Thirty percent of the patients for whom code stroke is activated have stroke mimics, the most common being epilepsy. Our purpose was to evaluate the usefulness of multiparametric CT for differentiating between seizure-related symptoms and vascular events.
Material and methodsWe conducted a retrospective observational study; data were gathered prospectively during one year. We studied multiparametric CT images of patients admitted following code stroke activation and finally diagnosed with epilepsy.
ResultsThe study included a total of 11 patients; 36% were men and mean age was 74.5 years. Three patients had right hemisphere syndrome, 4 displayed left hemisphere syndrome, and the remaining 4 had isolated aphasia. Maximum time from symptom onset to multiparametric CT study was 8.16hours. Perfusion CT results were normal in 2 patients. Nine patients showed longer or shorter times to peak (Tmax); cerebral blood volume (CBV) and cerebral blood flow (CBF) maps varied. EEG was performed a maximum of 47.6hours after symptom onset. Four patients showed findings compatible with status epilepticus, 2 displayed focal epileptiform activity, and 5 showed post-ictal slowing ipsilateral to perfusion CT abnormalities.
ConclusionThe most sensitive parameter for differentiating between stroke and epilepsy in our series was increased time to peak in multilobar cortical locations in the absence of large-vessel occlusion and basal ganglia involvement. Multiparametric CT is a fast, readily available, and useful tool for the differential diagnosis of acute-onset neurological signs of epileptic origin in patients initially attended after code stroke activation.
Tras la activación del código ictus, hasta un 30% de los pacientes presentan cuadros imitadores del ictus, siendo la epilepsia el más frecuente. Evaluamos la utilidad de la TC cerebral multiparamétrica para la diferenciación de los déficit de origen comicial versus vascular.
Material y métodosEstudio observacional retrospectivo con recogida prospectiva de datos. Se revisan imágenes de TC multiparamétrica de pacientes atendidos como código ictus durante un año que finalmente fueron diagnosticados de etiología comicial.
ResultadosN=11 (varones 36%, edad media 74,5años). Tres pacientes presentaban focalidad neurológica derecha, 4 focalidad izquierda y 4 afasia aislada. El tiempo máximo desde el inicio de la clínica hasta la realización de la TC multiparamétrica fue de 8,16h. La TC perfusión fue normal en 2 pacientes. Nueve pacientes mostraron alargamiento/acortamiento del tiempo al pico (Tmáx), siendo los mapas de flujo y volumen variables. El electroencefalograma se realizó con un tiempo máximo de evolución desde el inicio de la clínica de 47,6h. Cuatro registros mostraron hallazgos compatibles con estatus epiléptico, 2 actividad epileptiforme focal y los 5 restantes lentificación poscrítica ipsolateral a las anomalías de la TC perfusión.
ConclusiónEl alargamiento del tiempo al pico en una distribución cortical multilobar en ausencia de oclusión de gran vaso y con respeto de ganglios de la base ha resultado el parámetro más sensible para la diferenciación de estas entidades en nuestra serie. Consideramos que la TC cerebral multiparamétrica es una herramienta rápida, disponible y útil para el diagnóstico diferencial de síntomas neurológicos deficitarios de inicio brusco debidos a etiología comicial que son atendidos como código ictus.
Seizures are included in the differential diagnosis of acute stroke. Deficits occurring after a seizure or non-convulsive status epilepticus may be indistinguishable from those associated with stroke. These symptoms are known as “stroke mimics” and account for up to 31% of cases of focal neurological signs; in 20% of cases, symptoms are caused by seizures.1,2 Given that these symptoms may be indistinguishable from stroke symptoms, the availability of an effective diagnostic tool in emergency departments may prevent the administration of fibrinolytic therapy to patients with stroke mimics, which would be ineffective and potentially life-threatening and result in delayed administration of antiepileptic treatment.
