SARS-CoV-2 infection is an emerging disease that represents a threat to life globally, with more than 179 million confirmed cases and 3 million deaths. In Colombia, where almost 5 million infections and approximately 127 thousand deaths have been reported, it presents a wide variety of neurological manifestations that range from mild to severe symptoms.
ObjectiveThis study describes the characteristics of neurological manifestations in patients with COVID-19 in the period March–September 2020 at a tertiary hospital in Bogota.
MethodsWe performed a cross-sectional descriptive study. We selected patients by non-probability sampling, including all patients attended by the neurology service at our hospital. We included all patients with infection confirmed by RT-PCR test and neurological disease confirmed by tomography, study of cerebrospinal fluid, and clinical manifestations reported in the medical history. We excluded epileptic patients who presented seizures as the only clinical manifestation.
ResultsIn a total of 58 patients, the mean age was 58 years, with 60.3% of patients being men; 65.5% were alert at admission. The main neurological symptom was brain ischaemia, in 36.2%, followed by seizures, in 25.9%. Arterial hypertension was observed in 58.6%. We observed no alterations in the cerebrospinal fluid; the mean hospital stay was 35 days, and 41.4% of patients died.
ConclusionsSARS-CoV-2 infection not only affects the respiratory system, but can also cause a range of neurological manifestations ranging from mild symptoms such as headache, dysgeusia, and anosmia to severe complications such as seizures, brain ischaemia/haemorrhage, encephalopathy, or death.
La infección por SARS-CoV2 es una enfermedad emergente que representa un peligro para la vida a nivel mundial, con más de 179 millones de casos confirmados y 3 millones de muertes. En Colombia, se han reportado casi 5 millones de personas contagiadas y alrededor de 127 mil fallecidos, presenta una amplia variedad de manifestaciones neurológicas que van desde leves a severas.
ObjetivoDescribir las características de las manifestaciones neurológicas en pacientes con infección por coronavirus SARS-CoV2 (Covid19) en el periodo marzo – septiembre de 2020 en un Hospital de 3er nivel en Bogotá.
MetodologíaSe trata de un estudio descriptivo tipo corte transversal. Se realizó un muestreo no probabilístico en el que se incluyeron todos los casos atendidos por el servicio de neurología de la institución seleccionada, se incluyeron todos los pacientes con infección confirmada por prueba de RT-PCR y aquellos con enfermedad neurológica documentada por tomografía, estudio de líquido cefalorraquídeo o manifestaciones clínicas registradas en la historia clínica. Fueron excluidos los pacientes epilépticos quienes presenten convulsiones como única manifestación clínica.
ResultadosEn un total de 58 pacientes, se encontró media de edad de 58 años, con un 60,3% correspondiente al sexo masculino, 65,5% estuvieron alerta, la principal manifestación neurológica fue la isquemia cerebral en un 36,2%, seguida de convulsiones con un 25,9%. La hipertensión arterial estuvo en el 58,6%. No hubo alteraciones en el LCR, el promedio de estancia hospitalaria fue de 35 días y el 41,4% fallecieron.
ConclusionesLa infección por SARS-CoV2 condiciona no solo una afección al sistema respiratorio, sino que presenta un amplio espectro de manifestaciones neurológicas que van desde las más leves como cefalea, disgeusia y anosmia, hasta las más graves como convulsiones, isquemia/sangrado cerebral, encefalopatía o muerte.
In March 2020, COVID-19 was declared a pandemic; this is a global life-threatening disease with more than 230 million confirmed cases and 4.8 million deaths.1 In Colombia, almost 5 million infections and approximately 127 thousand deaths have been reported; Bogota is the city with the highest number of cases reported to date.2 Approximately 80% of hospitalised patients have presented neurological symptoms during the infection,3 including less frequent symptoms as anosmia and dysgeusia that may manifest in the absence of nasal congestion or secretion but are associated with a severe cognitive or cardiorespiratory dysfunction4 (and of slow resolution: olfactory function may take up to 4–8 months to fully recover)5; and severe neurological symptoms such as altered level of consciousness, hallucinations, or psychomotor agitation.6 The most prevalent neurological symptoms are myalgia, headache, encephalopathy, and vertigo.4 To date, no Colombian study has addressed patients with COVID-19 and neurological symptoms, although it represents a considerable healthcare emergency, giving rise to the need for scientific articles to improve our understanding of the condition in order to provide better care to patients.
