Internal carotid artery (ICA) occlusion is an important cause of stroke: stroke most frequently occurs at the time of occlusion or during the following year, due to low perfusion and cerebral ischaemia or artery-to-artery embolism. In symptomatic stenosis with more than 70% of arterial lumen, selected symptomatic patients with stenosis of more than 50%, or asymptomatic patients with a more than 70% stenosis, endarterectomy or carotid stent placement has been shown to be beneficial for secondary prevention of ischaemic strokes. However, there is no recommended surgical or interventional procedure for carotid occlusion and current recommendations focus on monitoring the contralateral ICA, controlling cardiovascular risk factors, avoiding distal hypoperfusion, and awaiting the development of natural compensatory mechanisms. The possibility of spontaneous recanalisation of the occluded artery is frequently overlooked.
We report the case of a patient with ICA occlusion which was confirmed by arteriography and followed up with ultrasound. At 18 months, spontaneous recanalisation was observed, with a critical stenosis of that artery, which poses the following questions: How frequent is spontaneous recanalisation of an occluded ICA? When does it happen? How should we react? For how long should we follow up patients with occluded ICAs?
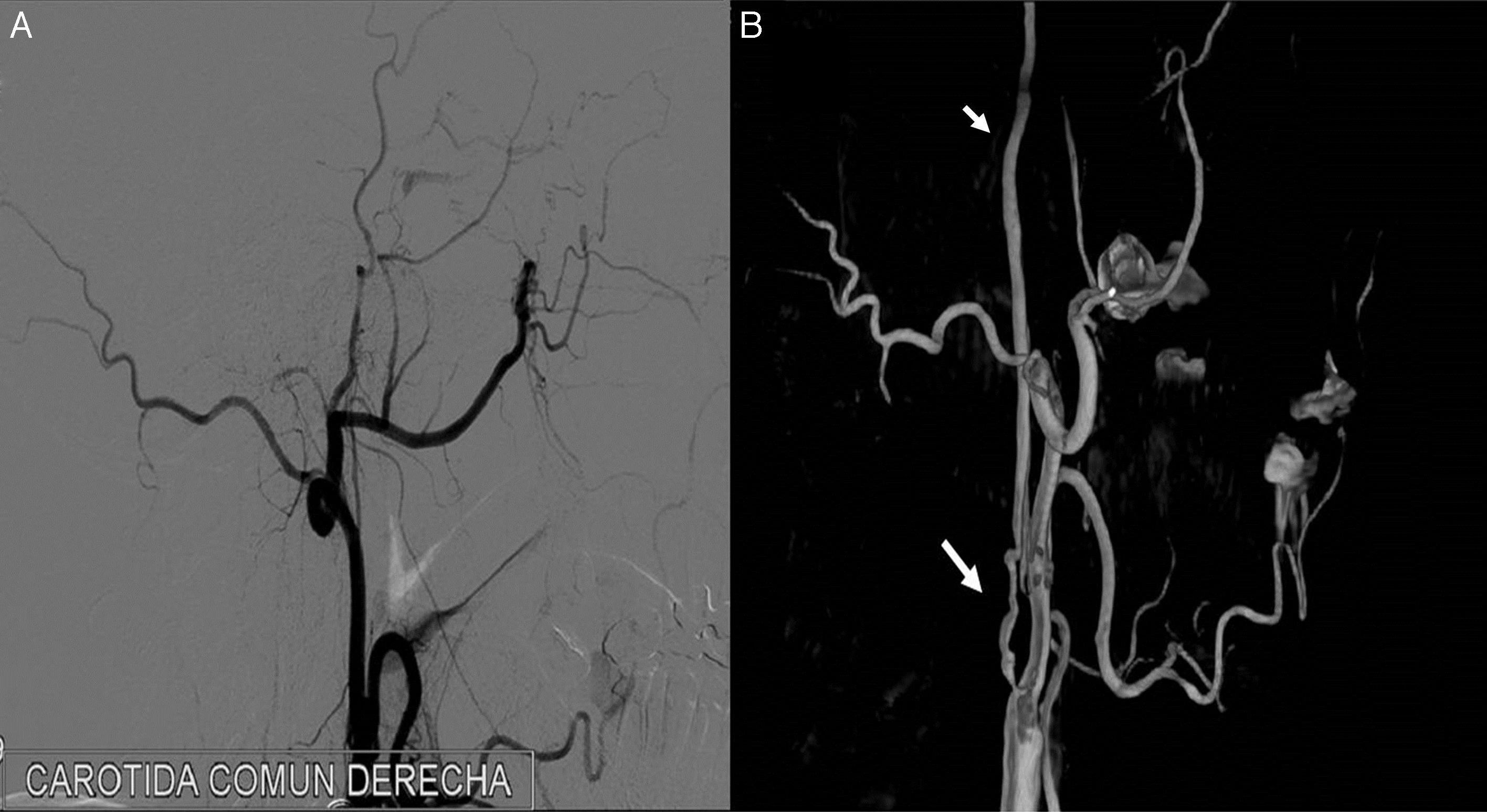
Clinical caseWe present the case of a male smoker, aged 52, with type 2 diabetes mellitus and no history of arterial hypertension. He was admitted due to left hemiparesis with faciobrachial predominance and sudden-onset ipsilateral hypoaesthesia, with no language impairment, visual field deficit, or any other associated neurological symptoms. A brain MRI showed an infarct in the right middle cerebral artery (MCA) territory. An echo-Doppler study of the supra-aortic trunks (SAT) revealed an occlusion of the right proximal ICA, a stenosis of less than 50% of the left ICA, and multiple, well-defined atherosclerotic plaques in both carotid sinuses and in the right common carotid artery. These findings were confirmed by angiography of the SATs (Fig. 1A), which revealed no radiological findings typical of fibromuscular dysplasia, vasculitis, or arterial dissection. The patient's clinical symptoms stabilised and he was discharged after 8 days of hospitalisation, receiving 300mg of acetylsalicylic acid and 80mg atorvastatin daily.
