Cerebral venous thrombosis (CVT) is an uncommon cause of stroke that mainly affects young adults. Early, accurate diagnosis can reduce the rate and severity of complications.
ObjectiveThe aim of this study was to analyse the clinical characteristics, management, and treatment of CVT in different centres in Spain.
MethodsWe conducted a multicentre, retrospective, descriptive study of patients hospitalised due to CVT between 2008 and 2017 at 10 Spanish centres.
ResultsWe included 256 patients, with a mean age (SD) of 49.8 (18.7) years; 51% of patients were women. The most frequent symptoms were headache (73%), focal deficits (50%), epileptic seizures (33%), and encephalopathy (21%). The most frequent localisations were the superior sagittal sinus (12.5%), the transverse sinus (10.9%), and 2 or more sinuses or veins (66.4%). Thrombophilia was the most frequent known aetiology (24%), and was most commonly associated with the prothrombin G20210A mutation (19%). Forty-six percent of patients were treated with antithrombotics for 3 to 6 months, 21% for one year, and 22.6% required indefinite anticoagulation. Endovascular therapy was performed in 5% of cases, and 33% required neurosurgery. Regarding outcomes, 75% of patients were independent at 3 months (modified Rankin Scale [mRS] score ≤ 2), with papilloedema (P = .03), focal deficits (P = .001), and encephalopathy (P < .001) showing a statistically significant association with poor prognosis (mRS > 3). The in-hospital mortality rate was 4.3%, with a 3-month mortality rate of 6.3%.
ConclusionThe diverse risk factors and variable presentation of CVT represent a challenge in the diagnosis and treatment of this condition. To improve prognosis and reduce mortality, it is essential to establish management protocols for this entity.
La trombosis venosa cerebral (TVC) es una causa poco común de ictus que afecta principalmente a adultos jóvenes. Un diagnóstico precoz y preciso puede reducir la tasa y gravedad de las complicaciones.
ObjetivoAnalizar las características clínicas, manejo y tratamiento de la TVC en diferentes centros de nuestro país.
MétodosEstudio descriptivo retrospectivo multicéntrico de pacientes hospitalizados por TVC entre 2008 y 2017 en 10 centros sanitarios en nuestro país.
ResultadosSe incluyeron 256 pacientes, edad media 49,8 ± 18,7 años y el 51% fueron mujeres. Los síntomas más frecuentes fueron: cefalea (73%), déficits focales (50%), crisis epilépticas (33%) y encefalopatía (21%). Las localizaciones más frecuentes fueron: seno longitudinal superior (12,5%), transverso (10,9%) y afectación de dos o más senos o venas (66,4%). La etiología conocida más frecuente fue la trombofilia (24%), siendo la mutación de la protrombina G20210A la más común (19%). El 46% fue tratado con antitrombóticos durante 3-6 meses, el 21% durante 1 año y un 22,6% de los pacientes requirieron anticoagulación indefinida. En un 5% de los sujetos fue preciso terapia endovascular y un 33% requirió neurocirugía. En relación al pronóstico, el 75% fueron independientes a los 3 meses con una puntuación en la escala de Rankin modificada (mRS) ≤ 2 y la presencia de papiledema (p = 0,03), déficit focal (p = 0,001) y encefalopatía (p < 0,001) se relacionaron significativamente con mal pronóstico (mRS > 3). La tasa de mortalidad intrahospitalaria fue del 4,3% y el 6,3% de los pacientes fallecieron a los 3 meses.
ConclusiónLa diversidad de factores de riesgo y la presentación variable suponen un desafío en el diagnóstico y tratamiento de la TVC. Para mejorar el pronóstico y reducir la mortalidad es fundamental la instauración de protocolos en el manejo de esta patología.
In normal circumstances, almost 80% of cerebral blood volume is located in venous structures; despite this, cerebral venous thrombosis (CVT) is much less prevalent than ischaemic stroke, representing only 0.5% to 1% of cases of cerebrovascular disease.1 Its incidence is estimated between 3 and 4 cases per million population, with higher rates in neonates and young children (7 cases per million).2
The main features differentiating it from arterial disease include its predominance among younger patients and women, with the latter being linked to specific aetiological aspects associated with female sex, such as pregnancy, puerperium, and the use of oral contraceptives (OC).3–5
Another characteristic trait of venous cerebrovascular disease is the great anatomical variability of the venous system, with imprecise venous drainage, especially in the superficial system. Cerebral veins and dural sinuses lack valves or tunica layers, which affords them great compensatory capacity in the event of thrombosis. Furthermore, the presence of multiple anastomoses between cortical veins facilitates collateral circulation in thrombosis of the superficial system.
All these peculiarities of the venous system result in significant heterogeneity in the clinical presentation of CVT, which will depend on the localisation, extension, and rapidness of onset, as well as on the effectiveness of collateral circulation.6,7 Thus, extensive involvement, which especially affects the deep venous system, is associated with higher risk of a poor progression, whereas focal involvement of the superficial system may lead to paucisymptomatic forms.8
The low incidence of this disease also makes it difficult to perform epidemiological studies and largely hinders the performance of randomised clinical trials that might clarify current uncertainties associated with such important aspects as therapeutic management.9 Therefore, more information is still needed on the reality of this entity in each territory.
