It was with great interest that we read the article published by E. Durán Ferreras analysing the complications of epidural anaesthesia with reference to a case in which VI cranial nerve palsy (CNP) developed.1
The doctor presents an excellent review of the history of complications that have been described after lumbar puncture (LP), the physiopathological mechanisms that may be involved, and a description of the most common clinical presentations. The article suggests conservative treatment measures including rest, hydration, and analgesia. In many cases, this approach delivers spontaneous resolution of symptoms at some point between 2 weeks and more than 3 months. It also describes use of epidural blood patches which give mixed results, depending on how soon they are used after symptom onset.
We recently treated a patient whose clinical description was similar to that in the cited article. She had an excellent response to treatment with an epidural blood patch given 72 hours after onset of diplopia.
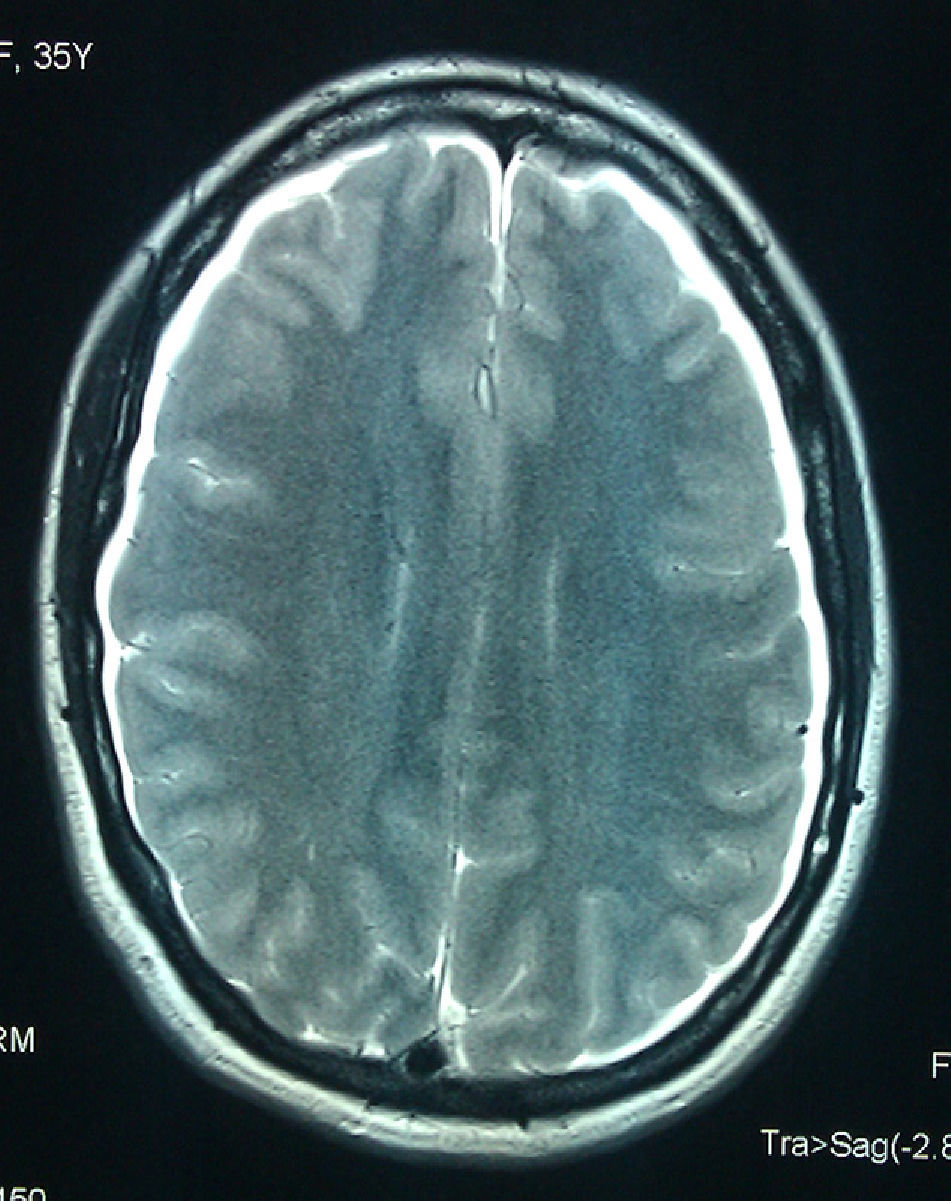
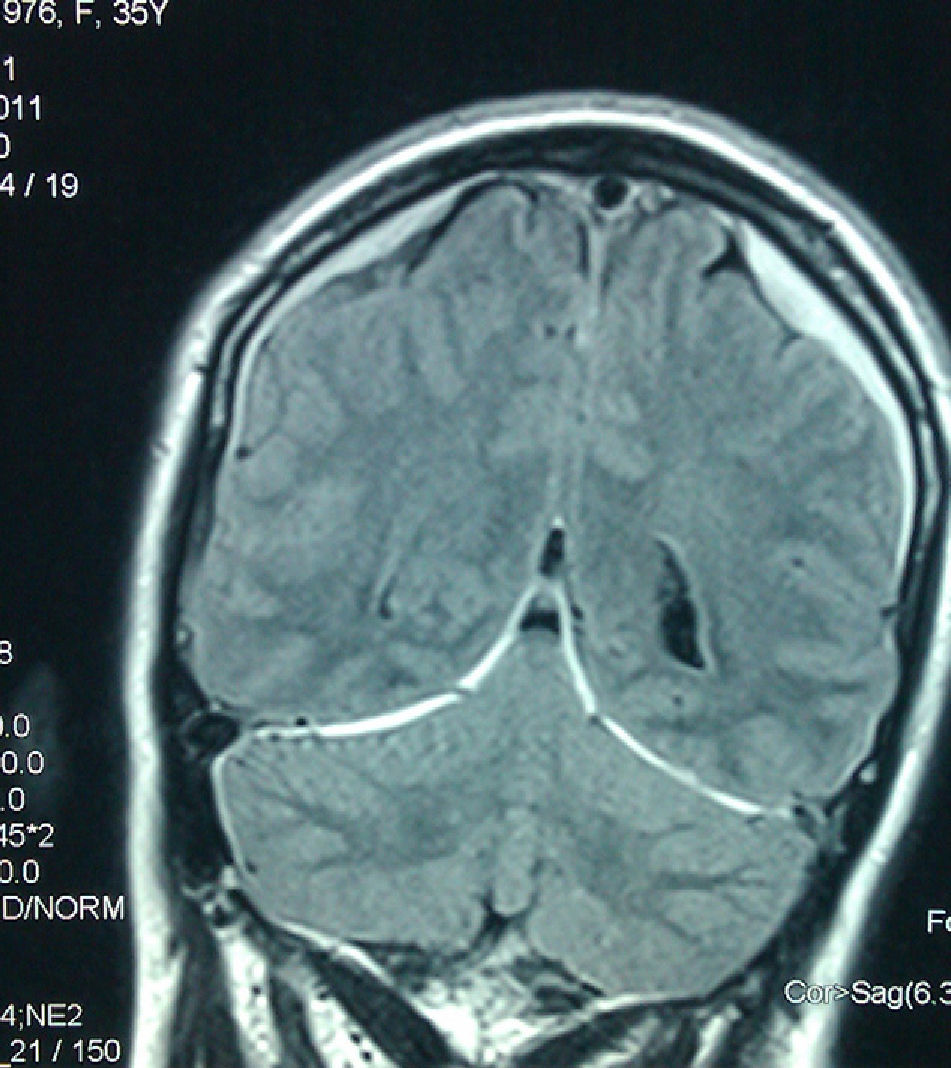
This 35-year-old female received an epidural during childbirth; on the following day, she experienced an intense generalised headache that intensified in a vertical position and improved upon lying down, accompanied by nausea and pain in the nuchal area. Doctors immediately employed conservative treatment measures with rest, hydration, and analgesics (metamizole+codeine, NSAIDs); the patient improved somewhat, and the doctors decided to discharge her. The patient was readmitted 5 days later due to recurrence of a similar headache and appearance of double vision when gazing to the right. Examination showed right VI CNP with no other changes. It was at that time that our department was contacted