Lumbar puncture (LP) is a technique often used for diagnostic purposes and less frequently for therapeutic ends.1,2 The main complications of the procedure are post-lumbar puncture headache (PPH) and transient nerve root irritation.3,4 Other less prevalent complications include cranial neuropathy, infections, brain herniation, vasovagal syncope, cardiac arrest, haemorrhage, and cerebral venous thrombosis (CVT).1,5 The last complication is exceptional, but it has been described after epidural anaesthesia, myelography, and diagnostic lumbar puncture.3,5,6
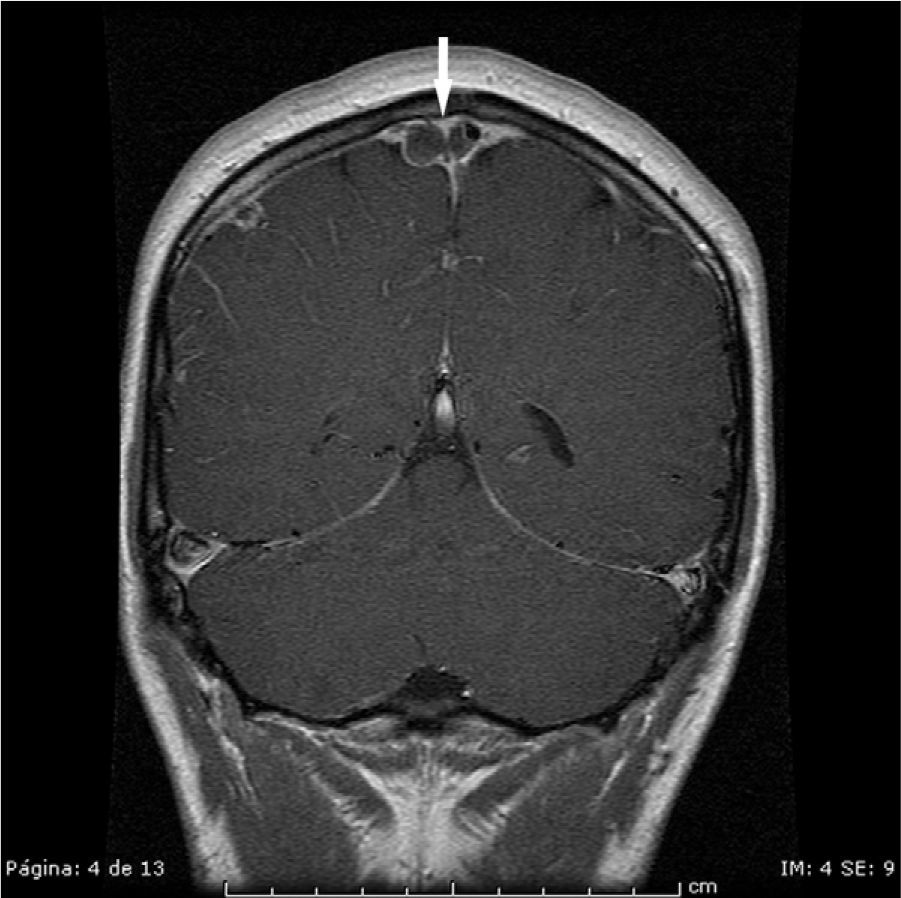
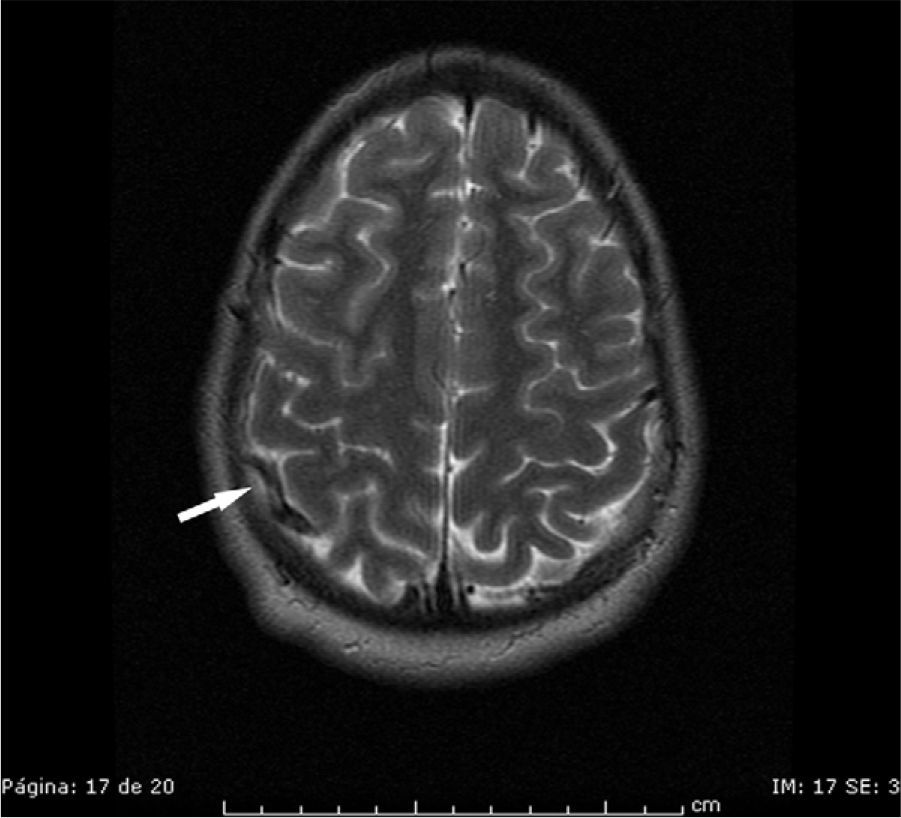
We present the case of a 20-year-old man with no known vascular risk factors, 2 prior episodes of retrobulbar optic neuritis over the 3 preceding years, and normal neuroimaging results. He was admitted for a subacute case of paraesthesia from the lower limbs to the waist. The examination found global hyperreflexia, bilateral ankle clonus, and hypoaesthesia at D10. MRI revealed multiple demyelinating lesions in the brain and another in the spinal cord at D8 with no contrast uptake. LP was performed (procedure was non-traumatic) to complete a biochemical and cytological study of CSF and oligoclonal bands due to suspected multiple sclerosis (MS). The patient was then started on IV methylprednisolone (1g bolus). Forty-eight hours later, the patient reported headache on standing up; by 5 days, the headache was more intense and did not improve on lying down. Neurological examination showed no focal signs, papilloedema, or new focal signs. Cranial MRI showed partial venous thrombosis of the superior sagittal sinus, with bilateral meningeal venous stasis and acute linear parietal ischaemic infarcts (Figs. 1 and 2). In light of these findings, doctors began treatment with therapeutic doses of low molecular-weight heparin. This was subsequently changed to oral acenocoumarol, with which the patient has been treated for the past 6 months. Progress has been satisfactory from a clinical and radiological standpoint; headache resolved a few days after the patient was admitted and the one-month MRI scan found that sinus patency had been restored. The coagulation test revealed a heterozygous prothrombin G20210A mutation. The test for oligoclonal bands in CSF delivered positive results.
Some studies suggest that the mechanism responsible for PPH may contribute to CVT.3 Onset of PPH takes place 24 to 48hours after LP and generally resolves in a week. It typically intensifies when the patient is standing and diminishes when the patient lies down.1 The headache is caused by loss of CSF through the meningeal orifice at the puncture site when this procedure results in intracranial CSF hypotension. This gives rise to traction and