Terminal branch neuralgia is characterised by pain circumscribed to the territory of a terminal nerve branch, accompanied by such signs of nerve dysfunction as allodynia, hyperalgesia, or hypoaesthesia.1,2 The second edition of the International Classification of Headache Disorders (ICHD-2) added pain resolution with selective anaesthetic block to the diagnostic criteria for the disorder.3 The supratrochlear nerve is a terminal branch of the frontal nerve, and is the longest terminal branch of the ophthalmic division of the trigeminal nerve. It provides sensory information from the skin and conjunctiva of the upper eyelid and the skin of the inferomedial area of the forehead.4
The findings most suggestive of vasculitis include neuropathies, with mononeuritis multiplex being most informative for diagnosis.5,6 Cranial nerve involvement is described in 0.7% of cases of vasculitis, with the trigeminal and facial nerves most commonly being affected.6 To date, no cases have been described of terminal branch neuralgia as a manifestation of systemic vasculitis. We present a case of terminal branch neuralgia of the trigeminal nerve (specifically, supratrochlear neuralgia) secondary to systemic vasculitis; neuralgia was also the initial manifestation of vasculitis.
The patient was a 41-year-old woman who, after her first pregnancy at the age of 18 years, began to present episodes of frontal headache. Symptom onset coincided with fever (38 °C), odynophagia, mouth ulcers, general discomfort, joint pain, swelling of both ankles, and non-painful, indurated, erythematous nodules on both legs (Fig. 1). A biopsy sample was taken of one of the nodules; the histology study revealed lobular panniculitis with vasculitis; the remaining complementary studies and aetiological study of vasculitis yielded negative results.
Since then, episodes of systemic symptoms have occurred approximately every 2 years, although headache episodes have occurred every 2 weeks, with a duration of 5-6 days, not coinciding or intensifying with the episodes of systemic symptoms. The patient described continuous pressing and stabbing pain circumscribed to the right medial supraciliary area, with an intensity of 6/10 on the verbal analogue scale (0: no pain; 10: worst imaginable pain). She presented no trigeminal autonomic symptoms, nausea, or vomiting, but did occasionally experience photo- and phonophobia when pain was most intense. She did not present aura, changes in pain in association with postural changes, or a specific temporal pattern of pain. Pain was more frequent in the perimenstrual period. The patient was using non-steroidal anti-inflammatory drugs and eletriptan for symptomatic treatment, with unsatisfactory results, and had received no preventive treatment.
