisation and at 1 year), and dependence (at one year). Age was not associated with the length of the hospital stay or the mortality rate. However, younger age was linked to a significant and independent increase in the probability of being independent for activities of daily living 1 year after the stroke. Only the degree of dependence upon admission and the patient's age had a significant influence on institutionalisation.
Multivariate analysis of the impact of the different characteristics stroke characteristics on the quality indicators at admission.
| Variables | P | OR (95% CI) | |
| Mortality rate during hospitalisation | Care by neurology department | 0.001 | 0.04 (0.006–0.27) |
| Degree of dependence upon admissiona | 0.003 | 2.75 (1.41–5.37) | |
| Age | NS | 0.97 (0.91–1.04) | |
| Type of strokeb | NS | 1.02 (0.13–7.61) | |
| 1-year mortality rate | Care by neurology department | <0.001 | 0.039 (0.007–0.22) |
| Degree of dependence upon admissiona | <0.001 | 4.01 (1.9–8.44) | |
| Age | NS | 1.02 (0.95–1.11) | |
| Type of strokeb | NS | 2.34 (0.28–19.47) | |
| Dependence at 1 yearc | Care by neurologists | 0.008 | 0.14 (0.03–0.6) |
| Degree of dependence upon admissiona | <0.001 | 3.76 (2–7.07) | |
| Age | 0.008 | 1.11 (1.03–1.21) | |
| Type of strokeb | NS | 0.2 (0.03–1.42) | |
| Institutionalisation | Care by neurologists | NS | 0.27 (0.25–3.07) |
| Degree of dependence upon admissiona | 0.008 | 3.42 (1.38–8.44) | |
| Age | 0.042 | 1.23 (1.008–1.51) | |
| Type of strokeb | NS | 1+0.08 | |
| Hospital stay | Care by neurology department | <0.001 | |
| Degree of dependence at admission | <0.001 | ||
| Age | NS | ||
| Type of strokeb | NS | ||
We found a positive correlation between the mortality rate observed every month and the percentage of patients treated by a general practitioner (r=0.63; P=0.02) (Fig. 1). We observed the highest mortality rate among patients referred to a general practitioner in the absence of a neurologist.
DiscussionIn 2003, the European Stroke Initiative published updated treatment guidelines emphasising the need for stroke patients to be treated by neurologists.21 In both PASI8 and the SNS stroke care strategy,15 neurologists are listed as the coordinators of stroke care teams at local hospitals. In contrast, the Andalusian stroke care plan18 does not list adding neurologists to its hospitals among its objectives, and stroke care teams do not include this specialty. However, this plan does promote universal administration of thrombolytic treatment in all hospitals.
As evidenced by the current study, neurological care for stroke patients is associated with a precise diagnosis, the use of complementary tests, and better identification of stroke aetiologies. These factors are crucial for selecting a specific therapeutic approach and establishing proper secondary prevention strategies which entail a lower risk of recurrence and lower dependence and mortality rates. This study shows that stroke patients cared for by neurologists at Andalusian local hospitals have lower mortality rates during hospitalisation. There is a 39% absolute decrease in mortality which remains constant over the long term, and a 35% absolute increase in the number of patients who are independent after 9 months of follow-up. This association becomes even more noticeable when we discover the significant and positive correlation between the mortality rates observed for each month in 2006 and the percentage of patients who were not cared for by neurologists during hospitalisation. By this logic, neurology appears to be a necessary specialty.
Other studies carried out in Spain22,23 and other countries24,25 also attest to the benefits of specialised neurological care. In Spain, the PRACTIC study22 included patients with acute stroke from 88 hospitals. The study revealed that admitting patients to the neurology department resulted in fewer complications and relapses, a lower mortality rate during hospitalisation, and more patients being independent after 6 months of follow-up.
The current study shows more significant differences than the PRACTIC study with regard to the outcomes of patients treated by a neurologist and outcomes of those treated by a general practitioner. This may be due to the fact that the PRACTIC study did not include local hospitals without a neurology department, a description which fits 14 local hospitals in Andalusia and was also true of HIE until late 2005. The lack of familiarity with the most recent stroke care practices displayed by general practitioners at these hospitals may result in poorer care and outcomes for stroke patients. In fact, if general practitioners were to receive training in neurology, the significant differences in patient outcomes would gradually disappear. Were this to occur, it would still not detract from the importance of having a neurologist at every Andalusian local hospital. Instead, further training for general practitioners would be an additional benefit of including this specialty in hospitals.
This study also reveals that care by neurologists is cost-effective, since it results in shorter hospital stays and lower mortality and dependence rates. We know that the patient's level of disability is the main factor determining the cost of stroke; in fact, care for patients who survive the stroke with a disability is 5 times more expensive than care for independent patients.26 If we extrapolate the results to the number of patients with stroke and infarct (GRD 14) admitted to Andalusian hospitals in 2006,27 it seems that having neurology departments in all the hospitals would prevent 1916 deaths and 1719 cases of dependence yearly. A decrease of 1719 dependent patients every year would entail significant cost savings for the healthcare system in the areas of physical therapy, outpatient care, and institutionalisation, in addition to the savings in indirect or social costs of stroke, such as lost years of work for patients and working hours provided by carers. In any case, this extrapolation is merely a model illustrating the impact of providing neurological care to all patients with ischaemic stroke in Andalusia, since each hospital may follow different stroke care procedures.
The current study has some methodological limitationsThe Rankin scale is not appropriate for evaluating the severity of acute strokes. However, given that medical histories did not include the NIH stroke scale, we opted to establish stroke severity by using the motor deficit reported in the medical history and comparing this deficit to a score on a dependence scale. Nonetheless, the Rankin scale is appropriate for assessing patients during follow-up. In this case, the assessment was carried out conventionally.The current study did not take into account the comorbidities that may have affected patient outcomes. Furthermore, the data gathering process was not blinded. Both circumstances may have created biases affecting the validity of the study. However, certain robust variables such as mortality rate cannot be influenced by whether or not the study is blinded.
Stroke care in Andalusia presents some definite problems. There are no neurologists in half of all Andalusian hospitals (1883264 inhabitants would have no access to neurological care if they were hospitalised). Andalusia is ranked last among Spain's autonomous communities by the number of inhabitants for every SU bed. Considering that the entire region has only 2 stroke units, there are 1037500 inhabitants for every bed.16 Access to neurological care and the presence of SU are clearly associated with decreased mortality from stroke.7,8,21,22,28–32 The lack of both of these measures is probably a determining factor for the high stroke mortality rate in Andalusia. Some researchers have linked the high mortality rate in what is known as Spain's ‘stroke belt’ to socioeconomic differences, risk factors, and the prevalence of chronic diseases.33 However, these factors are probably more related to increased stroke incidence than they are to higher stroke mortality.34
Following in the footsteps of other autonomous communities, the Andalusian stroke care plan should consider including neurologists in every local hospital in Andalusia as a necessary first step in the process of organising a healthcare network.35 In a best-case scenario, these neurologists would work in partnership with the neurology units at their corresponding hospitals of reference, by using multi-hospital management units. Such a system has already been implemented in Huelva province, where the neurologist at Hospital Infanta Elena cooperates with neurologists at Hospital Juan Ramón Jiménez. This approach may promote the implementation of the SNS stroke care strategy by creating a network of professionals and SUs. Taking this step would be a decisive move in order for stroke care in Andalusia to be comparable with that in the rest of the country.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez Fernández E, et al. Repercusión de la introducción de neurología en un hospital comarcal de Andalucía. Neurología. 2012;27:400–6.