The fogging effect is a radiological phenomenon occurring in the subacute phase of ischaemic stroke. It consists of attenuation or even transient disappearance of hypodensity in the cerebral parenchyma in radiological images due to an ischaemic lesion, and it usually takes place around the second or third week after stroke. As a result, a brain computed tomography (CT) performed during that period may yield apparently normal results.1 The fogging effect has also been described in MR images.2
We present the cases of 2 patients with extensive infarctions who exhibited this effect in brain CT images.
Case 1The first patient, a 68-year-old woman with a history of arterial hypertension, was found at home with a low level of consciousness. She was intubated and received mechanical ventilation upon arriving at the emergency department. The patient's eyes remained closed during the neurological examination, which revealed nociceptive flexion reflex of the limbs, mydriatic and nonreactive midposition pupils, absent oculocephalic reflexes, generalised hypotonia, and bilateral Babinski sign. An emergency brain CT scan was performed, yielding normal results. Subsequently, a CT angiography of the intracranial arteries showed a filling defect compatible with basilar artery thrombosis.
The patient was referred to another hospital where she underwent mechanical thrombectomy. Complete recanalisation of the basilar artery was achieved 24hours after symptom onset. Another neurological examination was performed after surgery while the patient was still intubated and sedated; although her eyes did not open, she was able to follow simple instructions. Her gaze remained centred and pupils showed little reaction to light. Left supranuclear facial paresis and left-sided weakness were observed.
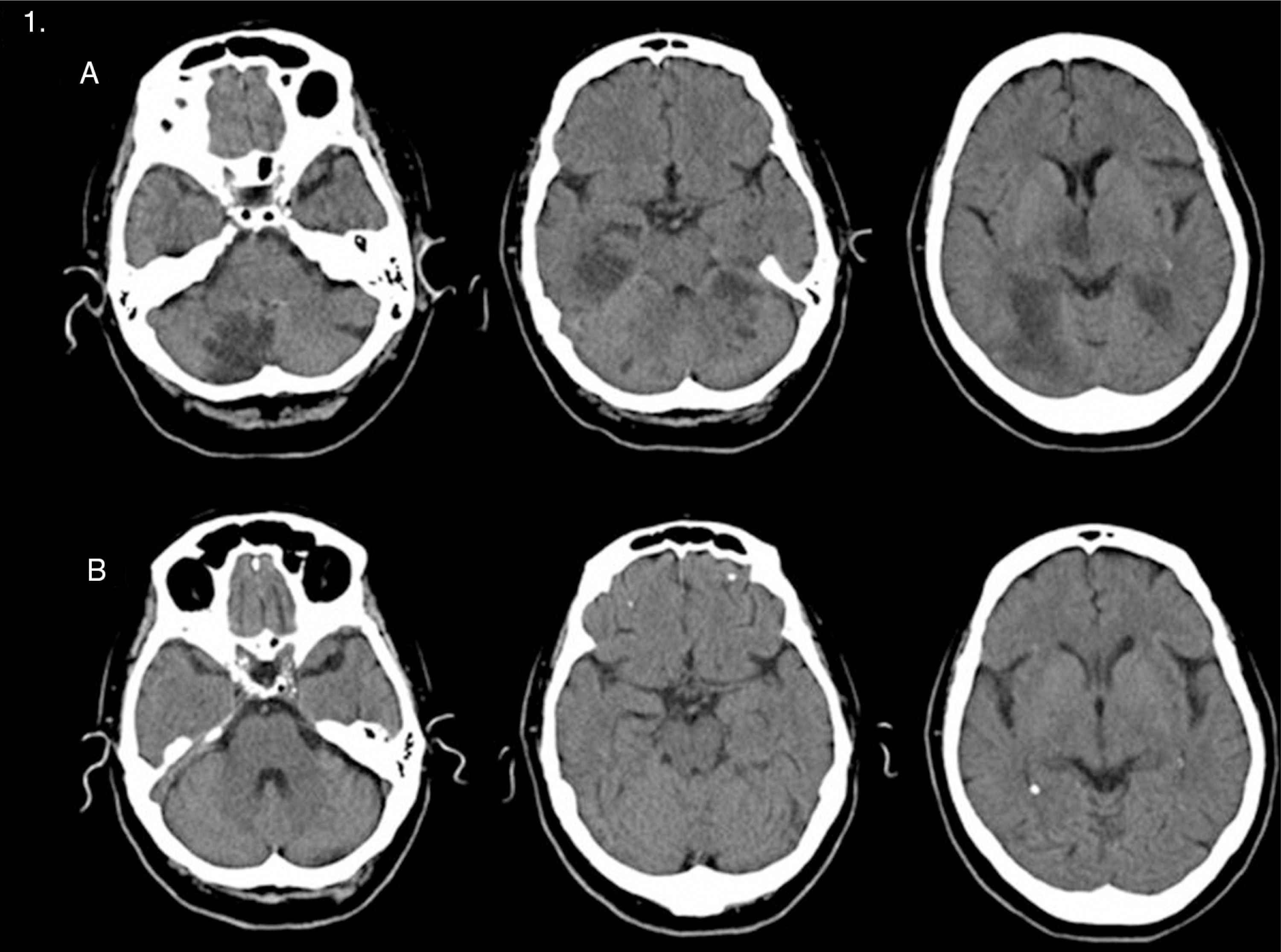
Four days after the ischaemic episode she was referred to our hospital and admitted to the intensive care unit (ICU). A control CT scan showed bilateral development of ischaemic lesions affecting virtually all of the posterior territory (Fig. 1A).