The main aim of the MOTIVATE study (abbreviation for the project’s Spanish name “management of cerebral venous thrombosis in Spain”) is to perform a descriptive analysis of the clinical characteristics of patients with CVT in different Spanish centres, and to reveal the most important aspects of its diagnosis and treatment in the Spanish setting. As secondary objective, we aimed to identify the most relevant prognostic factors in our series.
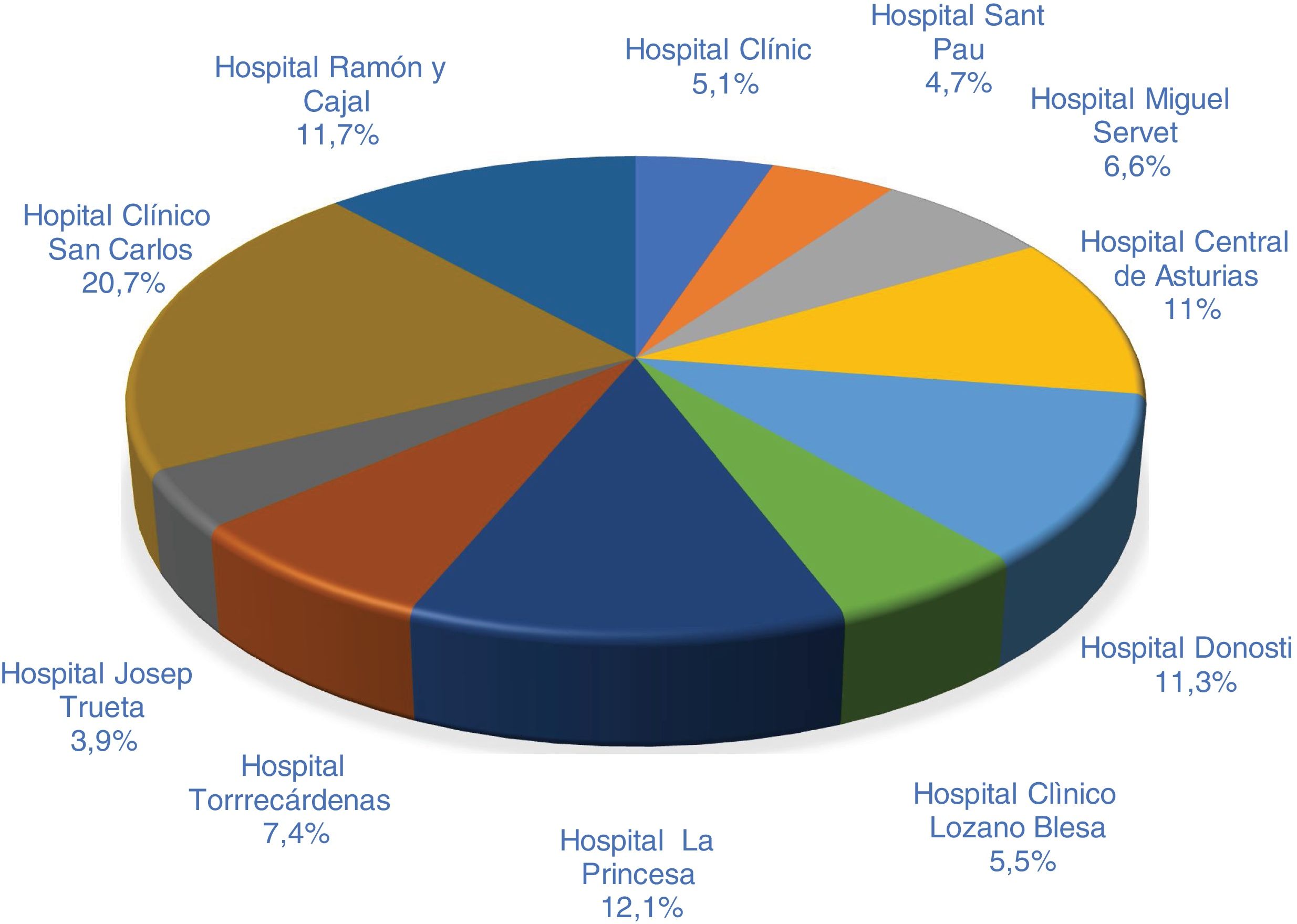
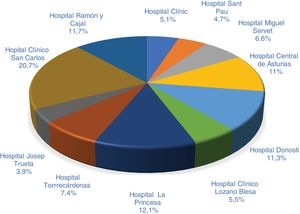
MethodsWe performed a retrospective, descriptive, multicentre study in Spain, including 11 centres from the following autonomous communities: Andalusia (Hospital Torrecárdenas), Aragon (Hospital Clínico Lozano Blesa and Hospital Miguel Servet), Asturias (Hospital Central de Asturias), the Basque Country (Hospital de Donostia), Catalonia (Hospital de la Santa Creu i Sant Pau, Hospital Clínic Barcelona, and Hospital Dr. Josep Trueta), and the region of Madrid (Hospital Clínico San Carlos, Hospital de La Princesa, and Hospital Ramón y Cajal).