It has been suggested that multiparametric CT may be useful for diagnosing ischaemic stroke as it reveals the area of penumbra and enables mismatch estimation to optimise fibrinolysis and interventionist treatment.3 For this reason our hospital's code stroke protocol requires that all patients with focal neurological signs and suspected stroke of less than 9hours’ progression and/or unknown onset time undergo multiparametric CT as part of the routine evaluation.
Cerebral perfusion maps are based on sequential CT slices acquired during the administration of an iodinated contrast agent. Perfusion CT is a fast, non-invasive technique for evaluating cerebral perfusion. It comprises 3 maps:
- (1)
Time to peak (TTP/Tmax): time to the maximum concentration of contrast in brain tissue.
- (2)
Cerebral blood volume (CBV), which indicates blood volume per unit of brain mass (normal range, 4-6mL/100g).
- (3)
Cerebral blood flow (CBF), which indicates the volume of blood flow per unit of brain mass per minute (normal range, 50-60mL/100g/minutes).
Tmax has the greatest sensitivity for detecting cerebral ischaemia, whereas CBV and CBF are more specific.4
Cerebral perfusion studies are a widely accepted method for localising the epileptogenic focus in patients with seizures; the study of epilepsy with perfusion CT has been addressed by multiple researchers.5–8
The purpose of this study is to analyse brain CT images from a series of patients who were attended at our hospital's emergency department following code stroke activation and ultimately diagnosed with epilepsy. We also aimed to analyse perfusion CT findings from the perspective of the hypothesis that changes in brain metabolism during seizures can be identified in perfusion CT images.
Material and methodsWe conducted a retrospective observational study with prospective data collection. We gathered the clinical histories of patients attended at the emergency department following code stroke activation between May 2014 and December 2015 and finally diagnosed with epileptic seizures or status epilepticus based on clinical and/or EEG criteria. We excluded all patients for whom no follow-up neuroimages (CT or MRI) or EEG data were available.
We also gathered demographic, clinical, and complementary test data for each patient. All patients were evaluated by on-call neurologists and radiologists at the emergency department, and underwent baseline brain CT, CT-angiography, and perfusion CT studies. Images were subsequently analysed by our hospital's neuroradiology department.
Images were obtained using a Siemens Somatom 40 CT scanner. We obtained baseline CT slices measuring 2.5mm in the posterior fossa and 4.8mm in the supratentorial region. For perfusion CT, 80mL of a contrast agent (Omnipaque 350mg) was administered at a rate of 5mL/seconds via an 18-gauge venous catheter; gantry rotation time was 1second. We selected the site of perfusion CT assessment according to the potentially involved territory; we acquired 3 slices of 9.6mm thickness with the following parameters: field of view 238mm, radiation 270mAs, 80kV. For CT-angiography, we obtained 3-mm slices from carina to the vertex; datasets could be reconstructed with 0.6mm slice thickness, field of view 244mm, 120kV, and 160mAs. Acquisition time was 16seconds and rotation time 0.5seconds.
ResultsThe study included 11 patients, 36% of whom were men. Mean age was 74.45±18.15 years (range, 39-93). One patient (patient 5) had a history of stroke, 2 had self-limiting symptoms with a final diagnosis of transient ischaemic attack, and 2 had history of focal epilepsy triggered by brain injuries secondary to severe head trauma and were receiving antiepileptics. Another patient had a history of epilepsy in the context of alcohol withdrawal.
Four patients (36.36%) showed symptoms of isolated aphasia, 4 had left hemisphere syndrome, and 3 had right hemisphere syndrome. Mean NIHSS score was 10.1±7.14 (range, 1-26).
Eight patients were transferred to the hospital with an unknown progression time. The maximum progression time was estimated at 8.16±6.20hours (range, 1.3-24), based on the last time patients were known to be asymptomatic.
In the baseline CT scan, the 2 patients with a history of head trauma and the patient with a history of stroke showed signs of known encephalomalacia. Baseline CT scan results were normal in the remaining 8 patients. No patient showed signs of large-vessel occlusion on CT-angiography.
