Dear Editor:
The search for new treatment options for patients with pain has led to promising advances in decreasing the necessary doses and consequently the adverse reactions of such drugs as opioids. For example, some studies have reported an association between intake of vitamin C/ascorbic acid (AA) and a decrease in pain in several diseases.
Scurvy, a disease caused by AA deficiency, is characterised by pain probably secondary to bleeding in bone and muscle tissues[1]; this pain significantly improves when adequate plasma AA levels are achieved through supplementation.[2] Bone and muscle pain in the neck and lower back and pain in inflammatory diseases such as rheumatoid arthritis have been also associated with AA deficiency; this may be explained by the vitamin’s capacity to positively or negatively regulate genes by modifying transcription factors and epigenetic marks, causing osteogenic, chondrogenic, and osteoblastogenic effects.[3]
Ascorbic acid requirements increase in postsurgical patients; different meta-analyses conclude that the administration of AA may decrease the incidence of chronic pain syndromes with oral doses of 2 g/day or intravenous doses of 50 mg/kg/day.[4] Studies have found a decrease in pain using doses below 1 g/day for 2 weeks in patients with osteoarthrosis, whereas improvements have been reported in rheumatoid arthritis with infusions administered twice a week.[5] Studies of other clinical entities, such as Paget disease, report favourable outcomes in pain after the administration of AA, probably due to its activity as a cofactor of the enzymes responsible for collagen synthesis.[3] One study including a patient with postherpetic neuralgia reports that intravenous administration of AA was associated with a decrease in pain; furthermore, in these cases, vitamin C deficiency (< 45 μmol/L) was also associated with an increased risk of neuropathic pain.[6]
Patients with cancer present higher AA requirements than the general population, and therefore higher incidence of vitamin C deficiency; pain is common in these patients, in whom nociceptive and neuropathic pain may coexist.[7] Recent studies have shown a positive impact in pain reduction, a decrease in the need for analgesic drugs, and an improvement in the quality of life of patients receiving supplementation with high doses of AA (4 g/day); a significant decrease has also been reported in pain secondary to bone metastases and in episodes of breakthrough pain in patients receiving intravenous doses of 5 g per week or oral doses of 500-4000 mg.[8]
