Subclavian steal syndrome refers to subclavian artery stenosis before the origin of the vertebral artery, mainly due to the appearance of atheromatous plaques, which causes a retrograde flow in the ipsilateral vertebral artery together with transient neurological symptoms secondary to ischaemia in the affected territory.1
Its prevalence ranges from 0.6% to 6.4% in the general population.2 It is more frequent in men (ratio of 2:1), with the exception of cases secondary to Takayasu arteritis, in which women are more commonly affected. The left subclavian artery is more frequently involved, with a ratio of 4:1.
We present the case of a 70-year-old man with a history of arterial hypertension controlled with calcium channel blockers, angiotensin II receptor blockers, and thiazide; and type 2 diabetes mellitus treated with oral anti-diabetic drugs. The patient was admitted to the neurology department due to symptoms of central vertigo and gait ataxia of 48hours’ progression.
The physical examination revealed marked asymmetry when arterial blood pressure (BP) was measured simultaneously in both arms. The mean BP calculated from 3 measurements was 100/70mmHg in the right arm and 148/97mmHg in the left. Heart sounds were regular and no heart or carotid murmur was heard. The radial pulse was less easily felt in the left wrist than in the right. The neurological examination revealed vertical nystagmus, gait ataxia, and moderate dysarthria. During the targeted interview, the patient reported frequent left arm pain of several months’ progression.
A head CT scan revealed no signs of acute ischaemia; a brain MRI confirmed an acute vertebrobasilar stroke. A Doppler ultrasonography of the supra-aortic trunks showed a biphasic pattern in the left subclavian artery, compatible with subclavian steal syndrome (grade 2). Examination of the basilar artery through the transforaminal window revealed inverted flow at a depth of 80mm in the left vertebral artery and reduced flow speed in both posterior cerebral arteries.
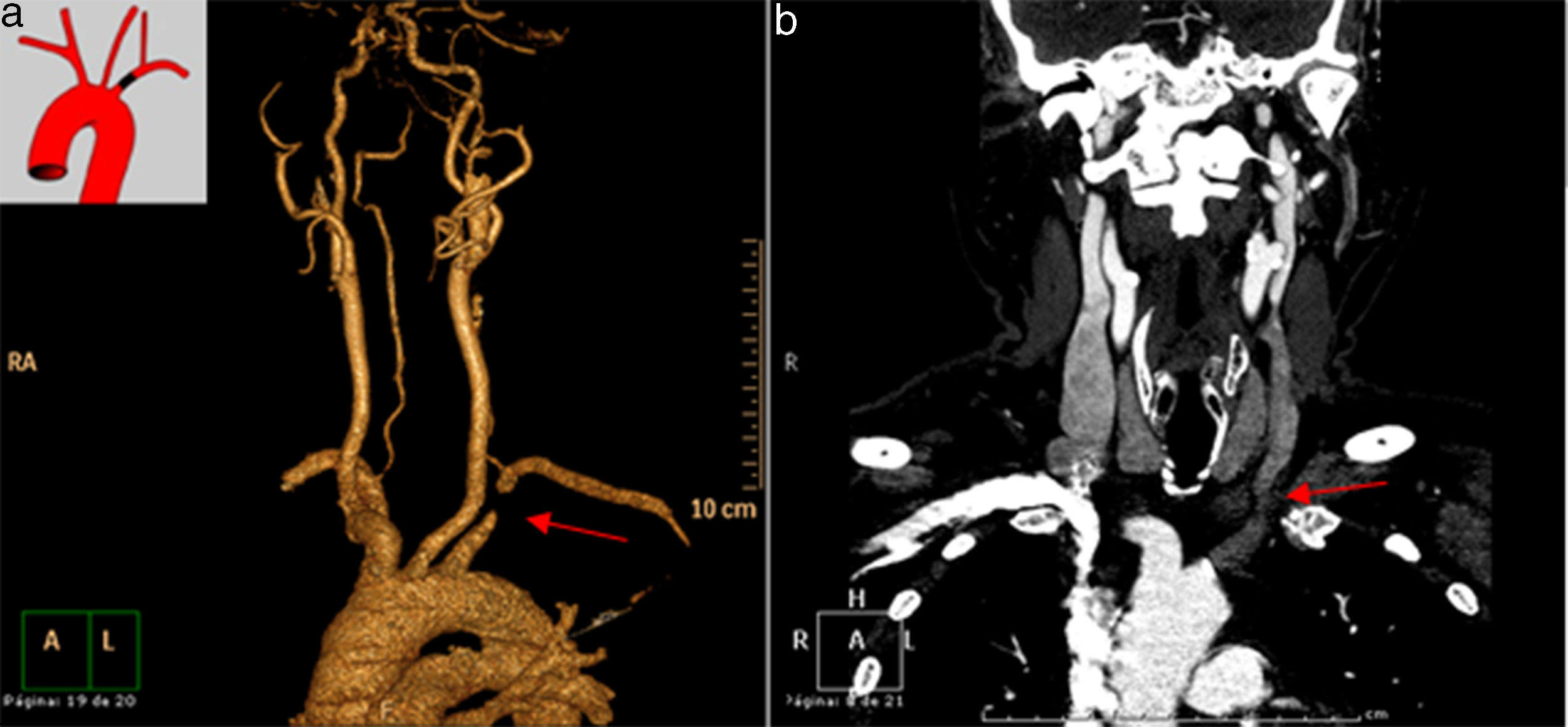
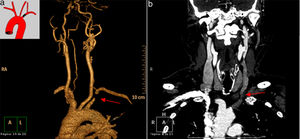
An MRI-angiography revealed severe stenosis of approximately 5mm in diameter in the left subclavian artery, proximal to the origin of the homolateral vertebral artery; images were suggestive of retrograde flow in the left vertebral artery, which was permeable in a contrast study. These findings are compatible with subclavian steal syndrome (Fig. 1).
