SARS-CoV-2 infection may present with a wide range of neurological manifestations, including ischaemic and haemorrhagic stroke secondary to endothelial damage and a procoagulant state caused by the virus.
We report the case of a patient with COVID-19 who presented multiple strokes; the patient was a carrier of the mutation responsible for cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), which had been asymptomatic until the time of consultation.
Case reportThe patient was a 28-year-old man with no relevant history who consulted due to apathy, diarrhoea, and vomiting of 36 h progression. He had no relevant family history of neurological disease. The physical examination revealed bradyphrenia, severe dysarthria, and dysphagia for both solids and liquids. A PCR test for SARS-CoV-2 yielded positive results. During hospitalisation, HIV infection and syphilis were ruled out. The patient presented no metabolic alterations. A biochemical analysis of CSF yielded normal results.
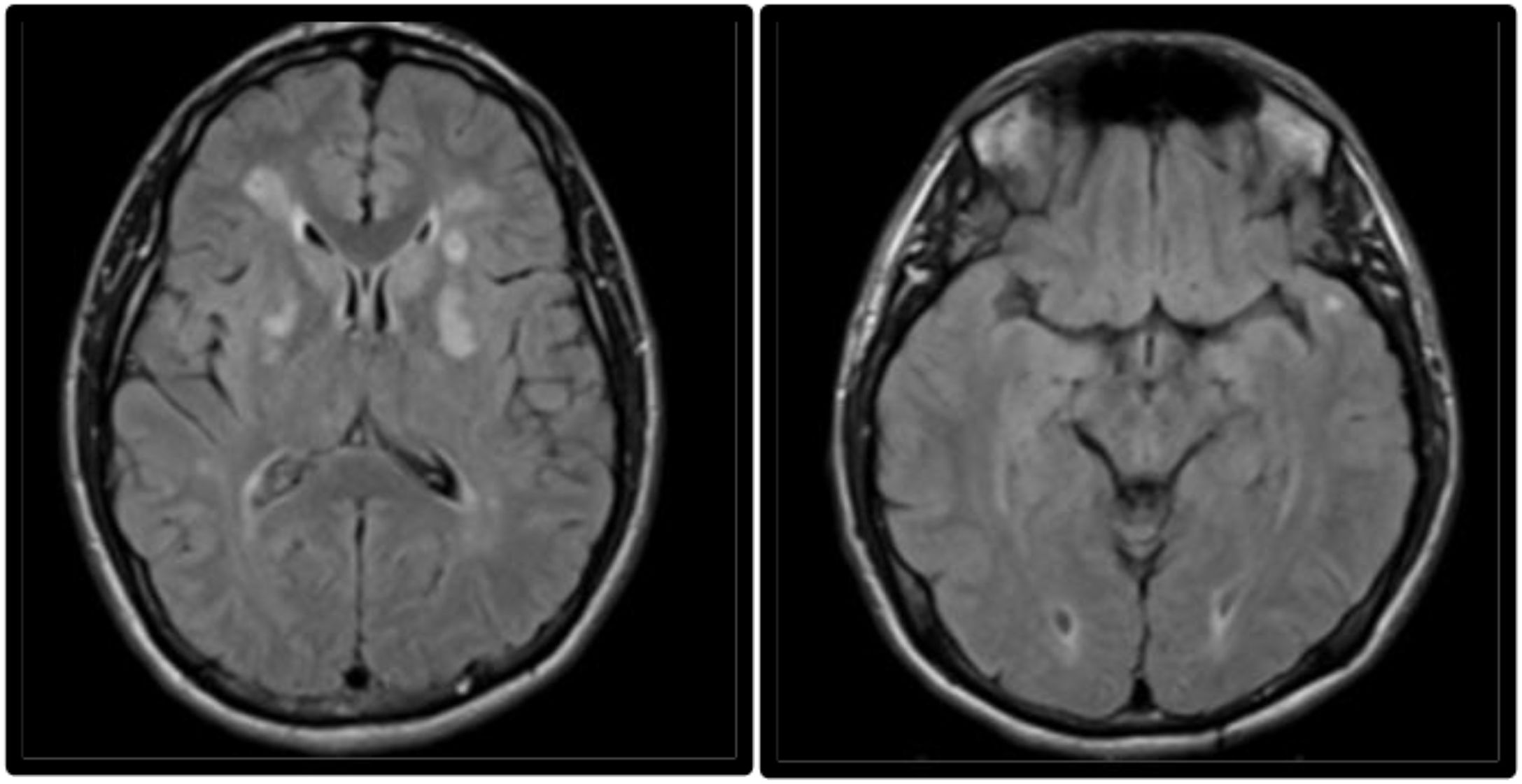
Laboratory analyses for rheumatic and haematological diseases ruled out blood clotting disorders. A contrast brain MRI scan revealed multiple subcortical lesions compatible with acute ischaemic lesions in both hemispheres, predominantly at the level of the centrum semiovale (Fig. 1). Hyperintense lesions were found in the subcortical white matter of both temporal poles (Fig. 2). CT angiography of the brain and neck detected no abnormalities. Transthoracic echocardiography with microbubbles yielded normal results. Brain angiography and positron emission tomography ruled out vasculitis. The patient received treatment with acetylsalicylic acid dosed at 100 mg/day and required feeding with a nasoduodenal tube due to dysphagia. Imaging findings were suggestive of CADASIL; sequencing of the NOTCH3 gene revealed heterozygosity for a pathogenic variant associated with the disease. The patient's neurological symptoms progressed favourably. At discharge, the patients scored 1 on the National Institutes of Health Stroke Scale due to mild dysarthria. At 3 months from symptom onset, he scored 1 point on the modified Rankin Scale.
MRI study performed 2 weeks after symptom onset. Axial non-contrast FLAIR sequence showing persistent hyperintensity of the lesions affecting both lenticular nuclei, predominantly in the left hemisphere. The image also reveals hyperintensities in the subcortical white matter of both temporal poles, a typical finding in CADASIL.
