Acute torticollis is a frequent reason for consultation with paediatrics departments. The aetiology varies1; severe underlying diseases must therefore be ruled out.
Intervertebral disc calcification, an infrequent condition in paediatric patients, has been described as a cause of painful torticollis. We present the cases of 3 patients with torticollis secondary to intervertebral disc calcification attended at our centre, a tertiary hospital, over the past 20 years, and review the literature on this entity.
The patients were aged 5, 6, and 10 years old; the series includes 2 boys and one girl. All 3 patients presented sudden-onset torticollis and deviation of the head (to the right in 2 cases and to the left in 1). Only one of the patients had presented self-limited episodes previously (4 similar episodes in the previous 2 months, lasting 3–8 days). One patient had history of minor trauma. Time from symptom onset to diagnosis ranged from 5 to 10 days.
The physical examination revealed deviation of the head to the side of torticollis, shoulder asymmetry, elevation of the ipsilateral scapula, limited head extension, and mild contracture of the ipsilateral sternocleidomastoid and trapezius muscles. All 3 patients were in good general health, and neurological examination revealed no other pathological findings in any of them.
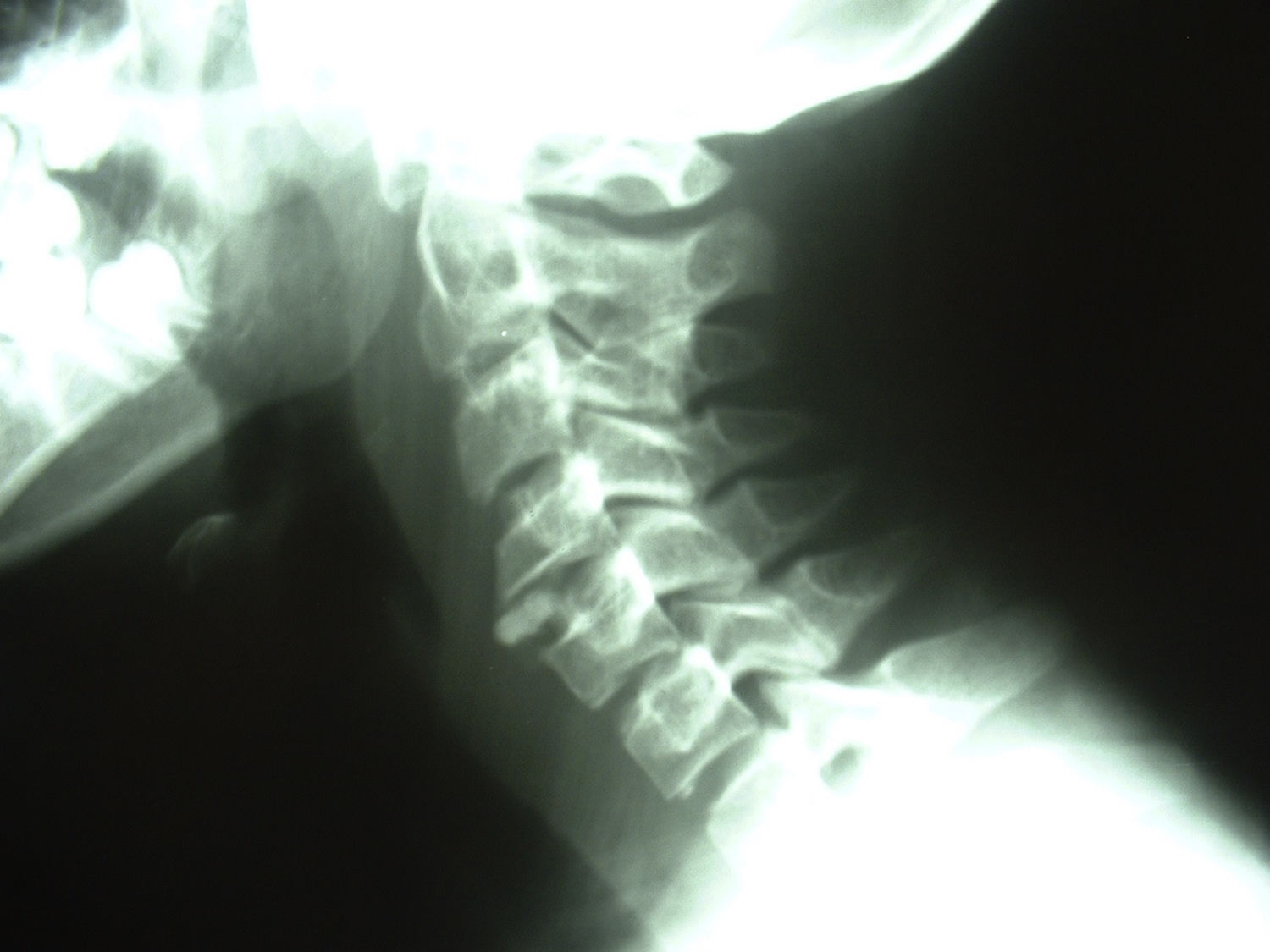
Cervical and thoracic spine radiography revealed signs of intervertebral disc calcification in all cases. In 2 patients, calcifications were observed in a single intervertebral space (C3-C4 and C2-C3), whereas the remaining patient showed calcifications at multiple locations (C4-C5, C7-T1, T2-T3, and T5-T6) (Fig. 1). Spinal cord involvement was not observed in any patient. Calcification was confirmed with MRI (Fig. 2). Two of the patients underwent a complete blood count; a biochemical study; tests for calcitonin, PTH, hydroxyproline, pyridinoline, and thyroid hormone levels; tests of calcium and phosphorus metabolism; erythrocyte sedimentation rate; renal function studies; and urine tests. All results were normal.
Patients received anti-inflammatory and analgesic treatment (non-steroidal anti-inflammatory drugs), and symptoms resolved after 5 to 35 days. Radiological progression varied. In one patient, calcification disappeared at 3 months, whereas another patient showed no changes at 4 months. The remaining patient underwent no follow-up radiology studies.