The need for opioids after administration of AA has also been analysed on multiple occasions. Administration of doses above 1 g in oncological patients decreases the need for opioids and significantly reduces withdrawal symptoms.[9,10] In the case of postsurgical pain after oncological procedures, AA has been shown to decrease pain scores on the visual analogue scale and the total morphine dose required.[4,11]
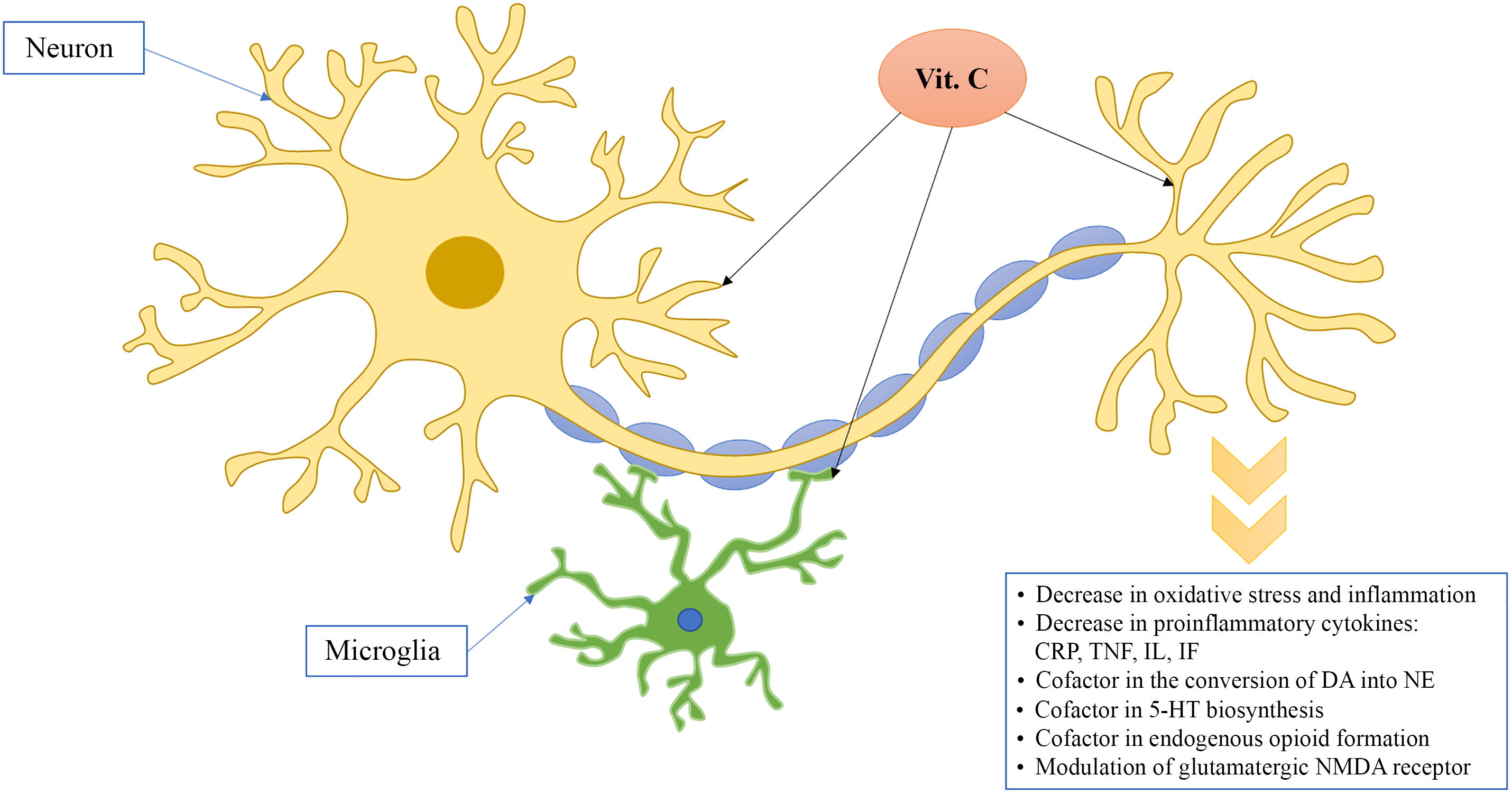
Possible explanations for the analgesic effect of AA include the decrease in oxidative stress, given its capacity to eliminate multiple reactive oxygen species, the decrease in tissue damage, and its anti-inflammatory properties due to a decrease in proinflammatory cytokines, in addition to its enzymatic participation in multiple physiological processes.[12]
AA participates as a cofactor in catecholamine synthesis, in the conversion of dopamine into norepinephrine by dopamine β-hydroxylase, and by promoting the recycling of the cofactor tetrahydrobiopterin, necessary for the activity of tyrosine hydroxylase and the synthesis of serotonin, thus favouring the modulation of ascending pain pathways and activation of descending pain inhibitory pathways.[13] Lastly, AA also participates in the synthesis of endogenous opioids and modifies NMDA receptors (Fig. 1).
According to the data from clinical trials and theoretical pharmacological associations, AA is considered an interesting option for patients with neuropathic pain, nociceptive pain of oncological origin, and postoperative pain. Further studies with larger populations and more rigorous methodologies are needed to define other indications; however, considering the low risk of complications secondary to AA supplementation, its low cost, and availability in different healthcare systems, it may be included among indications for multimodal pain management.
FundingThe authors received no funding for this study.
Conflicts of interestThe author has no conflicts of interest to declare.