MethodsWe conducted a cross-sectional descriptive study. Our aim was to describe the characteristics of neurological symptoms in patients with COVID-19 from March to September 2020 at a tertiary hospital in Bogota. We used data from patients attended by the neurology department, extracted from the Colombian SERVINTE system.
We selected patients by non-probability sampling of all patients attended at our hospital’s neurology department. Qualitative variables are expressed as absolute and relative frequencies; quantitative variables are expressed with measures of central tendency and dispersion selected according to normality of distribution (Shapiro–Wilk test).
We describe the inclusion and exclusion criteria below.
- 1.
Inclusion criteria
- •
Confirmed infection with SARS-CoV-2 by RT-PCR testing.
- •
Neurological symptoms confirmed by computed tomography, cerebrospinal fluid (CSF) study, or clinical manifestations reported in the medical history.
- •
Age 18 years or older.
- 2.
Exclusion criteria
- •
Epileptic patients presenting seizures as the sole clinical manifestation.
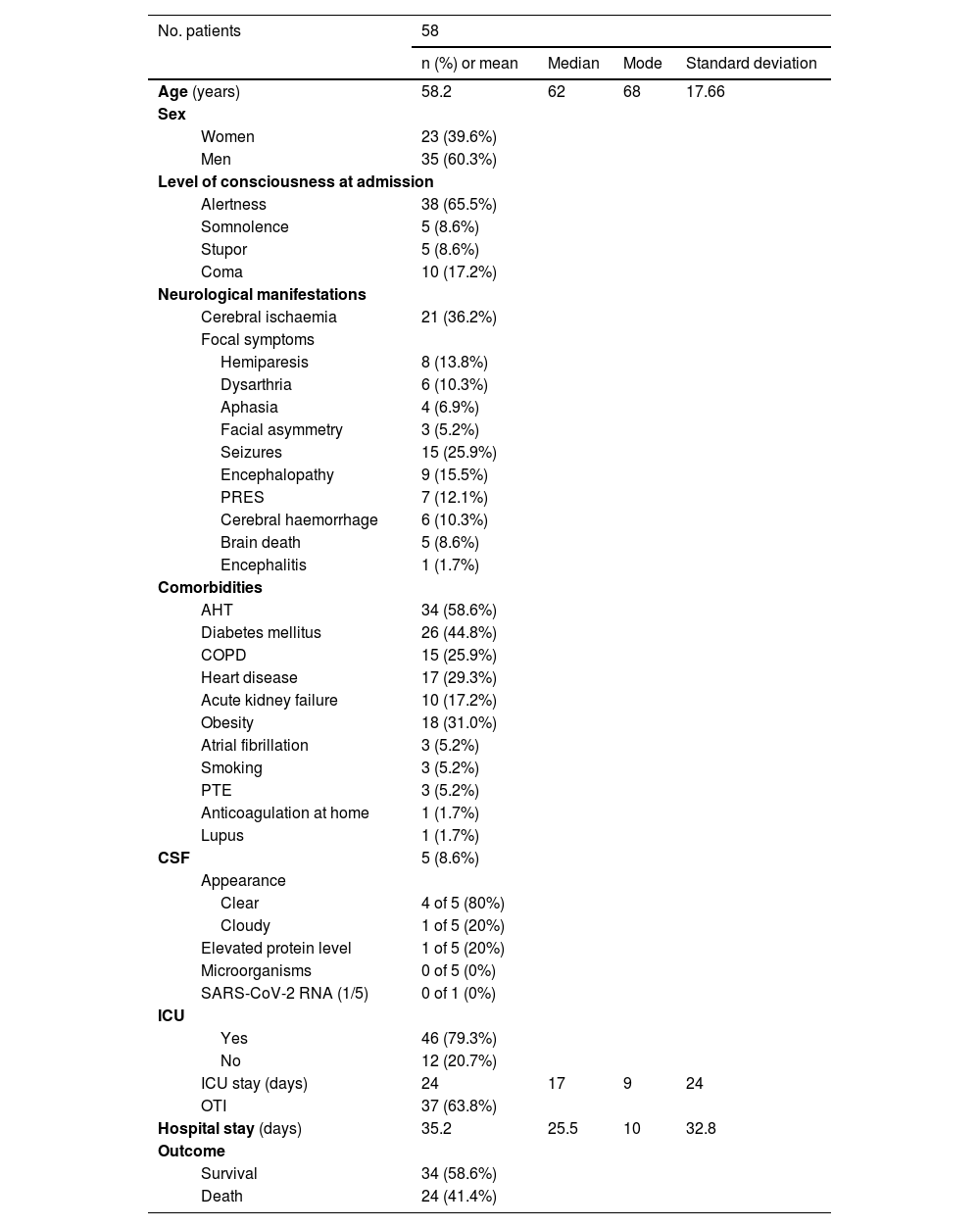
We analysed data from 58 patients attended by the neurology department and presenting neurological symptoms and RT–PCR-confirmed SARS-CoV-2 infection. Mean age [standard deviation (SD)] was 58 years (17.6), with 60.3% being men. Most patients were fully alert at admission (65.5%), with coma being the second most prevalent state (17.2%). The most frequent neurological symptom was brain ischaemia, observed in 36.2% of patients and accompanied by such focal symptoms as hemiparesis (in 8 patients), dysarthria,6 aphasia,4 and facial asymmetry.3 Other symptoms were seizures (25.9%), encephalopathy (15.5%), posterior reversible encephalopathy syndrome (12.1%), brain haemorrhage (10.3%), brain death (8.6%), and encephalitis (1.7%) (Table 1).