Study populationWe selected patients hospitalised due to CVT at the participating centres over a period of 10 years (2008–2017). We included those patients who were diagnosed with CVT during hospitalisation, and excluded those patients with incidental CVT and paediatric patients (age under 14 years).
Cases were identified using the International Classification of Diseases, 9th revision (ICD-9). Data were prospectively collected from each centre’s electronic clinical records, and variables were grouped in a previously anonymised database for analysis. The study was approved by the clinical research ethics committee of the region of Aragon (report 07/2019).
Study variablesWe gathered baseline data on personal history, previous treatment, form of presentation, time since symptom onset, time from the request for medical assessment to diagnosis, systemic and neurological complications, intensive care unit (ICU) admission, in-hospital and 3-month mortality, cause of death, and modified Rankin Scale (mRS) score at 3 months.
We analysed the following neuroimaging data: location of the thrombosis, presence of oedema, venous infarction, and direct signs of venous thrombosis, obtained with the different techniques used in each case.
We included the following treatment variables: type of antithrombotic therapy, duration of treatment, time from symptom onset to treatment onset, endovascular therapy, or need for surgical treatment.
Statistical analysisStatistical analysis was conducted using the SPSS statistics software (version 23.0 for Windows). Normally distributed quantitative variables are expressed as means and standard deviation, and were compared using the t-test for unpaired samples. Non–normally distributed variables are expressed as medians and quartiles 1 and 3 and were compared with the Mann-Whitney U test. Dichotomous variables are expressed as percentages and were compared with chi-square test or the Fisher exact test. The threshold for statistical significance was set at a bilateral P-value < .05.
ResultsWe included a total of 256 patients. Fig. 1 shows the distribution of data from the different centres.
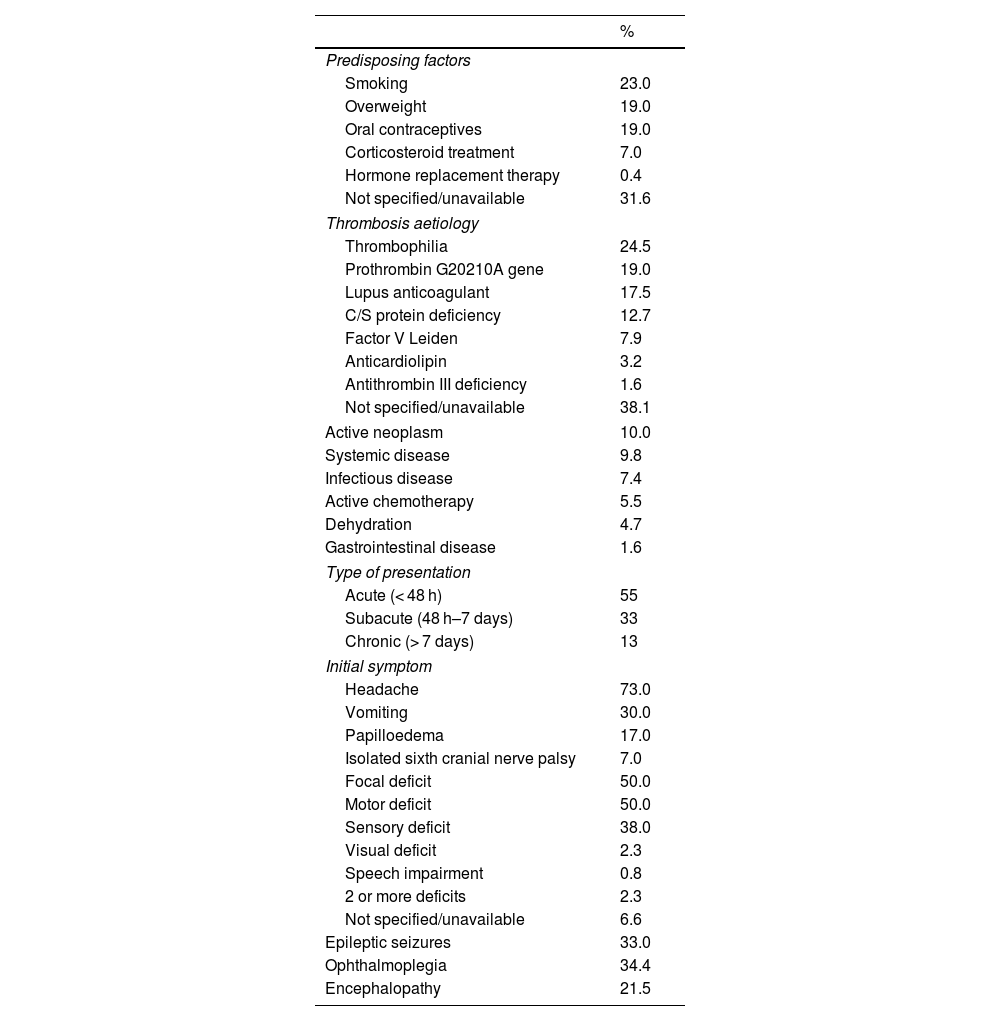
Baseline characteristicsThe mean age in our sample was 49.8 (18.7) years (range, 16–89): 45.8 for women and 53.9 for men. Women accounted for 51% of the sample. Risk factors and conditions predisposing to CVT are listed in Table 1. The most prevalent were smoking (22.7%), overweight, and use of OC.