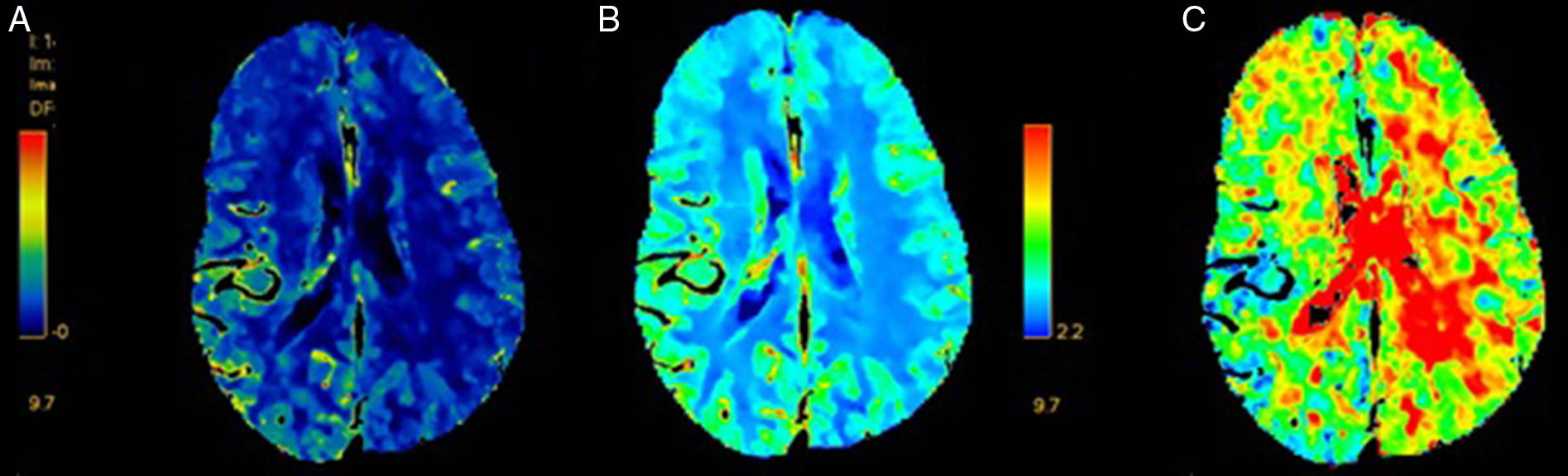
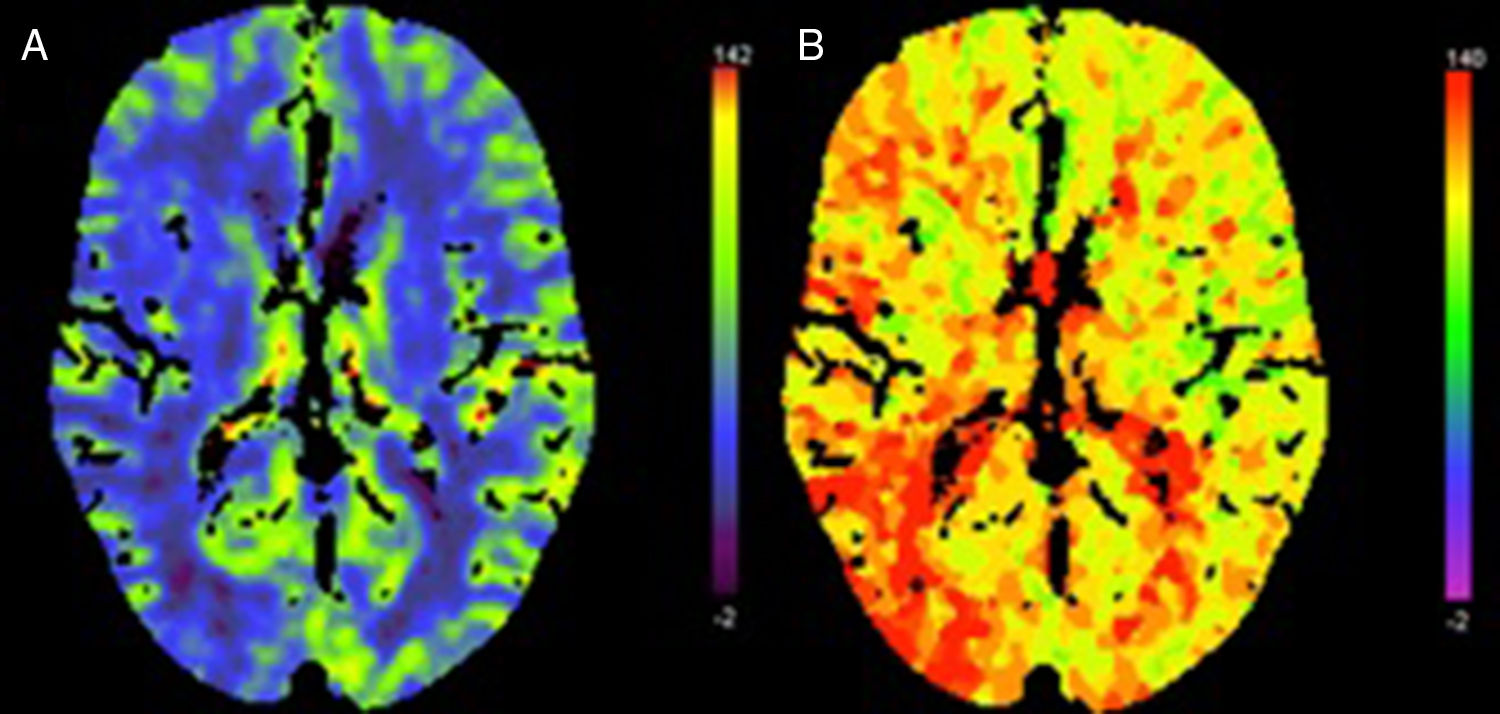
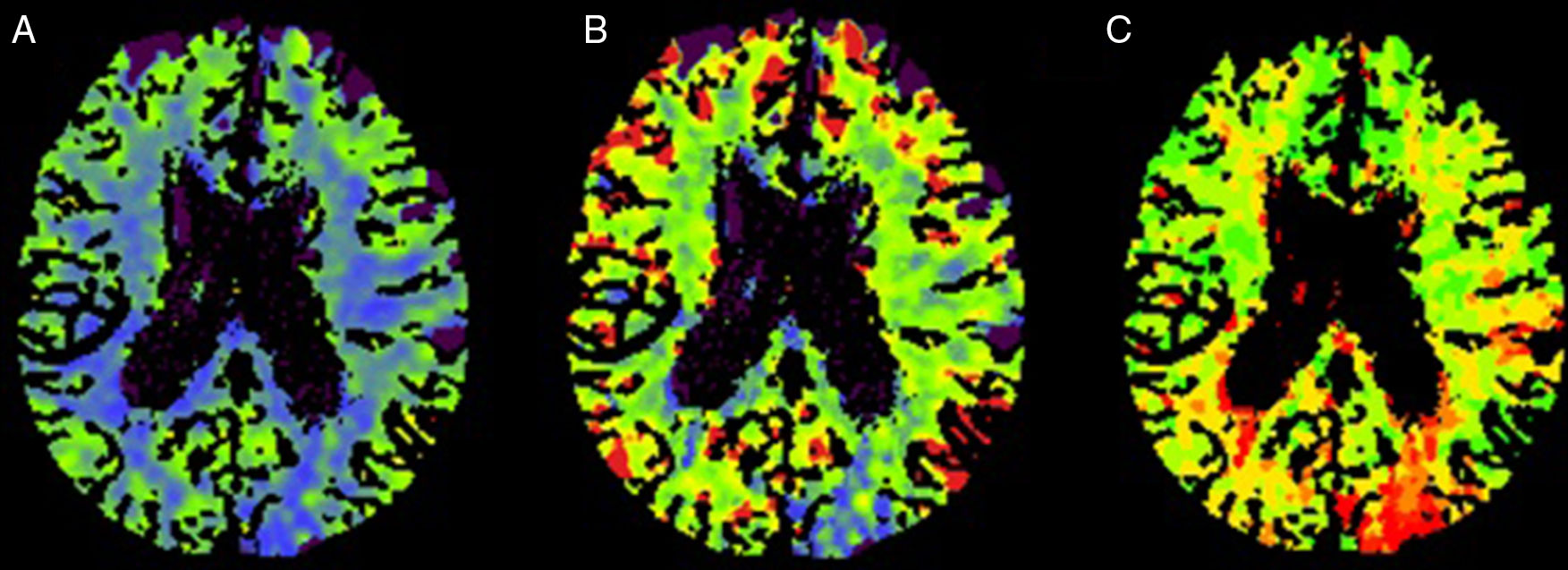
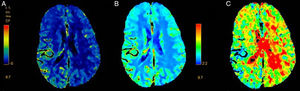
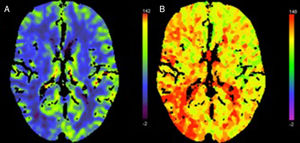
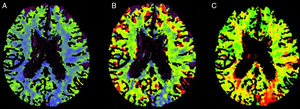
Two patients showed normal perfusion, with no asymmetries in CBV, CBF, or time to peak (Tmax). The most frequent finding in the rest of the sample was longer time to peak (Tmax), with varying CBF and CBV (Figs. 1–3).
Perfusion CT scan from patient 6. Right hemisphere syndrome (NIHSS score: 12). (A) Increased CBF in the right hemisphere. (B) Increased CBV in the right hemisphere. (C) Shorter Tmax at a similar location in the cortex. Changes do not clearly correspond to a specific vascular territory. CT-angiography revealed no large-vessel occlusion.
Perfusion CT scan from patient 7. Right hemisphere syndrome (NIHSS score: 6). (A) Decreased CBF in the right hemisphere. (B) Longer Tmax at a similar location in the cortex. Changes do not clearly correspond to a specific vascular territory. CT-angiography revealed no large-vessel occlusion.
Perfusion CT scan from patient 9. Left hemisphere syndrome (NIHSS score: 10). (A) Decreased CBF in the left parieto-occipital area. (B) Decreased CBV in the left parieto-occipital area. (C) Longer Tmax at a similar location in the cortex. Changes do not clearly correspond to a specific vascular territory. CT-angiography revealed no large-vessel occlusion.
EEG was performed a mean of 47.63±41.32hours after symptom onset (range, 4-120). In 4 cases, EEG recordings were compatible with non-convulsive status epilepticus (Table 1). Two patients showed epileptiform activity, with spikes and sharp waves. The remaining 5 patients displayed slow activity in the same hemisphere where multimodal CT detected abnormalities (3 hemispheric and 2 temporal).
