Dear Editor:
Spinal arachnoid cysts (SAC) are a rare cause of spinal cord compression and are frequently considered to be congenital. Proliferation of arachnoid trabeculae has been proposed as the underlying pathophysiological mechanism. SACs most frequently present in the dorsal region of the thoracic spinal cord and are usually intradural. They tend to develop progressively, with compressive myelopathy, causing lower limb weakness, hypoaesthesia, gait alterations, and neuropathic pain.1,2
We describe the atypical presentation of an extensive intradural SAC affecting the cervical and thoracic regions in a 53-year-old woman with no relevant medical history.
Our patient reported left elbow trauma one year previously, which led to poorly-defined paraesthesia in the left forearm. She was diagnosed with ulnar neuropathy secondary to elbow trauma, and received conservative treatment with infiltration analgesia administered at the medial epicondyle of the humerus, oral anti-inflammatory drugs, and lidocaine patches. In the past 3 months, she had experienced progressive weakness in the left hand; a neurophysiological study was therefore requested. The study detected a mild chronic neurogenic pattern at C5-C7, without active denervation, and a moderate-to-severe neurogenic pattern at C8-T1, with active denervation on the left side. In the light of these findings, neurological and MRI assessments were requested. The neurological examination revealed hypoaesthesia distal to the elbow with no clear dermatomal distribution and weakness of the intrinsic muscles of the left hand, with marked atrophy of the hypothenar eminence. Examination of the lower limbs revealed no alterations, with no pyramidal signs or signs of involvement of any other tract.
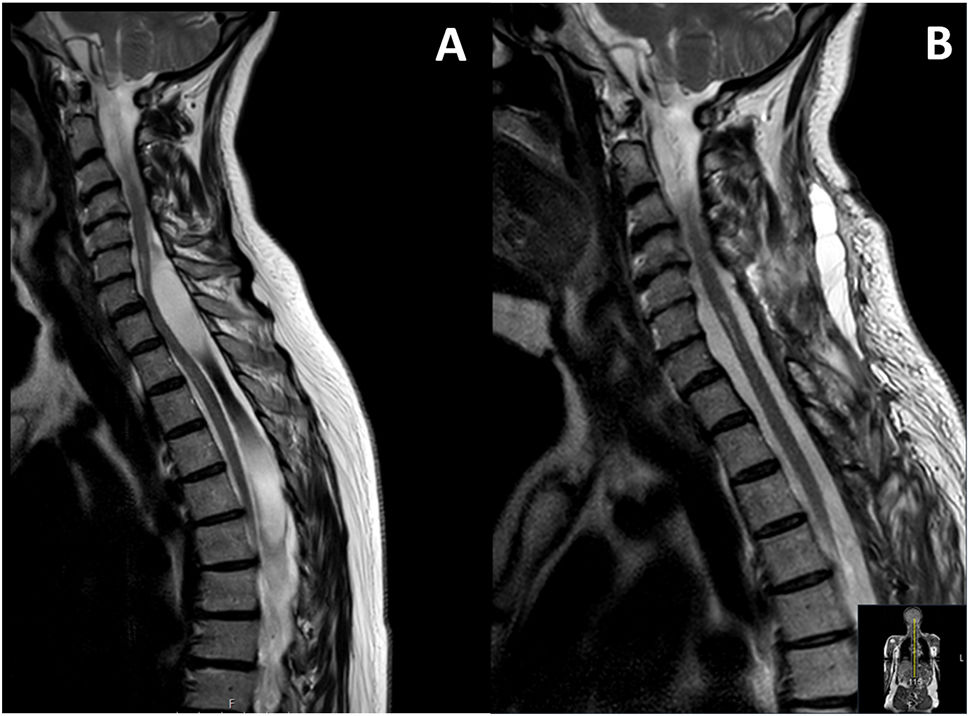
A spinal cord MRI scan (Fig. 1) revealed an intradural extramedullary lesion, with 2 cysts (one at C6-T2 and the other at T3-T6) connected by a more solid band. Compressive myelopathy was observed at the C6 level.
A) Cervical and thoracic spinal MRI scan. T2-weighted sequence showing 2 spinal arachnoid cysts. The lesion caused greater spinal cord compression at the C7-T1 level and myelopathy at C6. B) Postoperative MRI scan showing spinal cord decompression and residual myelopathy at C6-C7.
