Dear Editor:
Brain cysts are a relatively common incidental finding. They are typically stable over time, asymptomatic, and have no pathological repercussions. However, when they present changes in successive imaging studies, differential diagnosis must be expanded.
We present the case of a 62-year-old woman with no relevant history who developed asymptomatic cystic dilatation of a perivascular space after endovenous treatment of a saccular aneurysm of the middle cerebral artery.
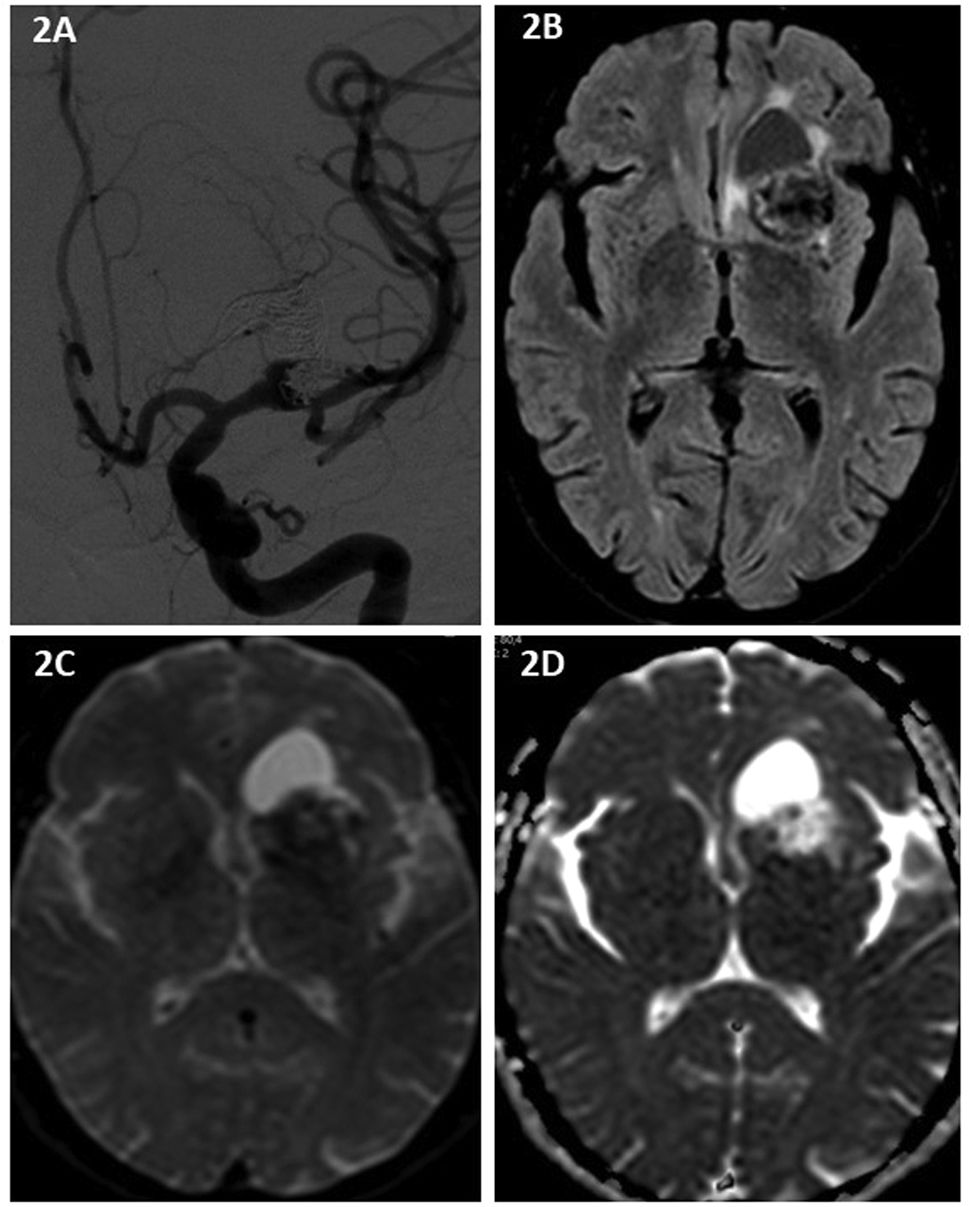
The patient attended the emergency department in December 2014 due to several days' history of left retro-ocular headache radiating to the ear, accompanied by vomiting and hypersensitivity to sound and light. She underwent CT scans with and without contrast, revealing an aneurysm on the left middle cerebral artery measuring 27 × 8 mm (dome-to-neck ratio of 3.4), which presented partial thrombosis and no signs of acute bleeding. The patient underwent endovascular treatment with endoprosthesis placement and platinum coil embolisation, achieving incomplete exclusion of the aneurysm; the procedure was completed without incident. In 2016, a second embolisation procedure was required due to permeability of a small residual neck. A follow-up angiography study conducted in 2018 showed complete exclusion of the aneurysm.