Intervertebral disc calcification is rare among the paediatric population. Beluffi et al.2 conducted a retrospective study of radiographs taken over 26 years from patients aged 0 to 18 years, and identified intervertebral disc calcification in 6 patients; the condition was asymptomatic in one patient. Calcification may affect the intervertebral discs, vertebral bodies, muscles, or ligaments, causing cervical pain, sensorimotor alterations, or torticollis. The aetiology is unknown, but local inflammation of the nucleus pulposus is a possible explanation. Other possible causes include hypervitaminosis D, metabolic disorders, and haemolytic anaemia. On occasion, intervertebral disc calcification is an incidental finding.2
Over 300 cases of intervertebral disc calcification have been reported since the condition was first described by Baron in 1924.3 The condition is more frequent among children aged 6 to 10 years, and predominantly affects boys.4,5 The cervical spine is involved in 70% of cases, and 35% of patients show calcification of more than one intervertebral disc space. The lumbar spine is the least frequently affected location. Cervical involvement is the most symptomatic, causing symptoms in 83% of cases (vs 24% in cases of lumbar involvement). The most frequent symptom is cervical pain, followed by sensorimotor alterations and fever,6 particularly when calcifications have nearly resolved. The condition causes persistent or recurrent torticollis in 23% of cases.3
Diagnosis is established according to cervical radiography, CT, or MRI findings. Alterations in calcium and phosphorus metabolism should be ruled out. Most patients are treated conservatively with non-steroidal anti-inflammatory drugs and rest; a cervical collar may be used if symptoms persist. Surgery (laminectomy) is indicated if the patient presents neurological deficits or symptoms of spinal cord compression.7,8 The condition usually resolves spontaneously. In 70% of cases, pain resolves within a month, with calcifications usually disappearing between 28 days and 6 months after symptom onset.9 Calcifications disappeared spontaneously in all 3 of our patients. Follow-up of these patients helps confirm spontaneous resolution of intervertebral disc calcification, which in turn confirms the diagnosis and rules out other conditions.
Please cite this article as: Fernández Gómez A, Bernal Calmarza R, Monge Galindo L, Luis Peña Segura J. Calcificación de discos intervertebrales como causa de tortícolis dolorosa en edad pediátrica. Neurología. 2020;35:419–421.