Clinical variables of the study population.
| % | |
|---|---|
| Predisposing factors | |
| Smoking | 23.0 |
| Overweight | 19.0 |
| Oral contraceptives | 19.0 |
| Corticosteroid treatment | 7.0 |
| Hormone replacement therapy | 0.4 |
| Not specified/unavailable | 31.6 |
| Thrombosis aetiology | |
| Thrombophilia | 24.5 |
| Prothrombin G20210A gene | 19.0 |
| Lupus anticoagulant | 17.5 |
| C/S protein deficiency | 12.7 |
| Factor V Leiden | 7.9 |
| Anticardiolipin | 3.2 |
| Antithrombin III deficiency | 1.6 |
| Not specified/unavailable | 38.1 |
| Active neoplasm | 10.0 |
| Systemic disease | 9.8 |
| Infectious disease | 7.4 |
| Active chemotherapy | 5.5 |
| Dehydration | 4.7 |
| Gastrointestinal disease | 1.6 |
| Type of presentation | |
| Acute (< 48 h) | 55 |
| Subacute (48 h–7 days) | 33 |
| Chronic (> 7 days) | 13 |
| Initial symptom | |
| Headache | 73.0 |
| Vomiting | 30.0 |
| Papilloedema | 17.0 |
| Isolated sixth cranial nerve palsy | 7.0 |
| Focal deficit | 50.0 |
| Motor deficit | 50.0 |
| Sensory deficit | 38.0 |
| Visual deficit | 2.3 |
| Speech impairment | 0.8 |
| 2 or more deficits | 2.3 |
| Not specified/unavailable | 6.6 |
| Epileptic seizures | 33.0 |
| Ophthalmoplegia | 34.4 |
| Encephalopathy | 21.5 |