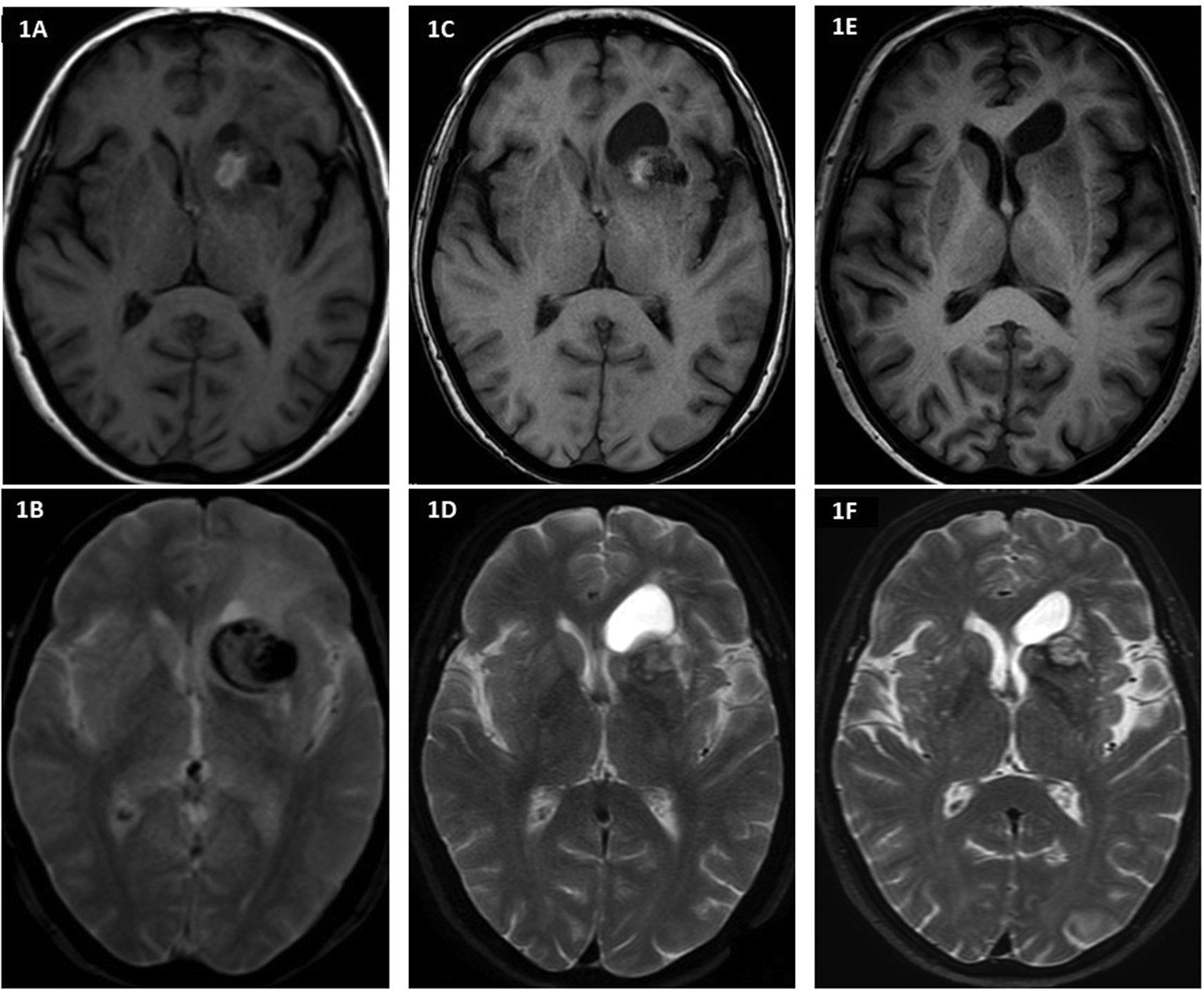
A follow-up MRI study revealed the formation and growth of a homogeneous cystic lesion (Fig. 1), which was practically isointense to CSF on all sequences, located adjacent to the dome of the embolised aneurysm (Fig. 2). The cyst reached a maximum size of 28 × 20 mm in September 2017, and progressively decreased in size after the complete occlusion of the aneurysm, reaching 16 × 8 mm at the time of the last follow-up study in February 2021. The patient remained asymptomatic at all times. Due to its imaging characteristics and progression over time, the lesion was diagnosed as cystic dilatation of a perivascular space, whose origin and involution were attributed to the endovascular treatment of the aneurysm.
The patient had no history of subarachnoid haemorrhage, and the lesion progressed asymptomatically, with no need for specific treatment. All of these characteristics are commonly reported in the scarce literature on the subject (prevalence of approximately 74% for each).1 However, the fact that the cyst appeared during follow-up of the aneurysm, rather than at onset, is rather unusual (approximately 26% of cases in the largest reported series).1
Perivascular spaces, or Virchow-Robin spaces, are small sleeve-like cavities that surround the walls of cerebral vessels. In MRI studies, they appear as thin, elongated structures with very similar signal intensity to that of the CSF,2,3 and typically appear in the basal ganglia (type I), subcortical white matter (type II), or brainstem (type III).2–4 They increase in number and become more apparent with age, and are considered dilated when they present a diameter > 1 mm.5
They are thought to be associated with the clearance of substances, although their connection with the CSF and cervical lymphatic system is not well demonstrated.2 Their clinical significance remains under study,4 and it has been suggested that they may be involved in numerous diseases of the central nervous system, including some types of dementia, Parkinson's disease, autism spectrum disorders, and recurrent ischaemic brain disease.4–8
