We present the case of a 47-year-old man who worked as a baker and was admitted to hospital due a 4-day history of subacute symptoms of choreoathetosis predominantly affecting the head and left limbs, as well as motor impersistence and dysarthria. The physical, neuropsychological, and psychiatric examinations revealed no other relevant findings, including normal muscle balance and polymodal sensitivity. He had no family history of interest and a personal history of migraine, smoking, and moderate alcohol dependence (3 mixed drinks per day; his alcohol consumption habits had not changed in the past few months).
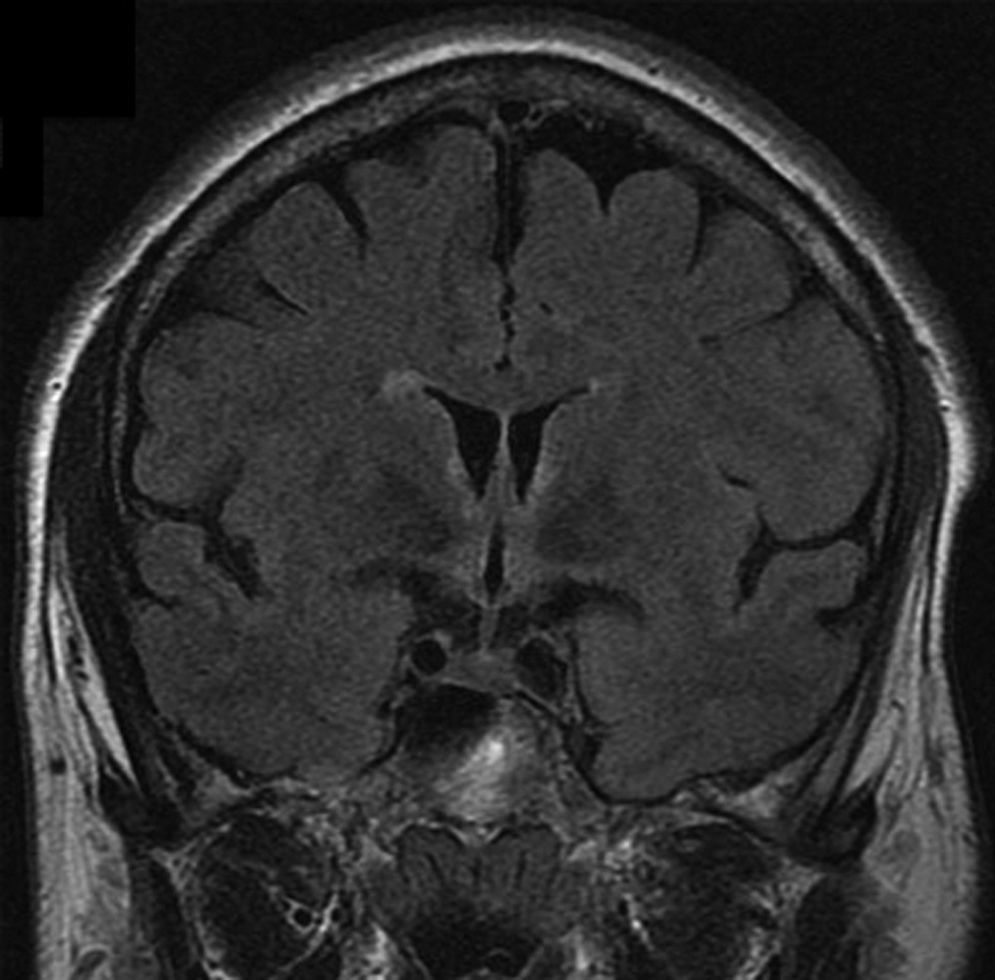
He underwent a complete blood study (electrolytes; TSH; PTH; copper; ceruloplasmin; folate; and vitamins E, B1, and B12), autoimmune tests (ANA; ENA; ANCA; TPO; lupus anticoagulants; and cardiolipin, gliadin, and intrinsic factor antibodies), serology tests, blood smear, test for antineuronal antibodies, lumbar puncture, and a urine toxicology test. The only relevant findings were macrocytosis (MCV=115fL [normal values: 80–100fL]) and vitamin B12 deficiency (148pg/mL [normal values: 200–900pg/mL]). Our patient displayed no anaemia and no other imbalances. A brain MRI scan revealed a slightly hyperintense area adjacent to the third ventricle and in the mammillary bodies, which may be related to our patient's alcohol consumption habits; no other alterations were found (Fig. 1). A CT scan of the neck, chest, abdomen, and pelvis showed no signs of hidden neoplasm.