Clinical characteristics of our sample.
| No. patients | 58 | ||||
|---|---|---|---|---|---|
| n (%) or mean | Median | Mode | Standard deviation | ||
| Age (years) | 58.2 | 62 | 68 | 17.66 | |
| Sex | |||||
| Women | 23 (39.6%) | ||||
| Men | 35 (60.3%) | ||||
| Level of consciousness at admission | |||||
| Alertness | 38 (65.5%) | ||||
| Somnolence | 5 (8.6%) | ||||
| Stupor | 5 (8.6%) | ||||
| Coma | 10 (17.2%) | ||||
| Neurological manifestations | |||||
| Cerebral ischaemia | 21 (36.2%) | ||||
| Focal symptoms | |||||
| Hemiparesis | 8 (13.8%) | ||||
| Dysarthria | 6 (10.3%) | ||||
| Aphasia | 4 (6.9%) | ||||
| Facial asymmetry | 3 (5.2%) | ||||
| Seizures | 15 (25.9%) | ||||
| Encephalopathy | 9 (15.5%) | ||||
| PRES | 7 (12.1%) | ||||
| Cerebral haemorrhage | 6 (10.3%) | ||||
| Brain death | 5 (8.6%) | ||||
| Encephalitis | 1 (1.7%) | ||||
| Comorbidities | |||||
| AHT | 34 (58.6%) | ||||
| Diabetes mellitus | 26 (44.8%) | ||||
| COPD | 15 (25.9%) | ||||
| Heart disease | 17 (29.3%) | ||||
| Acute kidney failure | 10 (17.2%) | ||||
| Obesity | 18 (31.0%) | ||||
| Atrial fibrillation | 3 (5.2%) | ||||
| Smoking | 3 (5.2%) | ||||
| PTE | 3 (5.2%) | ||||
| Anticoagulation at home | 1 (1.7%) | ||||
| Lupus | 1 (1.7%) | ||||
| CSF | 5 (8.6%) | ||||
| Appearance | |||||
| Clear | 4 of 5 (80%) | ||||
| Cloudy | 1 of 5 (20%) | ||||
| Elevated protein level | 1 of 5 (20%) | ||||
| Microorganisms | 0 of 5 (0%) | ||||