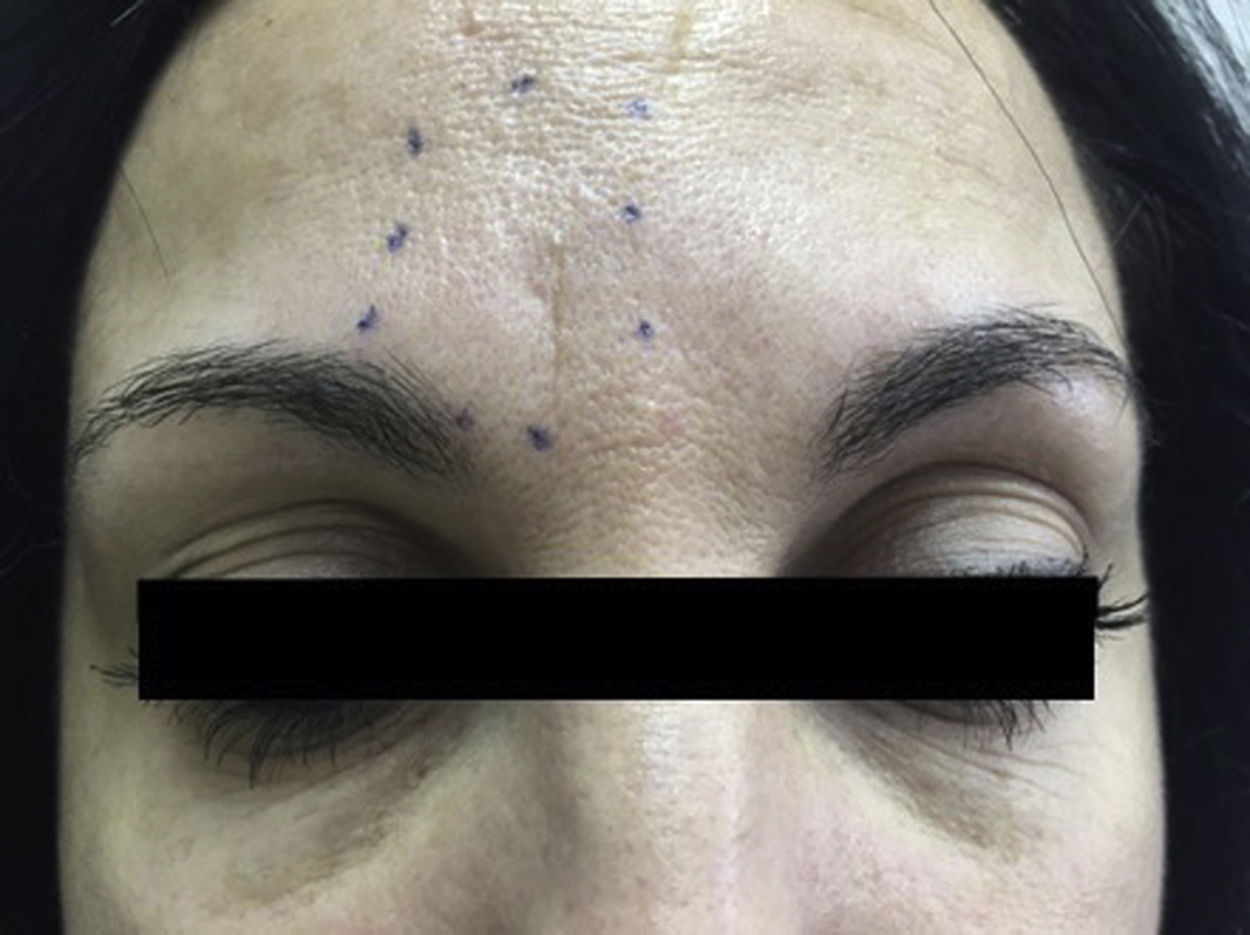
Twenty-three years after symptom onset, she was referred to the headache unit due to suspected migraine. Physical examination revealed pain upon palpation of the emergence of the right supratrochlear nerve and hypoaesthesia circumscribed to the medial supraciliary region (Fig. 2). A facial CT scan identified no local abnormalities. Suspecting supratrochlear neuralgia, we performed anaesthetic block with 0.5 cc of 1% lidocaine; pain completely resolved for 6 months, and subsequently returned periodically, with the effect of the nerve block persisting for 3-6 months. The patient has been under follow-up at the headache unit for 2 years.
To date, 17 cases have been reported of supratrochlear neuralgia,1,7 with 70.6% of patients being women; mean age is 44 years (range, 15-70). Pain is most frequently described as pressing (53%), burning (27%), or electric shock–like (6.6%). The frequency of episodes ranges from one per week to 10-15 per day. The mean diagnostic delay in the published cases is 6.8 years.7
Cases secondary to underlying causes have been described in practically all terminal branch neuralgias. The literature currently includes 24 cases of secondary supraorbital neuralgia,1,7 37 of infraorbital neuralgia,8–10 3 of lacrimal neuralgia, 7 of infratrochlear neuralgia, one of external nasal neuralgia, and 2 of nasal neuralgia.7 Secondary neuralgia has most frequently been reported in the mental nerve.11
Five cases have also been described of secondary supratrochlear neuralgia: one secondary to trauma, 2 following ophthalmological surgery, one due to trochlear inflammation, and one associated with varicella.3 As with other terminal branch neuralgias, underlying causes must be ruled out through neuroimaging studies and laboratory tests including immune markers.12
None of the reported cases of cranial nerve terminal branch neuralgia were secondary to vasculitis; ours is the first case of this association. The causal mechanism was probably inflammation of the vasa nervorum, resulting in compression and ischaemia.5,6 In our case, treatment with anaesthetic nerve block also led to a lasting clinical improvement. Therefore, we recommend considering this treatment option and bearing in mind the possibility of vasculitis as a potential cause of terminal branch neuralgia or neuropathy, especially in patients with accompanying systemic symptoms.
Please cite this article as: Méndez de Haro L, Guerrero Peral Á, García Azorín D. Neuralgia del nervio supratroclear: primer caso de neuralgia de ramo terminal facial como forma de presentación de una vasculitis. Neurología. 2021;36:653–654.