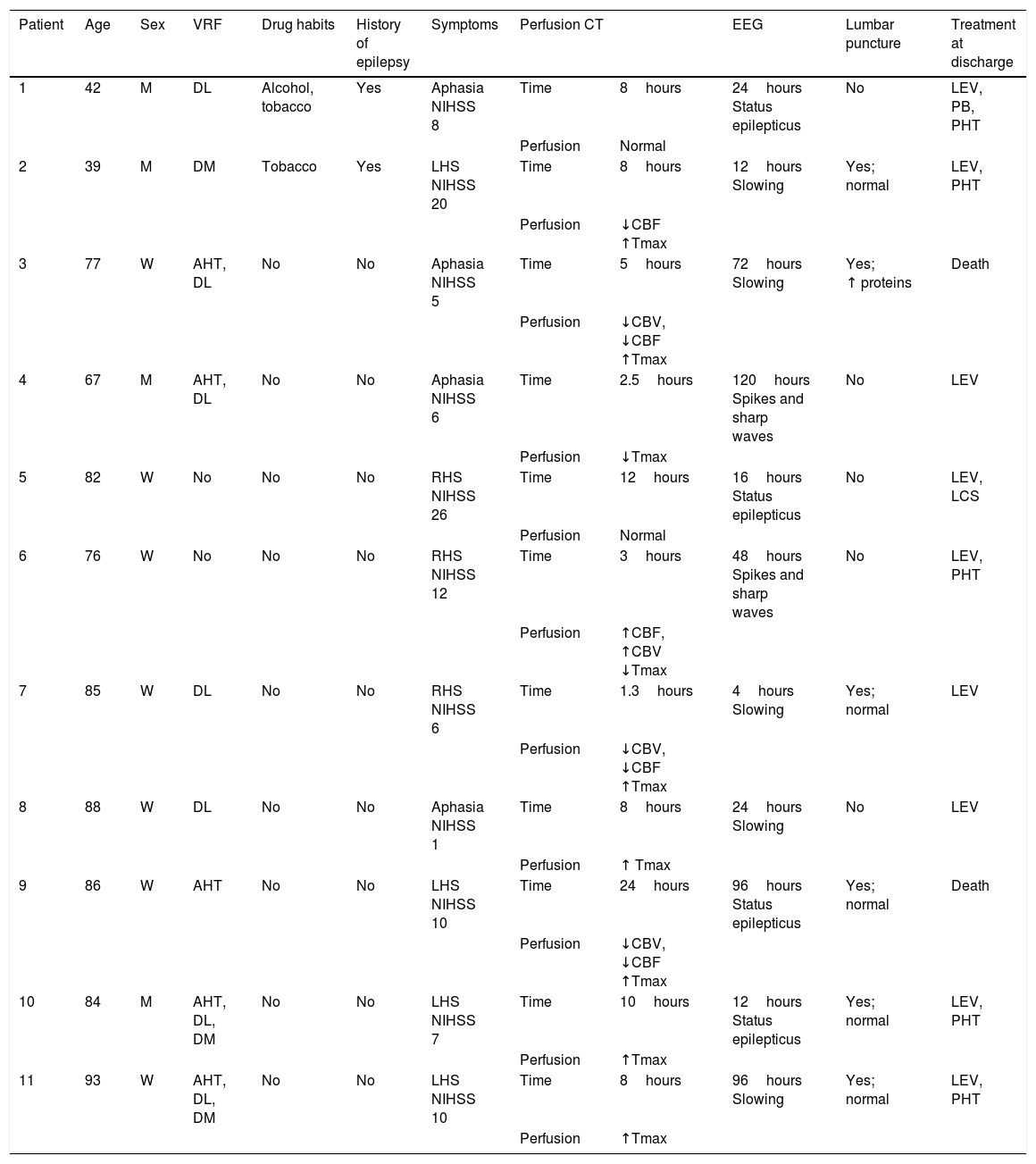
Clinical characteristics, complementary test results, and treatments in our sample.