A follow-up echo-Doppler study of the SATs performed 6 months later showed the same results as those obtained during hospitalisation.
Eighteen months after his discharge, the patient visited our department due to a one-week history of dizziness without vertigo and no other associated clinical symptoms. Physical examination revealed no new findings besides the sequelae of the previous cerebral ischaemic event. Vascular risk factors were adequately controlled, although LDL cholesterol levels had decreased only to 90mg/dL. An echo-Doppler study of the SATs revealed a filiform flow in the right ICA (which was occluded in the previous studies). This was confirmed by a new angiography of the SATs, which revealed a critical stenosis secondary to an atherosclerotic plaque at this level (Fig. 1B). The right hemisphere was adequately supplied by the left ICA. Lastly, considering the compensatory flow through the collateral arteries of the circle of Willis, the absence of significant interhemispheric asymmetries in the evaluation of haemodynamic reserve, the lack of microembolism detected by the transcranial Doppler ultrasound, and the fact that the patient had remained asymptomatic for the 18 months he was receiving the prescribed treatment, it was decided, in consensus with the interventional neuroradiology and vascular surgery departments, to continue the conservative treatment and periodic follow-up with ultrasound studies.
DiscussionSpontaneous recanalisation of an occluded ICA was believed to be an infrequent phenomenon; however, the number of published cases and some case series1-4 make us believe that this phenomenon is probably more frequent than thought. It most frequently occurs shortly after the occlusion5; however, published rates of late recanalisation range from 2.3% to 11%.1,6,7
The mechanism by which an occluded ICA is recanalised is subject to debate. Acute occlusions may be recanalised by endogenous lysis, decreased endothelial oedema located at the level of the occlusion, or intraplaque haemorrhage.8 Several hypotheses have been proposed for the recanalisation of chronic occlusions, including the activation of endothelial thrombolytic mechanisms; the histological characteristics of the plaque are also believed to influence the probability of recanalisation.4
Carotid occlusions have long been described as a stable condition not requiring surgery, unlike severe, symptomatic carotid stenosis (from 70% to 99% of arterial lumen), which may be considered to involve high embolic risk and, therefore, benefit from endarterectomy or angioplasty. After spontaneous recanalisation, an occluded ICA develops severe stenosis; the therapeutic approach to be taken with these patients may change as a result of this, especially in those who have experienced an improvement in the sequelae caused by the previous stroke, and with the brain parenchyma supplied by the occluded ICA being partially preserved.
Intra-arterial angiography is the standard test of reference to observe an occlusion or differentiate it from an ICA with severe stenosis9; however, this is an invasive procedure and may be associated with a certain risk of complication. The availability of the echo-Doppler study of the SATs, and its good sensitivity and specificity to detect ICA pseudo-occlusions (94% and 100%, respectively),9,10 support the use of this technique for proper follow-up of these patients. In doubtful cases, an echo-Doppler study of the SATs together with a CT angiography or contrast-enhanced MRI angiography may avert the need to perform an angiography.11 The duration and frequency with which follow-up echo-Doppler studies of the SATs should be performed in patients with carotid occlusions are not clear.
This case is an example of the possibility of late spontaneous recanalisation of an occluded ICA. This event may be more frequent than expected. Therefore, we deem it interesting to consider following up patients with an occluded ICA through echo-Doppler studies of the SATs with the aim of promptly detecting candidates to invasive treatment due to recanalisation.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tejada Meza H, Artal Roy J, Martínez García R, Marta Moreno J. Recanalización espontánea de una oclusión crónica de arteria carótida interna. Neurología. 2018;33:66–68.