Presentation was mainly acute (< 48 hours), in 55% of patients. The most frequent symptom at onset was headache, in 186 patients (73%), followed by focal motor deficits in 129 patients (50%), and seizures in 33%. Regarding the time from symptom onset to the request for medical attention by the patient, 33% of patients requested attention in the first 24 hours from symptom onset, 31% within the first week, and 36% after one week of progression. These data are listed in Table 1.
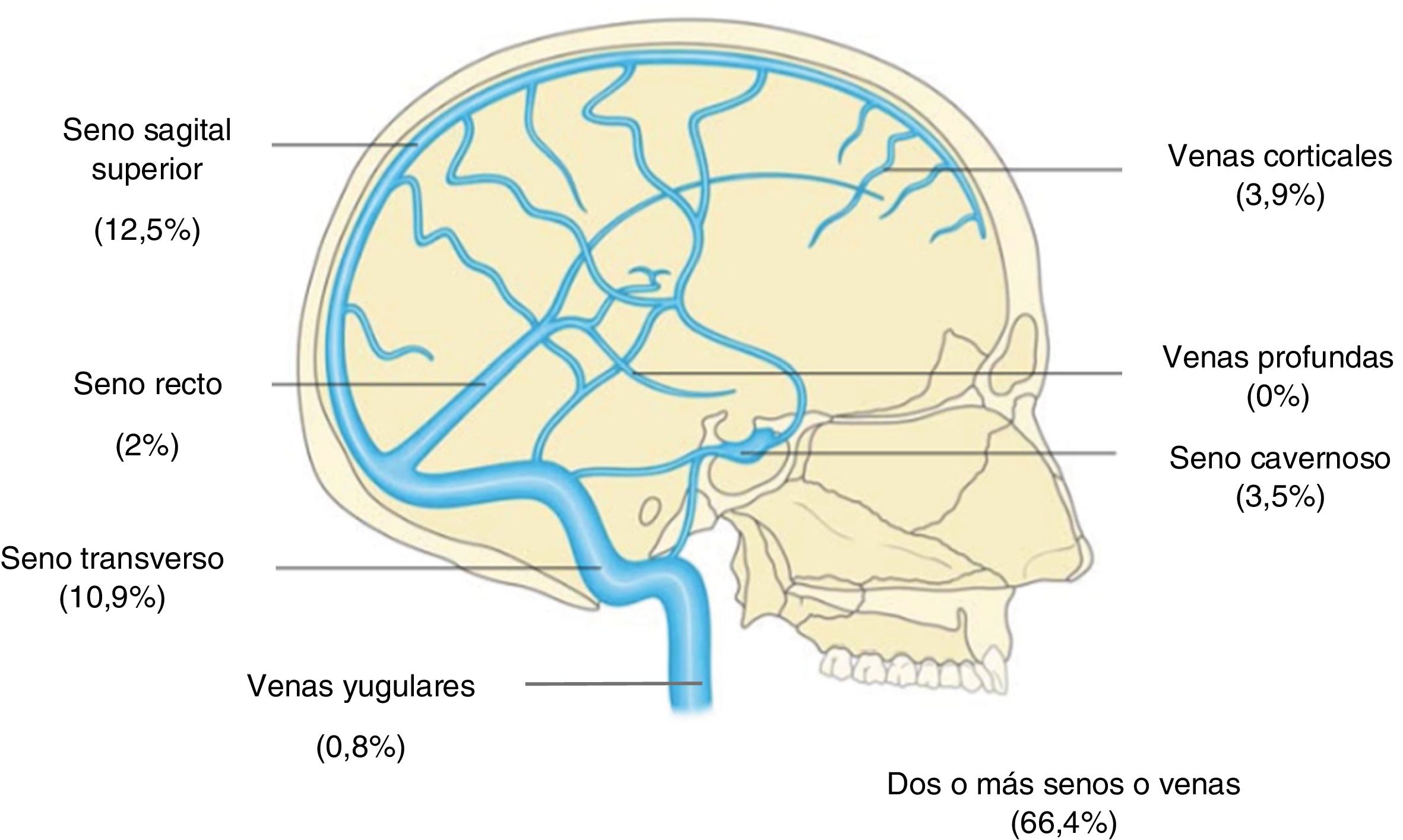
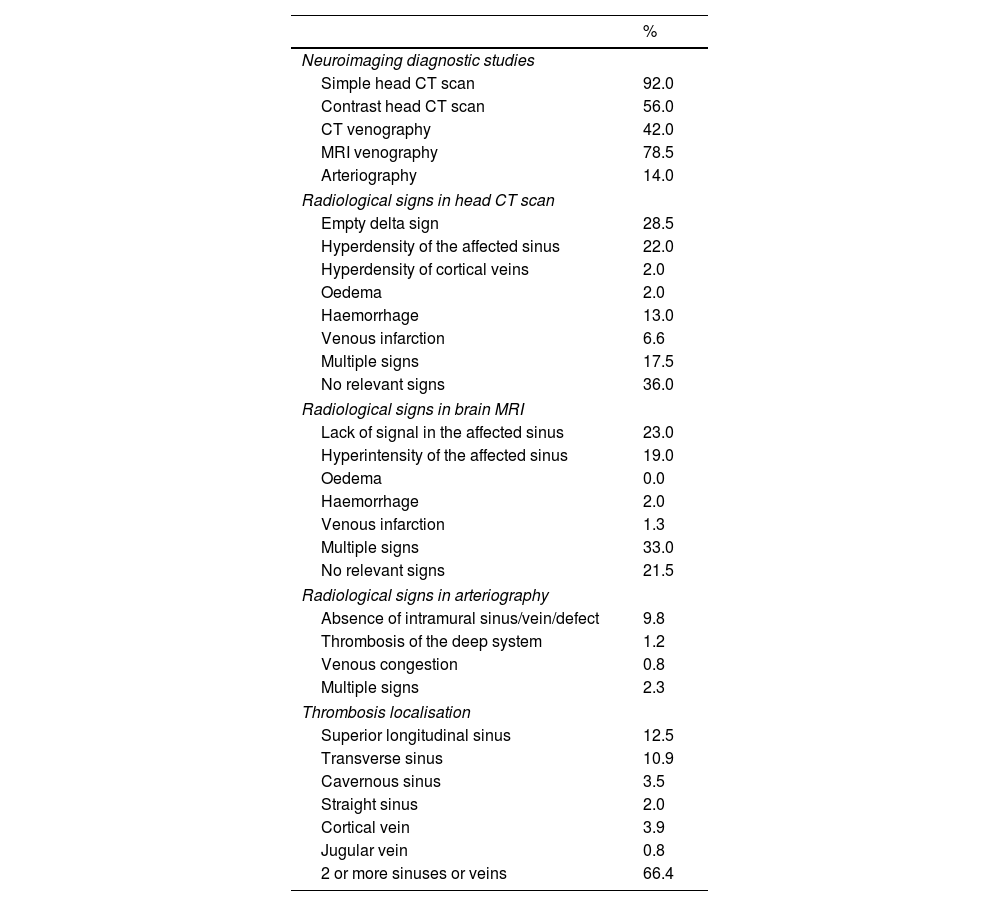
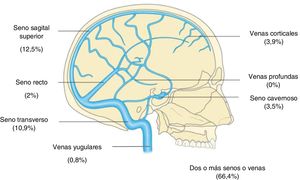
Neuroimaging diagnosis of CVTRegarding diagnostic tests, 236 patients (92%) underwent a simple CT scan. CT scans and MRI studies with venography were performed in 107 (42%) and 201 (78.5%) of cases, respectively. Only 36 patients (14%) underwent arteriography. Radiological signs indicative of CVT were identified in 60% of CT scans and 43% of MRI studies. Table 2 shows a summary of the data from radiological diagnostic studies. Regarding anatomical location, we identified involvement of 2 or more sinuses or veins in 66.4% of patients, with the superior longitudinal sinus (SLS, 12.5%) and the transverse sinus (TS, 11%) being the most frequently affected (Fig. 2).