CADASIL is an autosomal dominant cerebral arteriopathy characterised by recurrent ischaemic infarcts due to small-vessel disease secondary to mutations in the NOTCH3 gene. It typically manifests with deep ischaemic and haemorrhagic infarcts in the absence of vascular risk factors, attentional cognitive impairment with a dysexecutive pattern due to subcortical damage, migraine, and psychiatric symptoms. From a radiological viewpoint, it is characterised by subcortical ischaemic lesions to the anterior temporal lobes.1
Diagnosis of CADASIL is established based on the detection of a pathogenic variant of NOTCH3 in molecular studies or the detection of typical findings in electron microscopy and immunohistochemistry studies of a skin biopsy sample.1 From an anatomical pathology viewpoint, the mutation predisposes to abnormal protein formation, with deposition of granular osmiophilic material and fibrosis in the walls of small arteries.2 These biopsy findings are not pathognomonic of CADASIL and must therefore be accompanied by clinical and radiological findings typical of the disease.
There is no specific treatment for CADASIL. The efficacy of antiplatelet drugs has not been demonstrated. Anticoagulants should be avoided, and vascular risk factors should be controlled. Systemic thrombolysis is contraindicated in these patients, and statins are not indicated in patients without cardiovascular risk factors.3 The NOTCH3 gene is mainly expressed in vascular smooth muscle cells and plays a major role in the differentiation and maturation of these cells, as well as in vessel homeostasis.4 An association has been demonstrated between SARS-CoV-2 infection and cerebrovascular events. The incidence of ischaemic stroke in hospitalised patients with SARS-CoV-2 infection is 5%.5 Cases have been reported of large-vessel occlusion, multiple infarcts, venous thromboembolism, increased levels of inflammatory markers, and presence of antiphospholipid antibodies, and stroke in young individuals.5
Our patient showed an atypical presentation of acute SARS-CoV-2 infection, as he did not present respiratory symptoms but rather encephalopathy, and was a carrier of a gene mutation known to cause CADASIL, which had previously been asymptomatic.
With this case report, we intend to call attention to the severity of neurological symptoms triggered by SARS-CoV-2 infection and the importance of prevention measures, especially vaccination, in patients with this condition.
Conflicts of interestThe authors of this study have no conflicts of interest to declare.
Ethical considerationsThe authors observed their centre's protocols for the publication of patient data. The patient gave informed consent for the publication of this case report.