dilation phenomena in cerebral veins that stimulate pain receptors near the dural sinuses, resulting in headache.3,5 As a result of this dilation process, blood flow speed decreases, and the consequent venous stasis contributes to the development of CVT.3,7,8 Although both entities (PPH and CVT) share aetiological mechanisms, the frequency of CVT is very low compared to that of PPH. This suggests that the degree of venous stasis induced by the outflow of CSF from the spine is usually insufficient to cause CVT, except in patients who are predisposed due to other reasons (congenital thrombophilia, oral contraceptives, postpartum state, migraine, etc.).3
CVT secondary to a diagnostic lumbar puncture is extremely infrequent. Most such cases have been described in patients under study for demyelinating disease, as in our case.6,9,10 Additionally, administering high doses of IV corticosteroids after an LP was determined to be the main risk factor contributing to the development of CVT in most cases, especially if other associated vascular risk factors were present.9–12 Authors have not found a causal relationship between demyelinating disease and CVT.6 In recent years, however, experts focusing on disorders in intracranial venous haemodynamics have postulated that they may be involved in the pathophysiology of MS.13,14
On the other hand, given that treatment with high-dose corticosteroids is itself a prothrombotic risk factor, Kalanie et al. suggest that it may even be appropriate to use prophylactic enoxaparin to prevent CVT in patients with MS who will be treated with high-dose IV methylprednisolone.15
Early diagnosis is difficult, as CVT symptoms overlap with those of PPH. We should suspect CVT in all patients with typical PPH that intensifies after an initial period, does not lessen with the patient in decubitus, or persists for more than a week. This is especially true in patients with demyelinating disease, vascular risk factors, or treatment with high-dose corticosteroids immediately following LP.3 De novo appearance of a bilateral papilloedema associated with PPH is consistent with a diagnosis of CVT. However, in patients with MS, history of optic neuritis with peripapillary atrophy may make interpretation of findings difficult.
For the reasons listed above, we believe it appropriate to reserve a window of time between performing LP and administering high-dose corticosteroids. We feel it is best to start IV steroids to treat the clinical flare-up and wait at least a month before performing LP.
Please cite this article as: Sillero Sánchez M, Rodriguez Fernandez N, Sánchez Vera L, Gómez González B, Asencio Marchante JJ. Trombosis venosa cerebral tras punción lumbar y tratamiento corticoideo a dosis elevada. Neurología. 2014;29:315–316.