Diagnostic variables in the study population.
| % | |
|---|---|
| Neuroimaging diagnostic studies | |
| Simple head CT scan | 92.0 |
| Contrast head CT scan | 56.0 |
| CT venography | 42.0 |
| MRI venography | 78.5 |
| Arteriography | 14.0 |
| Radiological signs in head CT scan | |
| Empty delta sign | 28.5 |
| Hyperdensity of the affected sinus | 22.0 |
| Hyperdensity of cortical veins | 2.0 |
| Oedema | 2.0 |
| Haemorrhage | 13.0 |
| Venous infarction | 6.6 |
| Multiple signs | 17.5 |
| No relevant signs | 36.0 |
| Radiological signs in brain MRI | |
| Lack of signal in the affected sinus | 23.0 |
| Hyperintensity of the affected sinus | 19.0 |
| Oedema | 0.0 |
| Haemorrhage | 2.0 |
| Venous infarction | 1.3 |
| Multiple signs | 33.0 |
| No relevant signs | 21.5 |
| Radiological signs in arteriography | |
| Absence of intramural sinus/vein/defect | 9.8 |
| Thrombosis of the deep system | 1.2 |
| Venous congestion | 0.8 |
| Multiple signs | 2.3 |
| Thrombosis localisation | |
| Superior longitudinal sinus | 12.5 |
| Transverse sinus | 10.9 |
| Cavernous sinus | 3.5 |
| Straight sinus | 2.0 |
| Cortical vein | 3.9 |
| Jugular vein | 0.8 |
| 2 or more sinuses or veins | 66.4 |
Patients were initially admitted to the neurology ward in 39% of cases, and to stroke units in 37%; 8.6% were directly admitted to the ICU. The most frequent medical complications were seizures (38.7%), which in 4.7% of cases progressed to status epilepticus, and infection (15.7%). Seventeen percent of patients were admitted to the ICU, with 35 (79.5%) requiring orotracheal intubation.
Treatment of cerebral venous thrombosisRegarding treatment of thrombosis, 235 patients (92%) received anticoagulation treatment. Antithrombotic therapy consisted of dicoumarol anticoagulants in 21% of patients, low-molecular weight heparin (LMWH) in 34%, and unfractionated heparin (UFH) in 26%. Three patients received antiplatelet treatment, and 23 received a combination of the different therapies. The duration of anticoagulation therapy varied: 3 to 6 months in 23% of cases, 1 year in 21%, and undetermined duration in 22.6%, due to the presence of a chronic thrombogenic disease. Of the total sample, 13 patients (5%) received endovascular treatment due to clinical worsening and/or progression of thrombosis: pharmacological thrombolysis in 2 cases (0.8%), mechanical and pharmacological thrombectomy in 4 (1.6%), and isolated mechanical thrombectomy in 7 (2.6%). Neurosurgical procedures were performed in 84 cases (33%), with evacuation of haematomas being the most frequent (70 cases [27.5%]), followed by decompressive craniectomy in 9 (3.5%) patients, and intracranial pressure monitoring in 4 (1.5%).
Aetiology and long-term progressionRegarding the aetiology of the episodes, coagulation alteration was the most frequent, in 63 patients (24.5%), followed by active neoplasms in 26 (10%), and systemic diseases in a similar percentage (Table 1). In terms of prognosis, 177 patients (75%) achieved functional independence (mRS score ≤ 2) at 3 months. Eleven patients died during hospitalisation, the majority due to neurological causes (82%), with 15 deaths during the first 3 months (6.3%). Twenty patients were lost to follow-up at 3 months.
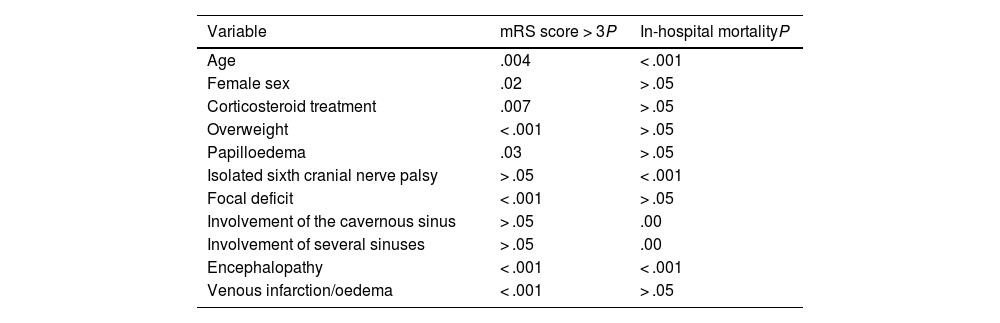
Analysis of prognostic factorsRegarding the baseline characteristics, we found a statistically significant association between functional dependence at 3 months (mRS score at 3 months > 3) and the following variables: older age (P = .004), female sex (P = .02), overweight (P = .001), and previous treatment with corticosteroids (P = .007). With respect to the form of clinical and radiological presentation, we observed a statistically significant association between higher mRS score at 3 months and the presence of intracranial hypertension with papilloedema (P = .03), focal deficits (P = .001), encephalopathy (P = .001), and venous infarction/brain oedema (P = .001). Likewise, we identified a statistically significant association between in-hospital mortality and the following variables: older age, sixth cranial nerve palsy, presentation with encephalopathy, and radiological involvement of the cavernous sinus or several venous sinuses (P = .001). These data are included in Table 3.
