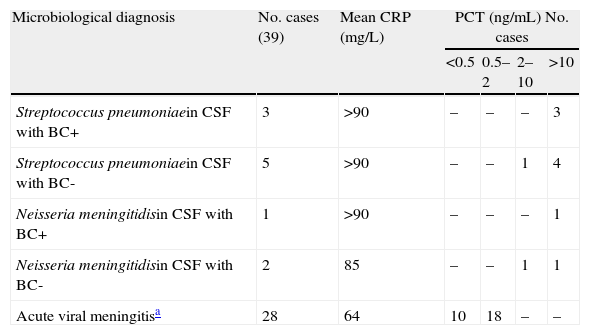
It was with great interest that we read the article by Jiménez Caballero et al.1 relating a descriptive analysis of cases of viral meningitis and their different characteristics in children and adults. We have been studying all diagnosed cases of central nervous system infections (CNSI) cared for by our emergency department (ED) for many years. In these cases, immediate and appropriate action has a crucial effect on the microbiological diagnosis, prognosis, and morbidity and mortality. However, one of the most important decisions made by an ED providing care to patients with acute meningitis (AM) is determining whether the meningitis is bacterial (BM) or viral (VM). This information allows professionals to administer the proper antimicrobial drug as soon as it is needed.2,3 We believe that cooperation between the ED doctor, the on-call neurologist, and the microbiology department is essential (quality of care is the result of teamwork with each member of the team performing properly). In the ED, doctors should immediately consider the possibility of AM and discuss possible diagnoses (in priority order) with the neurologist and microbiologist when necessary. Among other reasons, this is because the amount of cerebrospinal fluid (CSF) is limited.4 After lumbar puncture has been performed, and depending on the CSF's cytochemical profile, (pleocytosis, spinal fluid protein concentration, spinal fluid glucose concentration), lactate levels, and opening pressure, doctors should then order a microscopic examination, Gram staining, and bacterial antigen test (pneumococcal, meningococcal, etc.) while awaiting results from the CSF culture and any necessary blood cultures. In addition, as stated by Laguna del Estal,5 polymerase chain reaction (PCR) may prove to be a relatively rapid (results in 24hours) and very useful tool for identifying isolated cases or outbreaks in the ED. This technique is being incorporated in clinical practice in EDs.6 Nevertheless, in cases with an unclear CSF profile, prior use of antibiotics (partially-treated AM), no results from the Gram stain, or symptoms of sepsis (S), severe sepsis (SS), or septic shock (SSh), procalcitonin (PCT) and C-reactive protein (CRP) may be useful biomarkers in the ED. This test, which requires a small blood sample and can be processed in 20minutes, is helpful in distinguishing BM from VM and in deciding which blood cultures are needed, how best to administer early treatment with targeted antimicrobial drugs, and which department should admit the patient.5,7 We believe that biomarkers help predict whether or not the systemic reaction in AM is due to a bacterial infection, as this may be more difficult to determine in some cases than others.8 With that view in mind, we retrospectively included all adults diagnosed with AM between 1/1/2006 and 1/11/2010 who had undergone a PCT and CRP analysis (a total of 39 cases). AM was pronounced bacterial if the bacteria or its antigens could be isolated in CSF and viral if it met the criteria described by Jiménez Caballero et al.1 We used our laboratory's normal reference values: 0 to 8mg/L for CRP and PCT<0.5ng/mL. We determined PCR by using the quantitative method of enzyme immunoassay with a sensitivity of 1mg/L (VITROS CRP® slide for biochemistry). PCT was first measured with an immunochromatographic PCT-Q method (BRAHMS-PCT®) with semiquantitative evaluation, followed by ELECSYS (BRAHMS PCT®) with quantitative evaluation (these latter results were included in the intervals corresponding to the semiquantitative measurement). We used SPSS software version 15 for Windows (t-test for normal distributions and the χ2 test for proportions) in the comparative analysis. P<.05 was considered statistically significant. Table 1 shows results (the most frequently isolated strains) that suggest that levels of PCT>2ng/mL (P<.05) may be useful in distinguishing between bacterial and viral AM, and that values as low as PCT 10ng/mL (and CRP>90mg/L) in these patients predict the presence of bacteraemia and increased risk of clinical progression to SS-SSh, as other studies have shown.9 These results confirm that PCT is more sensitive and specific than CRP in cases of AM. The test predicts bacterial origin, the presence of bacteraemia and clinical progression to SS-SSh. As a result, it may be a very useful tool for decision-making in the ED. Until we possess results from future studies with correct methodology and sufficient sample sizes, we can state that PCT seems to be useful in the ED in cases of AM. PCT helps doctors activate ‘code meningitis’ or ‘code sepsis’ teams and deliver the right antibiotic treatment in a timely fashion. Protocols have been established in a number of EDs in recent years, especially for patients with S-SS-Sh.10
CRP and PCT values in acute meningitis.
| Microbiological diagnosis | No. cases (39) | Mean CRP (mg/L) | PCT (ng/mL) No. cases | |||
| <0.5 | 0.5–2 | 2–10 | >10 | |||
| Streptococcus pneumoniaein CSF with BC+ | 3 | >90 | – | – | – | 3 |
| Streptococcus pneumoniaein CSF with BC- | 5 | >90 | – | – | 1 | 4 |
| Neisseria meningitidisin CSF with BC+ | 1 | >90 | – | – | – | 1 |
| Neisseria meningitidisin CSF with BC- | 2 | 85 | – | – | 1 | 1 |
| Acute viral meningitisa | 28 | 64 | 10 | 18 | – | – |
BC−: negative blood cultures; BC+: positive blood culture; CRP: C-reactive protein; PCT: procalcitonin.
P<.05 in comparisons of PCT and CRP levels between viral and bacterial AM cases (cut-off point determined for PCT: 2ng/mL).
Please cite this article as: Julián-Jiménez A, et al. Utilidad de la procalcitonina y la proteína c reactiva en las meningitis agudas en urgencias. Neurología. 2013;28:189-90.