| SARS-CoV-2 RNA (1/5) | 0 of 1 (0%) | ||||
| ICU | |||||
| Yes | 46 (79.3%) | ||||
| No | 12 (20.7%) | ||||
| ICU stay (days) | 24 | 17 | 9 | 24 | |
| OTI | 37 (63.8%) | ||||
| Hospital stay (days) | 35.2 | 25.5 | 10 | 32.8 | |
| Outcome | |||||
| Survival | 34 (58.6%) | ||||
| Death | 24 (41.4%) | ||||
AHT: arterial hypertension; COPD: chronic obstructive pulmonary disease; CSF: cerebrospinal fluid; ICU: intensive care unit; OTI: orotracheal intubation; PRES: posterior reversible encephalopathy syndrome; PTE: pulmonary thromboembolism; RNA: ribonucleic acid.
Among the associated comorbidities, arterial hypertension was present in 58.6% of patients, followed by diabetes mellitus (44.8%), obesity (31%), heart disease (29.3%), chronic obstructive pulmonary disease (25.9%), and acute kidney failure (17.2%). We also observed lower numbers of patients with history of pulmonary thromboembolism, atrial fibrillation, and smoking; one patient was being treated with anticoagulant drugs at home and another had systemic lupus erythematosus (Table 1).
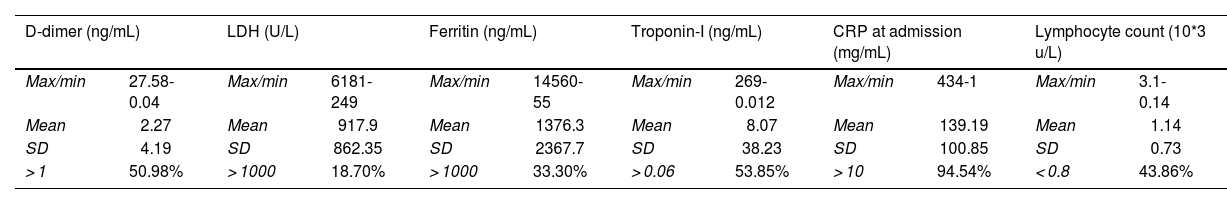
The severity markers most frequently observed at elevated levels were C-reactive protein (CRP), followed by troponin I, and D-dimer, in more than 50% of patients (Table 2). The least frequently altered severity marker was lactate dehydrogenase (LDH), followed by ferritin and lymphocyte count (Table 2). We calculated the standard deviation for each of the markers assessed, and found larger deviations and wider ranges for ferritin, LDH, and CRP, and smaller deviations and narrower ranges for lymphocyte count, troponin I, and D-dimer (Table 2).
Severity markers.