While waiting for results from the laboratory tests, we initiated empirical treatment with IV immunoglobulins, which did not improve our patient's symptoms. We ruled out toxic, infectious, dysimmune, vascular, neoplastic, and paraneoplastic causes. Since we suspected subacute choreoathetosis due to vitamin B12 deficiency, the patient started IM vitamin B12 (1000μg/day for 7 days, followed by 1000μg/week for a month, and 1000μg/month) plus oral tiapride dosed at 50mg every 8hours; symptoms improved steadily and had resolved completely one week after treatment onset. Our patient remained asymptomatic one month later, so tiapride was discontinued. At 3 months, he continued to be asymptomatic and showed normal vitamin B12 levels.
Vitamin B12 deficiency is typically associated with such neurological disorders as subacute combined degeneration, dementia, and polyneuropathy.1 However, the literature also includes isolated cases of such extrapyramidal disorders as parkinsonism, focal dystonia, ataxia, myoclonus, or even chorea associated with vitamin B12 deficiency.1–6
From a clinical viewpoint, chorea secondary to vitamin B12 deficiency may be either unilateral or markedly asymmetrical with no associated structural lesions, as with other types of chorea (those linked to deficiencies or metabolic changes).3 Chorea linked to vitamin B12 deficiency is thought to be caused by the glutamatergic activation of the basal ganglia due to excess of homocysteine (an NMDA agonist); in addition, there may be a potential neurotoxic effect resulting from an excess of methyltetrahydrofolate (an agonist of kainic acid which induces Huntington chorea in animal models).2,7,8 Unfortunately, homocysteine levels in our patient were not tested during the acute phase. If sensory alterations are associated with vitamin B12 deficiency,3 they may contribute to choreoathetosis by a deafferentation mechanism. However, this does not seem to be a necessary condition; in our patient and in other cases, examinations revealed no sensory alterations.2,6
As in other cases in the literature, our patient's diagnosis of subacute reversible chorea caused by vitamin B12 deficiency was based on the temporal relation between symptoms and vitamin B12 deficiency, the exclusion of other potential causes of chorea, symptom resolution having coincided with stabilisation of vitamin B12 levels, and the lack of recurrence after tiapride was discontinued. Given that not all patients with low vitamin B12 levels develop neurological symptoms, other factors such as long-term alcohol abuse are likely to trigger the syndrome. MRI findings in our patient match those classically associated with Wernicke encephalopathy due to vitamin B1 deficiency9; however, our patient showed normal vitamin B1 levels.
In conclusion, chorea is a rare manifestation of vitamin B12 deficiency which can be resolved with replacement therapy. We recommend including vitamin B12 tests in the aetiological study of chorea of unknown origin.
FundingThe authors have received no funding for this study.
Conflicts of interestThe authors have received travel grants and/or consulting fees from Biogen-Idec, Sanofi-Genzyme, Teva, Novartis, Almirall, Merck-Serono, and Schering-Bayer. The authors have no conflicts of interest to declare.
Please cite this article as: Gascón-Giménez F, Coret-Ferrer F. Corea subagudo reversible por déficit de vitamina B12. Neurología. 2017;32:342–343.