(A) A simple transverse CT scan performed 4 days after stroke displays multiple infarcts affecting the territory of both posterior cerebral arteries, right thalamus, and medial midbrain. (B) Simple transverse CT scan performed 18 days later showing apparent resolution of the lesions.
However, these lesions could not be seen on a follow-up CT scan performed 18 days later (Fig. 1B).
After 20 days at the ICU, the patient was transferred to the neurology department. No relevant neurological changes were observed. Two months later, she was transferred to a long-stay hospital.
Case 2The second case was a 77-year-old woman with a history of arterial hypertension, dyslipidaemia, chronic atrial fibrillation, obesity, sedentary lifestyle, and a 10-year history of residual facial palsy and visual field alterations secondary to ischaemic stroke in the territory of the right middle cerebral artery (MCA). She experienced impaired language production and comprehension with sudden-onset right-sided weakness, and was therefore sent to our hospital as part of the ‘code stroke’ protocol.
Upon arriving at the emergency department (2h 55min after symptom onset), the patient was unable to respond to simple instructions or speak. She also presented left-sided deviation of head and eyes, right-sided hemianopsia, hemiplegia, hypoaesthesia, right-sided neglect, and a score of 24 on the National Institutes of Health Stroke Scale (NIHSS).
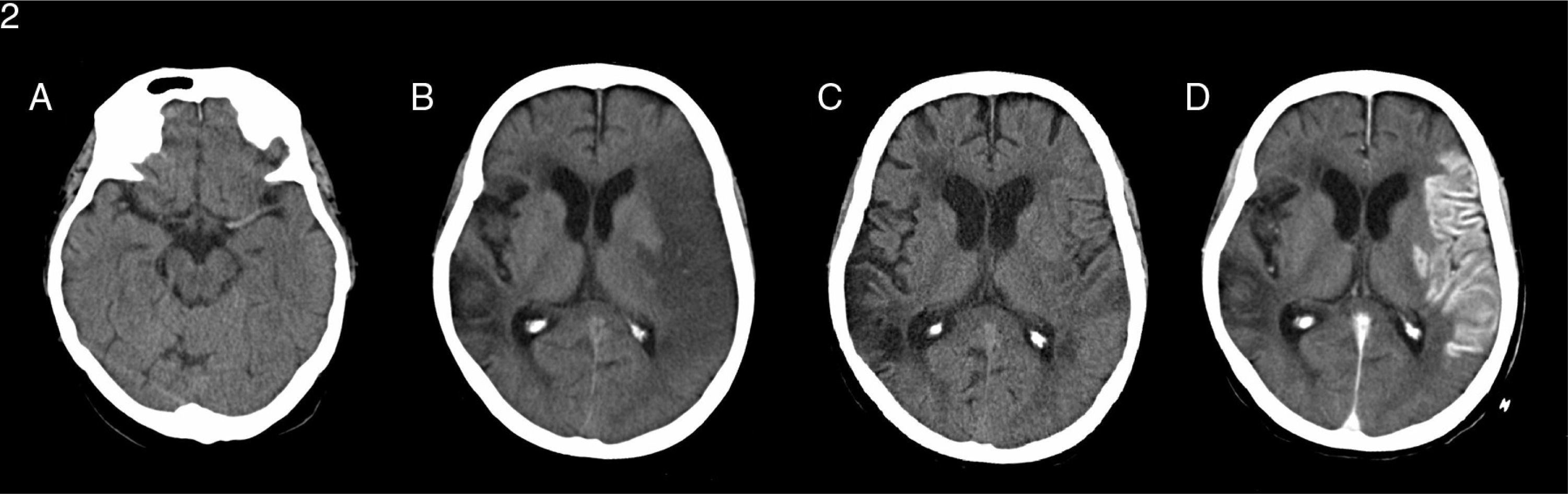
An emergency brain CT scan revealed spontaneous hyperdensity of the left MCA, an acute ischaemic lesion in the territory supplied by that artery (4 on the Alberta Stroke Programme Early CT Score scale), and an old ischaemic lesion in the right frontoparietal region (Fig. 2A). An emergency transcranial duplex ultrasound showed a TIBI (Thrombolysis In Brain Ischaemia) flow grade 1 at a depth of 63mm and compatible with proximal occlusion of the left MCA. CT angiography evidenced intracranial occlusion of the internal carotid artery affecting the ostium of the MCA and the anterior cerebral artery (‘carotid T occlusion’). Perfusion CT showed no areas of penumbra.