| D-dimer (ng/mL) | LDH (U/L) | Ferritin (ng/mL) | Troponin-I (ng/mL) | CRP at admission (mg/mL) | Lymphocyte count (10*3 u/L) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Max/min | 27.58-0.04 | Max/min | 6181-249 | Max/min | 14560-55 | Max/min | 269-0.012 | Max/min | 434-1 | Max/min | 3.1-0.14 |
| Mean | 2.27 | Mean | 917.9 | Mean | 1376.3 | Mean | 8.07 | Mean | 139.19 | Mean | 1.14 |
| SD | 4.19 | SD | 862.35 | SD | 2367.7 | SD | 38.23 | SD | 100.85 | SD | 0.73 |
| > 1 | 50.98% | > 1000 | 18.70% | > 1000 | 33.30% | > 0.06 | 53.85% | > 10 | 94.54% | < 0.8 | 43.86% |
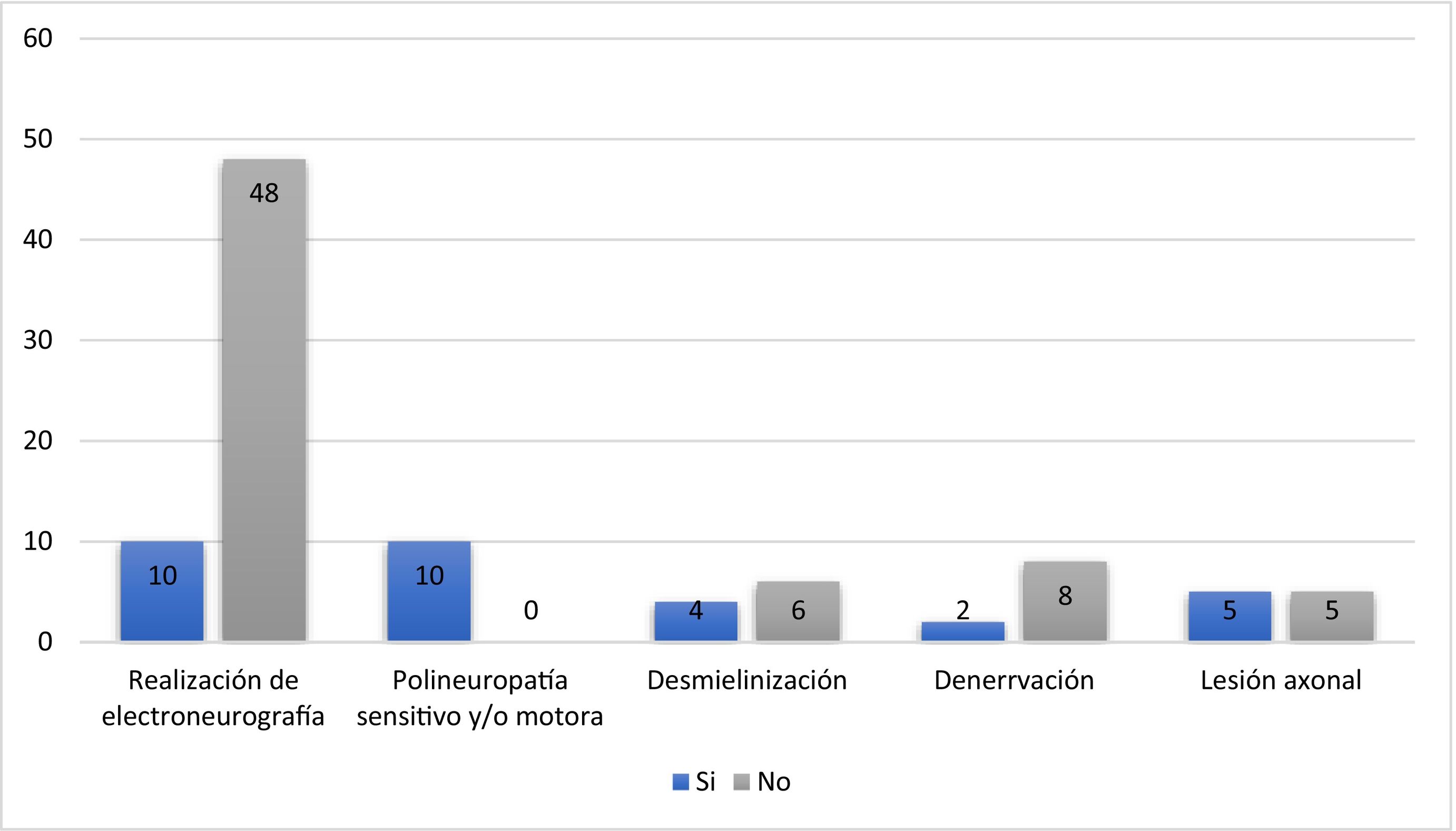
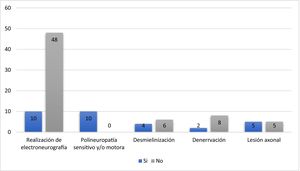
Lumbar punctures performed in five patients revealed clear CSF and glucose level within the normal range in four patients (80%), of whom two presented increased protein levels and the other two presented increased leukocyte count [one with increased percentage of lymphocytes (97%)]; one patient presented cloudy CSF. No microorganisms were detected in the CSF; PCR testing for SARS-CoV-2 in the CSF in one patient yielded negative results (Table 1). Electroneuromyography studies performed in 10 patients revealed sensory or motor polyneuropathy in all cases, with findings compatible with demyelination in 4 patients, denervation in 2, and axonal lesions in 5 (Fig. 1). (See Fig. 2.)