Dilatation of perivascular spaces often co-presents with small vessel disease, together with lacunar infarcts, white matter signal alterations, and microhaemorrhage.4,9 These spaces must not be mistaken for lacunar infarcts, which are typically larger, with a diameter greater than 3 mm.2
A much rarer finding is the presence of cystic dilatation associated with an aneurysm (perianeurysmal cyst); this situation requires management of both lesions, and surgical resection and potentially aneurysm clipping are indicated in the event of a mass effect with clinical repercussions.1
The “pulsatile hammering” aetiological hypothesis, according to which arterial pulsation displaces the adjacent tissue,1 may at least partially explain the origin of the cyst, with the platinum coils used in the endovascular embolisation procedure potentially even intensifying this hammering effect. The progressive appearance of intra-aneurysmal thrombosis subsequent to endovascular occlusion probably eliminated the pulsatile component of the aneurysm. These 2 pathophysiological factors, inherent to this type of treatment, may explain the progression observed in imaging studies, in terms of both the development and the subsequent partial involution of the cyst. It also seems likely that the aneurysm itself caused an alteration to the perivascular clearance of CSF; this is consistent with the findings of experimental studies with animals and small observational studies in humans.2,3
In conclusion, while this finding is rare, correct diagnosis is important to rule out such other diseases as cystic neoplasm and abscesses, which may require aggressive treatment and lead to iatrogenesis. Therefore, it is essential to perform contrast-enhanced imaging studies to rule out lesion enhancement and to identify the aneurysm.
Ethical considerationsThis study complies with our centre's protocols for the publication of patient data and have obtained the corresponding permissions.
Conflicts of interestThe authors have no conflicts of interest to declare.
FundingNone.