| Patient | Age | Sex | VRF | Drug habits | History of epilepsy | Symptoms | Perfusion CT | EEG | Lumbar puncture | Treatment at discharge | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 42 | M | DL | Alcohol, tobacco | Yes | Aphasia NIHSS 8 | Time | 8hours | 24hours Status epilepticus | No | LEV, PB, PHT |
| Perfusion | Normal | ||||||||||
| 2 | 39 | M | DM | Tobacco | Yes | LHS NIHSS 20 | Time | 8hours | 12hours Slowing | Yes; normal | LEV, PHT |
| Perfusion | ↓CBF ↑Tmax | ||||||||||
| 3 | 77 | W | AHT, DL | No | No | Aphasia NIHSS 5 | Time | 5hours | 72hours Slowing | Yes; ↑ proteins | Death |
| Perfusion | ↓CBV, ↓CBF ↑Tmax | ||||||||||
| 4 | 67 | M | AHT, DL | No | No | Aphasia NIHSS 6 | Time | 2.5hours | 120hours Spikes and sharp waves | No | LEV |
| Perfusion | ↓Tmax | ||||||||||
| 5 | 82 | W | No | No | No | RHS NIHSS 26 | Time | 12hours | 16hours Status epilepticus | No | LEV, LCS |
| Perfusion | Normal | ||||||||||
| 6 | 76 | W | No | No | No | RHS NIHSS 12 | Time | 3hours | 48hours Spikes and sharp waves | No | LEV, PHT |
| Perfusion | ↑CBF, ↑CBV ↓Tmax | ||||||||||
| 7 | 85 | W | DL | No | No | RHS NIHSS 6 | Time | 1.3hours | 4hours Slowing | Yes; normal | LEV |
| Perfusion | ↓CBV, ↓CBF ↑Tmax | ||||||||||
| 8 | 88 | W | DL | No | No | Aphasia NIHSS 1 | Time | 8hours | 24hours Slowing | No | LEV |
| Perfusion | ↑ Tmax | ||||||||||
| 9 | 86 | W | AHT | No | No | LHS NIHSS 10 | Time | 24hours | 96hours Status epilepticus | Yes; normal | Death |
| Perfusion | ↓CBV, ↓CBF ↑Tmax | ||||||||||
| 10 | 84 | M | AHT, DL, DM | No | No | LHS NIHSS 7 | Time | 10hours | 12hours Status epilepticus | Yes; normal | LEV, PHT |
| Perfusion | ↑Tmax | ||||||||||
| 11 | 93 | W | AHT, DL, DM | No | No | LHS NIHSS 10 | Time | 8hours | 96hours Slowing | Yes; normal | LEV, PHT |
| Perfusion | ↑Tmax | ||||||||||
AHT: arterial hypertension; CBF: cerebral blood flow; CBV: cerebral blood volume; DL: dyslipidaemia; DM: diabetes mellitus; EEG: electroencephalography; LCS: lacosamide; LEV: levetiracetam; LHS: left hemisphere syndrome; M: man; NIHSS: National Institutes of Health Stroke Scale; PB: phenobarbital; PHT: phenytoin; RHS: right hemisphere syndrome; Tmax: time to peak; VRF: vascular risk factors; W: woman.
In all cases, follow-up neuroimaging studies revealed no changes with respect to baseline.
In our sample, epilepsy was triggered by increased alcohol use (patient 1), reduction of antiepileptic drug dose (patient 2), sepsis (patient 7), and a previous structural lesion (patient 3). Two patients died due to complications associated with status epilepticus (aspiration pneumonia).
Table 1 shows patients’ medical histories, clinical characteristics, and complementary test results.
DiscussionWe studied multiparametric CT findings from 11 patients attended following code stroke activation who were finally discharged with a diagnosis of epilepsy according to clinical criteria or EEG findings. The most frequent perfusion CT finding was longer time to peak (Tmax) in 6 of the 11 patients; 3 of this group showed no alterations in CBF and CBV. No patient showed large-vessel occlusion; in all cases, multiparametric CT alterations did not correspond to any vascular territory and were predominantly cortical and multilobar. In all patients, EEG abnormalities were ipsilateral to perfusion CT alterations and consistent with the symptoms displayed.