Main prognostic factors and those associated with mortality in the study population.
| Variable | mRS score > 3P | In-hospital mortalityP |
|---|---|---|
| Age | .004 | < .001 |
| Female sex | .02 | > .05 |
| Corticosteroid treatment | .007 | > .05 |
| Overweight | < .001 | > .05 |
| Papilloedema | .03 | > .05 |
| Isolated sixth cranial nerve palsy | > .05 | < .001 |
| Focal deficit | < .001 | > .05 |
| Involvement of the cavernous sinus | > .05 | .00 |
| Involvement of several sinuses | > .05 | .00 |
| Encephalopathy | < .001 | < .001 |
| Venous infarction/oedema | < .001 | > .05 |
mRS: modified Rankin Scale.
CVT is very probably the least understood cerebrovascular disease. This is largely due to its low prevalence, as a result of which the available data are limited, and are mainly based on small studies from single centres or individual countries. To date, our study presents the largest patient sample from Spain; among previous studies, we may highlight the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT),10 a prospective observational study that included 624 patients from 21 countries and 89 centres, providing highly valuable epidemiological information and establishing differences between the different populations studied. These differences are aetiologically significant with regard to countries of lower socioeconomic levels, according to the observations of other authors.11,12
The first noteworthy finding from our study is the similar percentage of men and women affected by this condition, contrasting with the findings described to date, which show a clear predominance of female patients, especially at younger ages. According to Lanksta et al.,13 the risk of CVT is 3.7 times greater in women aged 15 to 24 years than in those aged between 25 and 34 years. This percentage is supported by other studies that have identified a greater risk in young women.14 Therefore, a possible explanation for our findings may be the mean age of our sample, which was close to 50 years, long after childbearing age, which is associated with conditions predisposing to CVT.15–17
In our study population, the most frequently detected risk factors were smoking, overweight, and the use of OC. The risk factors described in the literature have gradually changed in recent years. Previously, infectious causes were more frequent, whereas thrombophilia, neoplasms, and the use of OC are more frequently described today.18,19 Furthermore, risk increases proportionally in these patients in the event of overweight and obesity.20 Smoking, which was not assessed in the ISCVT, is very significant in our study, with almost 25% of patients being smokers.
The most frequent forms of presentation were acute (55%) and subacute (32%). These data are similar to those of the VENOST study, which included 1144 patients from Turkey.21 From a pathophysiological perspective, this type of presentation, which is disguised in some cases, may be attributed to the progressive growth of the thrombus, enabling collateral circulation. Regarding the clinical picture, headache was the most frequent symptom at onset, with focal symptoms presenting in a slightly higher percentage than in other studies.21 Epileptic seizures (33%) and encephalopathy (55 patients [21.5%]) were also frequent, though at slightly lower rates than those reported in the ISCVT (40% and 36% respectively).10 Mental symptoms as the form of presentation are usually more frequent in older patients, with headache being the least frequently reported in this age group.22
The prognostic value of the anatomical location of CVT is well-known, as symptom severity depends on the affected vessel and progression time.7 In our series, the SLS was the structure most frequently affected in isolation, followed by the TS; the majority of patients presented multiple involvement. Whereas rates of involvement of the SLS and TS were similar to those described in the literature, the involvement of multiple sinuses was less frequent.23 The anatomical preference for the SLS may be explained by the turbulent blood flow resulting from the drainage of superficial cortical veins, which would be intensified in the lower part by the presence of fibrous walls.24
Regarding the neuroimaging diagnosis of this condition, both CT and MRI are able to detect the direct and indirect signs of CVT. Simple non-contrast CT scans are usually the initial examination performed in patients with suspected CVT, although in up to 25% to 30% of cases it does not yield relevant findings.25 In our series, the great majority of patients initially underwent a simple CT scan, and somewhat more than half were administered a contrast agent (56%). MRI was performed in 78.5% of cases, probably due to suspicion after a simple or contrast CT scan, to confirm diagnosis or to better characterise CVT and its complications, in line with the results of other authors.26 Among the radiological findings, the most common was the empty delta sign, detected in almost one-third of patients, followed by hypodensity of the venous sinus; for both findings, the prevalence observed was similar to that reported in the literature (30%).27 However, CT detected no specific sign in more than one-third of patients in our study, with findings classified as normal, similarly to the results of other authors ( 25%–30% )25,26; this percentage decreased when brain MRI studies were performed.28 In our series, venous infarction was detected in only 6.6% of patients with CT, and in 3 cases with MRI; however, haemorrhagic lesions were detected in 33 patients with CT.
