Autonomic symptoms may be the first manifestation of an epileptic seizure.1 The International League Against Epilepsy (ILAE) classification identifies autonomic seizures as focal non-motor seizures.2 Autonomic symptoms may range from subclinical changes to potentially fatal haemodynamic instability. The anatomical substrate of autonomic seizures generally resides in the central autonomic network. This network comprises the insular cortex, anterior cingulate cortex, amygdalae, hypothalamus, periaqueductal grey matter, parabrachial nucleus, solitary nucleus, rostral ventrolateral medulla, and raphe nucleus.3 We present the case of a patient with episodes of right hemibody hyperhidrosis secondary to insular dysplasia.
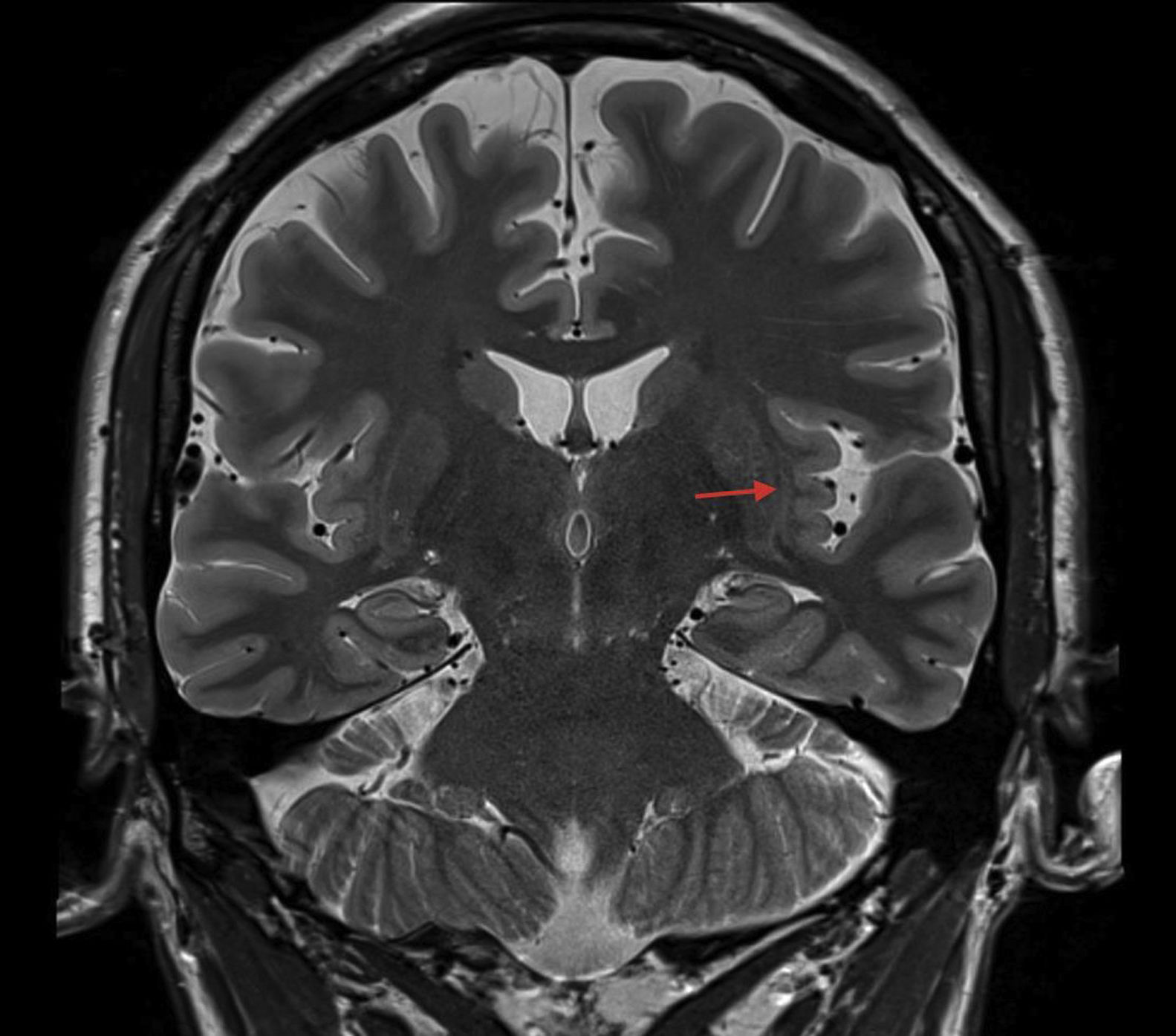
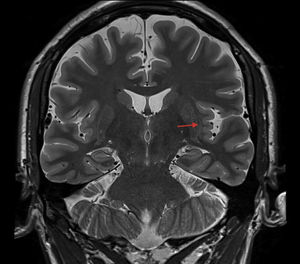
The patient was a 39-year-old right-handed man with no relevant medical history. From the age of 28, he had presented episodes of increased temperature and sweating on the right side of the face and body; episodes lasted 5-10minutes and did not involve altered level of consciousness (Fig. 1 and Appendix B). These episodes presented 6-7 times per day. The baseline sleep-deprived electroencephalogram (EEG) showed no epileptiform alterations. A brain magnetic resonance imaging (MRI) study (3T scanner) revealed radiological signs suggestive of polymicrogyria of the left insular cortex (Fig. 2). Suspecting focal autonomic seizures, we started treatment with eslicarbazepine acetate at 800mg/day; this reduced the number of seizures to the current frequency of one episode per month. Dosage is currently being adjusted; no video EEG monitoring has been performed due to a lack of availability at our centre and the good response to treatment.
Autonomic symptoms frequently present during seizures, either as the predominant manifestation or in association with other convulsive symptoms. They may be classified as cardiovascular changes, and respiratory, gastrointestinal, skin, pupillary, genitourinary, or sexual manifestations.4 Some of these signs and symptoms may help us to locate and lateralise the area of seizure onset and the subsequent route of propagation. They may also assist in understanding the anatomical and functional organisation of the central autonomic network.4
