Leprosy remains a major health problem in developing countries.1,2Mycobacterium leprae is the causative agent, and although it has been isolated in every part of the body except the central nervous system, it most commonly infects the peripheral nerves and skin. Peripheral neuropathy is elicited by the infection or by accompanying immunological events. It may be long-lasting and give rise to important residual symptoms on occasions.3 In some patients, neural involvement is the predominant or sole symptom.4 We present a case of imported leprosy that initially manifested with significant neural involvement and skin lesions of atypical location. Sural nerve biopsy was necessary to assign the diagnosis.
Our patient was a 19-year-old man from Mauritania who had emigrated to Spain 4 years previously. He came to our clinic due to a 2-year history of progressive sensory symptoms, mostly distal, in all 4 limbs and motor deficit in upper limbs. Neurological examination showed asymmetrical weakness in the upper limbs, predominantly in the region of the left ulnar nerve, together with amyotrophy of the hand (ulnar claw) (Fig. 1). Weakness of the lower limbs was predominantly distal, with mild impairment of toe walking. We found generalised hypereflexia with areflexia in the left upper limb. We also observed decreased tactile sensitivity in both hands and a burn injury on the left hand. No nerve hypertrophy was observed. Skin examination revealed no lesions on the face or limbs, but we did find 2 hypopigmented lesions with preserved sensitivity on the patient's back.
An electromyographic and electroneurographic study showed an axonal demyelinating sensorimotor neuropathy in several nerves of all 4 limbs compatible with moderate to severe mononeuropathy multiplex. The affected area was asymmetrically distributed, with the left arm being the most impaired.
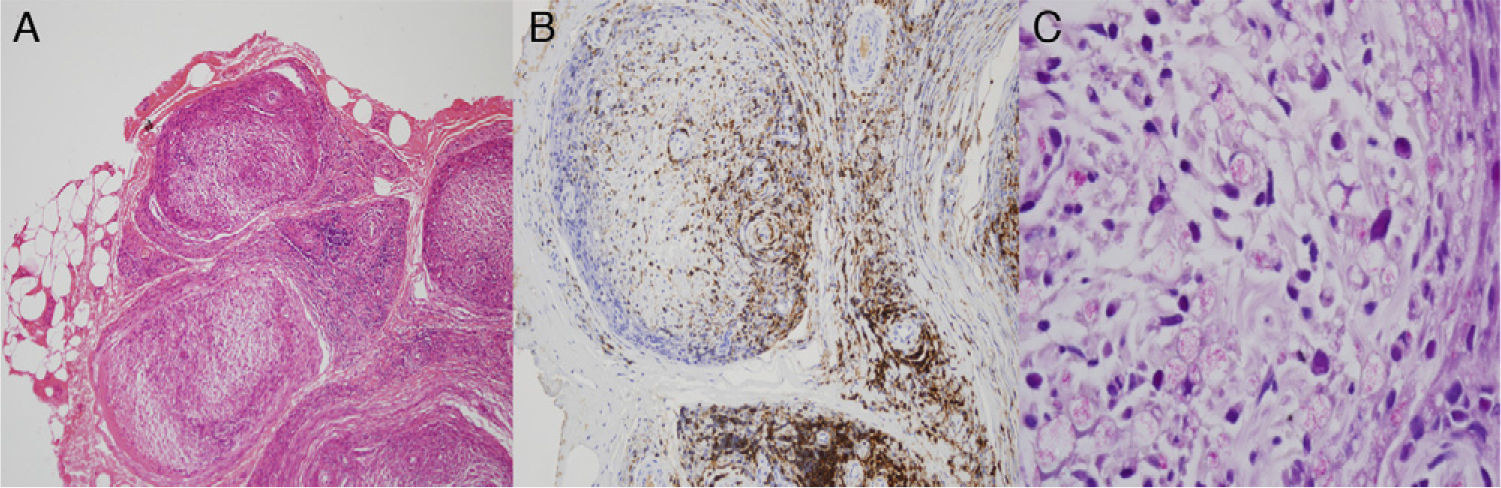
Examination of the sural nerve biopsy revealed damage to nerve fascicle structure due to a significant inflammatory infiltration of T and B cells (CD45, CD3 and CD20) into the epineurium, perineurium, and endoneurium. We found numerous vacuolated cells presenting punctiform structures partially revealed by the Ziehl-Neelsen stain technique and more clearly using the Fite-Faraco technique (Fig. 2). An overall loss of myelinated nerve fibres was also observed.
Based on these findings, the patient was diagnosed with leprosy and started treatment with rifampicin, clofazimine, and dapsone, according to recommendations by the World Health Organization (WHO) for multibacillary leprosy.5 The patient's condition improved with no reactions during treatment and a significant improvement in both motor and sensory deficit except in the left ulnar nerve.
The cardinal signs pointing to a diagnosis of leprosy are hypopigmented, anaesthetic skin lesions usually located on colder areas of the body (limbs and face), thickened nerves and Fite-Faraco stain revealing alcohol-fast bacilli in a skin biopsy, skin smear, or nerve biopsy specimen.6
According to WHO criteria,7 leprosy is classified as either paucibacillary or multibacillary according to the number of lesions and findings from the biopsy. The Ridley-Jopling classification, based on the host's immune response, classifies leprosy cases as tuberculoid or lepromatous, with different intermediate forms also appearing.8 Following both of these classifications, we can state that our patient presented multibacillary and indeterminate leprosy.
Nerve involvement is frequent in long-standing leprosy, whether the case manifests as mononeuritis multiplex or as predominantly distal polyneuropathy. Ulnar nerve involvement, as observed in our case, is especially frequent and incapacitating.2,4–6,9 Pure neural leprosy has classically been associated with tuberculoid manifestation of the disease, or with an incipient indeterminate stage according to the Ridley-Jopling classification.8 However, as in this case, multibacillary leprosy can cause symptoms in which neurological manifestations predominate over atypical and unremarkable skin symptoms.10
Neurophysiological studies initially show demyelination that can later be masked by the axonal lesion arising in advanced stages of the disease.2,4,11 In cases of atypical manifestation or when nerve involvement is very pronounced, a sural nerve biopsy may be necessary to deliver a diagnosis. A major inflammatory reaction with destruction of nerve fibres and presence of macrophages with bacilli is typical, as we observed in our case.12
Leprosy is the most common treatable cause of neuropathy in the world.13 Its prognosis depends mainly on the patient's immune response and on the interval between symptom onset and treatment.5 Leprosy is not a frequent disease in our setting and imported cases have specific characteristics. These cases usually affect young males who contract the disease in their home countries where leprosy is endemic (the Saharan region of Africa in our case).14 Early diagnosis can lead to the implementation of an appropriate diagnosis which prevents disease progression and improves the patient's functional state.
Please cite this article as: Pedraza Hueso MI, Hinojosa Mena-Bernal C, Hernández-Laín A, Guerrero Peral AL. Mononeuropatía múltiple por lepra: descripción de un caso con presentación atípica. Neurología. 2014;29:313–314.
Part of this study was presented in poster format at the 63rd annual meeting of the Spanish Society of Neurology, Barcelona, November 2011.