Considering a diagnosis of acute vertebrobasilar ischaemia secondary to subclavian steal syndrome, we opted for endovascular treatment, placing a stent in the left prevertebral subclavian artery. A subsequent angiography confirmed that flow was adequate and no complications were observed. A one-month follow-up Doppler ultrasonography of the supra-aortic trunks and BP measurement in both arms revealed a significant reduction in the BP asymmetry: mean BP was 135/77mmHg in the right arm and 145/76mmHg in the left. The patient presented no new neurological events and the systematic examination revealed minimal residual ataxia, no vertigo signs, and remission of the left arm pain.
The most frequent aetiology in subclavian steal syndrome is atherosclerosis, followed in order of frequency by vasculitis, temporal arteritis, and embryonic malformation of the aortic arch and supra-aortic trunks.
Stenosis of the subclavian artery provokes a compensatory increase in flow in the contralateral vessels (which is responsible for the presence of a retrograde flow from the vertebral artery) to ensure adequate blood supply and improve perfusion in the affected territory.2 Vertebrobasilar insufficiency is infrequent, except in the event of a lesion affecting the contralateral vertebral artery or innominate artery stenosis.3
Only 5% of patients with subclavian steal syndrome develop neurological symptoms. Most patients present proximal stenosis of the subclavian artery, compromising circulation to the posterior cerebral artery territory, specifically the V4 segment, which supplies the brainstem and cerebellum. Clinical symptoms typically include vertigo, ataxia, dysarthria, syncope, diplopia, and monocular or binocular vision impairment.4
Arterial occlusion only occurs distally in rare cases, with the predominant symptom being claudication of the affected limb. Physical examination reveals asymmetric radial pulses, with a difference in BP of >20mmHg between arms; supraclavicular auscultation may reveal artery bruit, depending on the degree of stenosis.5
There are 4 types of subclavian steal syndrome, depending on ultrasound findings: type 1, proximal stenosis of the subclavian artery or brachiocephalic trunk; type 2, severe proximal stenosis of the subclavian artery; type 3, anterograde flow from the vertebral artery at rest; and type 4, anterograde flow from the subclavian artery.6
Diagnosis of vertebral subclavian steal syndrome is initially established if flow inversion in the vertebral artery is observed in a Doppler ultrasound study in patients with clinical suspicion. The study should be completed with a CT scan, MRI angiography, and arteriographic study,7 in order to locate the lesion precisely and assess treatment options. If vertebral subclavian steal syndrome is suspected, we should rule out such other causes as arrhythmias, poorly controlled hypertension, or pacemaker malfunction.8
Indications for revascularisation are presence of symptoms of vertebrobasilar ischaemia, or severe extracranial atherosclerotic disease. The aim of treatment is to restore anterograde flow in the vertebral artery in order to improve the cerebral hypoperfusion.
Endovascular treatment of the lesions to the prevertebral subclavian artery is the treatment of choice, presenting a high success rate, minimal complications, and a low mortality rate.9 This technique offers greater long-term permeability when revascularisation is indicated due to symptoms of vertebrobasilar ischaemia than when it is indicated due to upper limb ischaemia.10
Follow-up with Doppler ultrasound is very important in patients undergoing endovascular therapy in order to ensure the permeability of the stent.11
In addition to the invasive revascularisation treatment, we should not forget the importance of adequately controlling cardiovascular risk in these patients by closely monitoring and controlling BP, lipid profile, and anticoagulant treatment, given the reported association between coronary and peripheral artery disease.12
Our case illustrates the challenge of diagnosing subclavian steal syndrome as the cause of acute brain ischaemia. We stress the importance of simultaneously measuring BP in both arms; this should be performed routinely in all hypertensive patients as it is essential in the early diagnosis of the disease.
Please cite this article as: Antón Vázquez V, Armario García P, García Sánchez SM, Martí Castillejos C. Síndrome del robo de la subclavia. Una causa olvidada de isquemia cerebral aguda. Neurología. 2020;35:65–67.