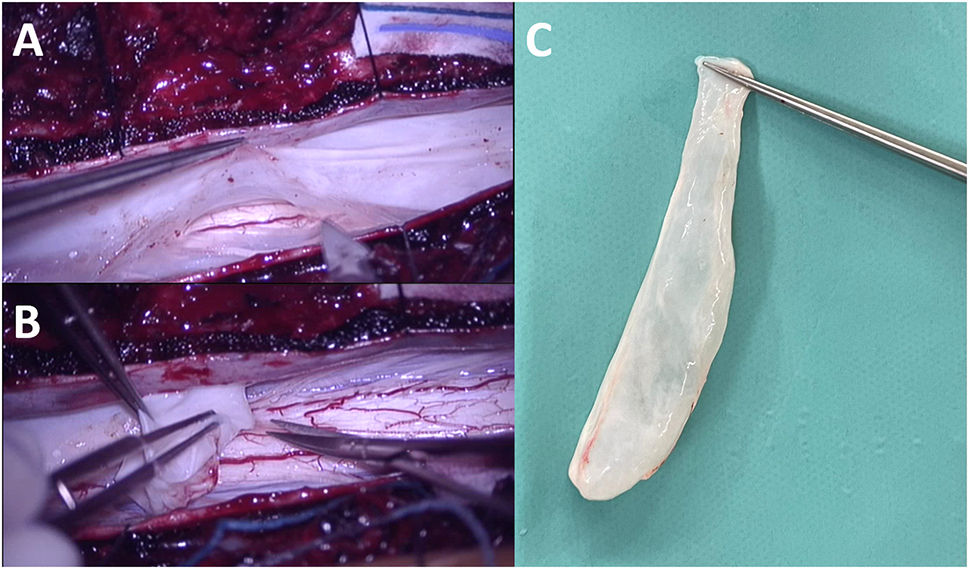
Given these clinical and radiological findings, we indicated surgical treatment. The patient underwent C6-T6 laminoplasty, with complete resection of the mass (Fig. 2). The patient progressed favourably in the postoperative period.
The anatomical pathology study of the mass revealed semitranslucent connective tissue lined by meningothelial cells, compatible with arachnoid cyst.
SACs are rare, and usually present with myelopathy or back pain. It has been suggested that they arise from diverticula in the septum posticum or from ectopic arachnoid granulations, although these hypotheses have not yet been confirmed. In most cases, the underlying cause cannot be identified, and these SACs are considered idiopathic.1,2 In some patients, SACs develop from arachnoid adhesions following trauma or as a result of inflammatory or infectious diseases. They have also been reported in the context of such invasive procedures as lumbar myelography, laminectomy, and vertebroplasty. Inflammatory adhesions within the arachnoid form arachnoid webs that may cause spinal cord compression and myelopathy. These adhesions may also form a unidirectional valve, accumulating circulating cerebrospinal fluid, leading to the formation of SACs.3,4
Idiopathic SACs in paediatric patients are mainly associated with neural tube defects.5
The typical anatomical location of SACs is the dorsal thoracic spine, with lesions frequently being intradural. Less frequently, SACs may present extradurally, in the ventral region, or in the lumbar or cervical spine. Some authors have suggested that ventral SACs constitute a specific subgroup arising from adhesive arachnoiditis following traumatic subarachnoid haemorrhage.6
The signs and symptoms of SACs are caused by their progressive expansion and chronic compression of nervous structures. Anterior or ventral cysts frequently cause weakness and myelopathy, whereas dorsal cysts more frequently cause neuropathic pain or hypoaesthesia. Some atypical symptoms include headache, in cervical SACs, and thoracic radicular pain, in thoracic SACs.2,4
MRI is the imaging technique of choice for diagnosis and follow-up of SACs, as it helps to determine the precise anatomical location of the lesion and its relationship with the spinal cord, and to detect areas of myelopathy or the degree of spinal cord atrophy. Another less frequently used technique is CT myelography, reserved for cases when MRI findings are inconclusive. Its main advantage is its ability to identify the site of communication between the SAC and the subarachnoid space, and to quantify the degree of cerebrospinal fluid circulation between the 2 compartments.3,7
Treatment for SACs is not well established. Most authors recommend complete resection of the cyst, as this strategy is associated with the lowest recurrence rate and achieves favourable neurological progression. When this is not possible, some authors suggest cyst wall fenestration, percutaneous drainage, disconnection of the cyst from the subarachnoid space, or syringopleural or cystoperitoneal shunts.1,8
Ethical standardsThe authors observed their centre’s protocols for the publication of patient data.
Conflicts of interestThe authors have no conflicts of interest to declare.