Previously described cutaneous manifestations include flushing, pallor, sweating, and piloerection. Autonomic symptoms have been attributed to different aetiologies: Franco et al.5 reported a patient with ipsilateral facial sweating secondary to anti-Ma2 autoimmune encephalitis associated with testicular teratoma. Sweating in the context of seizures has also been reported in a patient with a basal forebrain malformation, in association with tremor and hypothermia.6 Cases have also been reported of generalised sweating with other vegetative symptoms, with one case secondary to a periventricular lesion extending to the limbic area,7 and another as a consequence of a parietal meningioma.8
Previous cases have also been reported of episodes of hyperhidrosis and ictal piloerection of autoimmune origin in the temporal lobe. Other structures participating in the central autonomic network have less frequently been associated with pilomotor seizures.9 We present the first case of seizures presenting with hyperhidrosis and no piloerection, contralateral to insular polymicrogyria. Insular epilepsy is difficult to diagnose due to its clinical heterogeneity: with the exception of nociceptive symptoms, no clinical presentation is very specific of this location; autonomic symptoms have been described in this clinical entity.10 On many occasions, conventional EEG does not reveal alterations due to the deep location of the insula, which makes it necessary to perform video EEG monitoring in the event of treatment resistance.10 In our patient, the purely autonomic clinical presentation led us to consider the insula as a possible site of seizure onset, given its role in the central autonomic network; while non-specific, the absence of pathological data on the EEG may be compatible with alterations in this location, and the detection of a structural alteration in the MRI study together with the good response to antiepileptic drugs make us consider this diagnosis probable. One limitation of this study is the lack of video EEG monitoring or stereo EEG, which may help establish a more accurate electro-clinical correlate.
In conclusion, we present a case of autonomic seizures with hyperhidrosis probably caused by contralateral insular polymicrogyria. We consider it important to systematically describe more patients with infrequent autonomic symptoms, such as sweating, in order to establish the potential of these symptoms to locate and lateralise lesions.
FundingThe authors have received no external funding for this study.
Please cite this article as: López-Bravo A, Sanabria-Sanchinel AA, Marín-Gracia M, Viloria-Alebesque A. Sudoración como presentación de epilepsia focal: descripción de un caso clínico. Neurología. 2021;36:332–334.