Functional brain MRI and SPECT studies have shown changes in cerebral perfusion and metabolism that are suggestive of a hypermetabolic state during the ictal period and a hypometabolic state in the postictal period.9,10
Likewise, perfusion CT findings vary depending on when the scan is performed, that is whether the patient is in the ictal, interictal, or postictal period. According to the literature, perfusion CT shows shorter time to peak (TTP/Tmax) and increased CBF and CBV during seizures, which is consistent with hyperaemia,5,7 and longer time to peak (TTP/Tmax) (suggestive of hypoperfusion) in the postictal stage.7,11–14 In the interictal period, perfusion CT reveals longer TTP/Tmax and decreased CBV and CBF, as occurs with vascular events. However, these alterations usually affect more than one vascular territory and are predominantly cortical, with no involvement of the underlying white matter.15 These findings agree with our results.
The changes described previously are not pathognomonic of epileptic seizures; rather, they may be found in a wide range of conditions (infections, migraine, reperfused infarction, etc.11,15), which stands in contrast with the findings described in patients with acute ischaemic stroke. In clinical practice, early seizures may also appear in patients with stroke, especially haemorrhagic stroke: frequency ranges between 3.6% in patients over 85 years and 4.9% in younger patients.16 These cases are associated with a poorer prognosis.17 None of the patients in our sample showed signs of haemorrhage or large-vessel occlusion on CT, and a follow-up study ruled out ischaemia and acute/subacute cerebral haemorrhage.
Multiparametric CT is available in many emergency departments, and images are quick and easy to obtain and interpret; this tool is therefore especially beneficial in differential diagnosis including acute ischaemic stroke. This stands in contrast with the lack of availability of EEG equipment in some emergency departments, which may result in delayed diagnosis and treatment when no other complementary tests are available.
Given the unknown origin of our patients’ focal neurological signs, multiparametric CT scans were necessary to confirm vascular aetiology and determine eligibility for reperfusion therapy. None of the patients received fibrinolytic therapy as they were all outside the therapeutic window and had fluctuating symptoms or other contraindications. In many cases, early antiepileptic treatment was administered due to the patient's symptoms and multiparametric CT results, although these were not a determining factor for the decision not to administer fibrinolytic therapy or endovascular treatment in any case.
Perfusion CT does have some limitations. Firstly, it only examines axial slices of brain tissue measuring 20 to 40mm thick. Second, acquisition takes only seconds. Caution should therefore be exercised when establishing correlations between CT map findings and ictal, interictal, and postictal stages; epileptic seizures are dynamic processes involving constant electric changes and EEG recordings were not obtained simultaneously with perfusion CT. Furthermore, abnormalities on multiparametric CT scans are not pathognomonic of epileptic seizures, as other conditions may cause similar alterations; treatment decisions should not be made exclusively on the basis of these results. The small size and the heterogeneity of our sample also constitute a limitation to our study.
ConclusionsAlthough epileptic seizures or status epilepticus are diagnosed based on clinical and/or EEG findings, perfusion CT alterations suggestive of seizures may inform diagnosis.
In our series, the most sensitive parameter for diagnosing epileptic seizures or status epilepticus was longer time-to-peak in a multilobar cortical distribution, with no large-vessel occlusion or basal ganglia involvement. Although a larger sample would be necessary to confirm our results, we feel that multiparametric CT is a quick-to-administer, readily available technique which is useful for the differential diagnosis of sudden-onset deficits of epileptic origin in patients attended at emergency departments after code stroke activation. This tool may reduce the risk of iatrogenesis and help in early diagnosis and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNo funding was received for this study.
Please cite this article as: López Ruiz R, Quintas S, Largo P, de Toledo M, Carreras MT, Gago-Veiga A, et al. Utilidad de la tomografía computarizada cerebral multiparamétrica en el diagnóstico diferencial de patología comicial en el código ictus. Estudio preliminar. Neurología. 2019;34:73–79.
Some of the patients in this study were also included in a study presented as an oral communication at the 67th Annual Meeting of the Spanish Society of Neurology under the title “Multiparametric CT for the differential diagnosis of epilepsy in code stroke,” and in poster format at the 2016 European Stroke Organisation Conference and the 2016 Congress of the European Academy of Neurology under the title “CT perfusion [CTP] findings in stroke-mimics of epileptic origin.”