(A) A simple transverse CT scan performed when the patient arrived at the emergency department displays spontaneous hyperdense left MCA. (B) Simple transverse CT scan performed 24hours after stroke demonstrating an extensive hypodense area in the cortical-subcortical region affecting most of the territory of the left MCA, compatible with extensive subacute infarction in that area with a discrete mass effect on the left lateral ventricle. Malacia/gliosis can be observed in areas of the right hemisphere along the edge of old ischaemic lesions. (C) Simple transverse CT scan performed 10 days later showing less extensive hypoattenuated areas mainly affecting the peripheral territories, but also deep territories, in the corona radiata and left inner capsule. (D) A contrast CT scan was subsequently performed and showed pronounced gyriform cortical enhancement in the territory of the left MCA compatible with luxury perfusion in cortical and deep lesions secondary to subacute infarct.
In view of the radiological findings, reperfusion therapies were ruled out.
A control CT study was performed 24hours after symptom onset and showed hypodensity in the cortical-subcortical area affecting almost all the territory of the left MCA (Fig. 2B). The patient underwent another transcranial duplex ultrasound which revealed resolution of the occlusion described above.
A control CT scan performed 10 days later displayed less extensive hypoattenuated areas, and a contrast CT scan showed marked enhancement in that territory (Fig. 2C and D).
The patient experienced slight improvements during hospitalisation, but died 28 days later due to a massive bilateral pulmonary thromboembolism.
DiscussionIn 1979, Becker et al.1 observed that hypodensities initially displayed in brain CT scans temporarily disappeared during the acute phase of ischaemic stroke in some patients; they called this phenomenon the ‘fogging effect’. This effect has subsequently been described in brain MRI as well, in both T1- and T2-weighted sequences and in FLAIR sequences.2 Images taken using either technique may display transient isodensity or normal intensity in the infarcted area, and contrast material may be necessary in order to identify the infarction.1
This phenomenon can be observed in up to 50% of all cases and it is more frequently reported during the second and third weeks after an ischaemic stroke.3 Fogging has been described in both hemispheric and posterior territory ischaemic strokes.
The fogging effect has been linked to the ‘luxury perfusion’ phenomenon, defined as increased blood flow in advanced stages of ischaemic stroke that is insufficient to restore infarcted brain tissue. Brain SPECT studies have confirmed that blood flow increases in the ischaemic area during the subacute phase.4 Some researchers have suggested that increased blood flow associated with luxury perfusion masks radiological hypodensities during that phase.4
Other theories seeking to explain the fogging effect postulate the development of mild haemorrhagic transformations, proliferation of capillaries and decrease in bulk water in the infarcted area, or macrophage infiltration into the infarcted tissue as potential causes for this phenomenon.1,3
The 2 cases presented here experienced large-calibre vessel occlusion (basilar artery and terminal carotid artery) and late recanalisation of those occlusions did not result in any clinical improvement. The term ‘futile recanalisation’ refers to a situation in which recanalisation of an occluded artery fails to prevent extensive ischaemic stroke and thus does not improve patients’ functional outcomes.5
Although different mechanisms restored cerebral blood flow in these 2 patients (mechanical thrombectomy in the first patient and spontaneous recanalisation in the second), final outcomes were the same: late, ineffective recanalisation of the infarcted tissue.
The clinical cases presented here support the theory that establishes a connection between the fogging effect and the luxury perfusion phenomenon. The fogging effect may be a radiological manifestation of futile recanalisation and reflect the luxury perfusion phenomenon occurring in the infarcted tissue of these patients.
Further studies based on this hypothesis are necessary to elucidate the connection between the fogging effect and futile recanalisation.
Please cite this article as: Iglesias-Mohedano AM, García-Pastor A, Contreras-Chicote A, Villanueva-Osorio JA. ¿Está relacionado el fogging effect con la recanalización fútil?. Neurología. 2015;30:447–449.