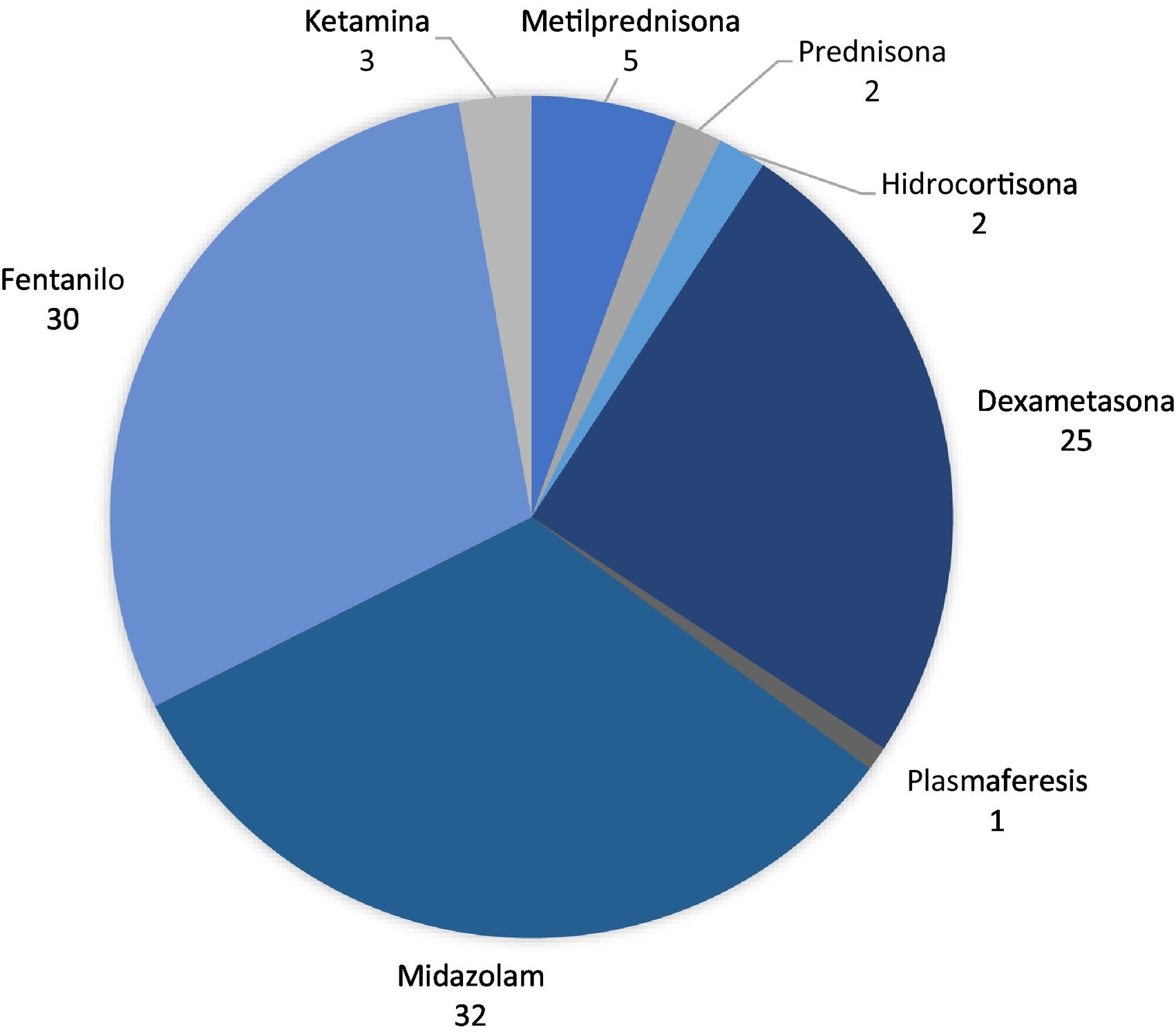
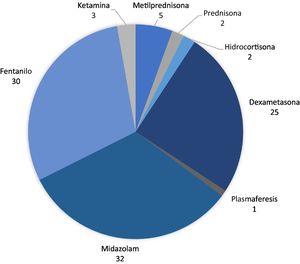
The main drug used to treat the clinical complications and manifestations was midazolam (in 35 patients), followed by fentanyl (32); corticosteroids were used in 37 patients, as follows: dexamethasone in 27, methylprednisolone in 6, hydrocortisone in 2, and prednisone in 2. Only one patient received plasmapheresis.
In addition to neurological symptoms, 52 patients (89.6%) presented imaging-confirmed pulmonary alterations. The mean hospital stay was 35 days; 79.3% of patients were admitted to the intensive care unit, with a mean stay of 12 days; orotracheal intubation was required in 63.8% of patients. Twenty-four patients (41.4%) died (Table 1).
DiscussionTo facilitate the discussion, the neurological manifestations described above are classified into the following categories.
EpidemiologyOur study showed that most patients with SARS-CoV-2 infection and neurological symptoms were men7; this finding is consistent with the current literature. The mean age of the patients was 58 years; recent research has found that the population aged around 50 years is more susceptible to the disease, with an increased risk of complications in patients older than 60 years and presenting associated comorbidities.8
Comorbid diseases in our sample included arterial hypertension, which was present in more than 50% of patients, followed by diabetes mellitus and chronic obstructive pulmonary disease. A study conducted in Wuhan found that arterial hypertension was one of the most frequent comorbidities associated with COVID-19, followed by diabetes and coronary disease.9