and the patient referred for care in our centre. An MRI scan (Figs. 1 and 2) revealed findings compatible with cerebrospinal fluid hypotension; bilateral subdural hygromas were present. As the headache and diplopia persisted despite hydration and analgesia, we consulted with the anaesthesiology division and decided to treat with a 20cc autologous blood patch at 72 hours after onset of VI CNP. The patient's headache and diplopia both improved gradually in the 24 hours following the procedure. The patient was discharged 72 hours after treatment, at which time the diplopia had abated and she was able to stand without experiencing further headaches.
Although most published cases report complete and spontaneous resolution of VI CNP after LP within several weeks or even months after onset of the deficit, there are also other cases that do not progress well and require more aggressive treatment, including surgical treatment.2,3 Diplopia and headache are debilitating symptoms that limit patients’ daily life activities and require use of the most effective treatment possible. The literature states that autologous blood patches are only effective for cases of post-LP headaches and diplopia in which treatment is initiated in the first 24 hours after VI CNP appears.4–6 The interesting feature of this case is that treatment delivered excellent results even though the epidural blood patch was administered 72 hours after palsy onset.
In conclusion, we would like to suggest considering treatment with an epidural blood patch even when more than 24 hours have passed since the onset of CNP. This treatment may significantly accelerate the patient's recovery.
Please cite this article as: Pulido Fontes L, et al. Paresia del VI par craneal tras anestesia epidural. Neurología. 2012;27:442–3.