A noteworthy finding in our series is the high number of cases with a delayed diagnosis, due to both the lack of perception of severity and the lack of initial diagnostic suspicion. Thus, only a third of patients consulted a physician during the first 2 hours, and almost half were diagnosed beyond the first 24 hours. These data illustrate the diagnostic challenge of this condition, and the risk of underdiagnosis.29,30 In this line, determination of D-dimer level before neuroimaging in patients with suspected CVT may be useful, except in those with isolated headache or with long symptom progression times (> 1 week), which are associated with false negatives.30,31
With regard to treatment, the guidelines recommend early anticoagulant therapy; however, there is no consensus regarding the type and duration of antithrombotic therapy. In our series, 34% of patients received LMWH at therapeutic doses, and 26% received UFH. Once the acute phase is resolved, oral anticoagulants are indicated in the absence of any contraindication.32 In our series, it is striking that only 21% of patients were subsequently treated with dicoumarol anticoagulants, assuming that the remaining patients continued receiving other antithrombotic therapies. In terms of treatment duration, a 3-month period is considered sufficient if CVT is associated with a transient risk factor; in other circumstances, with greater risk of recurrence, the duration of anticoagulation may be 6 to 12 months, or even indefinite.33 In our study, indefinite treatment durations were indicated in 23% of patients due to thrombophilic alterations; in similar percentages of patients, treatment was maintained for 3–6 to 12 months.
There is controversy regarding cases of CVT with venous infarction and a haemorrhagic component, which may be exacerbated by anticoagulant treatment. Few studies have been performed that clarify this question, although a meta-analysis of 2 small randomised studies observed a 13% absolute reduction in mortality, without an increase in the appearance of new haemorrhagic lesions; these results were not statistically significant.34 Despite this, the conclusions were similar to the results observed in clinical practice: an improvement associated with heparin treatment. In the prospective cohort of the ISCVT,10 with previous intracranial bleeding in almost 40% of cases, 83% of patients received heparin without poorer prognosis.
Currently, the role of endovascular treatment in CVT is poorly defined. In our study, only 13 patients received endovascular treatment. The main reasons that may explain its limited use are the inherent risk of this treatment, and the doubts regarding criteria for indication, which have been growing since the publication of a clinical trial that did not find a benefit. Therefore, such techniques are reserved for cases of neurological impairment with poor prognosis under medical treatment.35 This lack of a benefit, contrary to the findings reported in the context of arterial ischaemia, may be due to the technical difficulty of achieving persistent venous recanalisation, especially in the superficial system.
In our study, overall mortality and the rate of disability at 3 months were lower than those described by other authors.10 The prognosis of CVT has improved over the last decades due to 2 factors: a decrease in infectious pathology and an increase in the diagnostic accuracy of current neuroimaging techniques, enabling earlier diagnosis and treatment. However, special emphasis has been placed on subtle sequelae. Some studies have reported that up to one-third of patients with CVT did not return to work, especially among women and patients with parenchymal lesions.
Regarding factors associated with mortality, we observed a statistically significant association with older age, ophthalmoparesis, and encephalopathy, as well as involvement of the cavernous sinus and of multiple sinuses simultaneously. Factors associated with poorer prognosis (mRS score > 3 at 3 months) were again age, variables associated with increased intracranial pressure, and venous infarction. In a German multicentre study performed in neurocritical care units, such factors as clinical impairment at admission, midline shift, and age predicted poorer prognosis.36 In this line, clinical scales of CVT severity have been published to predict prognosis, such as that designed by Barboza et al.,37 which showed an accuracy of almost 92% in predicting mortality at 30 days and 85% for predicting mRS scores > 2.
Our study presents some relevant limitations. The first is its retrospective character, which entails a significant risk of losing data due to the inability to obtain all variables in all cases. The second would be the lack of centralised assessment of neuroimaging studies, which makes it difficult to obtain information of greater quality and interest. Another limitation is the participation of centres of different levels of care; although this enables a broader perspective of the management of this disease in the Spanish setting, it also increases the heterogeneity of the treated cases.
The MOTIVATE study is the largest multicentre study performed in Spain, with the participation of hospitals from all corners of the country. It includes a large patient sample, despite the low incidence of this condition, and provides relatively recent data for a prolonged period of time. We therefore believe that the study provides an approximate and representative image of the actual situation of CVT in Spain in recent years.
ConclusionsThe management of CVT in Spain presents significant variability from the diagnostic and therapeutic perspectives, as well as delays in seeking medical care, on the part of patients, and in diagnosis, by physicians. Our results identify favourable prognostic data but considerable areas for improvement, and suggest the need for greater homogeneity in the management of this severe but treatable condition. Prognostic markers enabling identification of patients at higher risk should be better defined in a national, multicentre prospective registry of CVT, with a view to improving the management of this condition based on experience obtained in real clinical practice.
FundingThis study has not received financing from any sources.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the participating centres for their collaboration in this study.