It is important to highlight that CSF PCR testing for SARS-CoV-2 was not routinely performed in patients undergoing lumbar puncture, as no clear association with high diagnostic specificity and sensitivity had been established at the time. This is also a costly test for a public hospital.
Clinical manifestationsAt admission, most patients were alert, and brain ischaemia was the most frequent complication of SARS-CoV-2 infection, followed by seizures. This infection has been shown to increase the risk of stroke.10
A Spanish study including a sample of 841 patients with confirmed SARS-CoV-2 infection reported that more than half of the patients developed some type of neurological symptom.11 Some presented non-specific symptoms such as myalgia or headache in the early stages of the disease, whereas such other alterations as anosmia and dysgeusia, which took longer to resolve, were associated with less severe cases; altered level of consciousness was less frequently reported.11
Another study found that 88% of the 100 hospitalised patients presented some neurological complaint potentially associated with SARS-CoV-2 infection, with the most frequent being anosmia, dysgeusia, and headache; less frequent symptoms included encephalopathy, seizures, and syncope. The study also reported two cases of ischaemic stroke.12
A Colombian study conducted by a group of neurosurgeons in Bogota showed that the most frequent symptoms were asthaenia or adynamia, followed by cough and headache, with the latter being the main neurological manifestation. The main symptom associated with cranial nerve involvement was anosmia.13
We found no significant alterations in CSF studies conducted in our sample. Among the main findings described in the literature are increased protein levels,14 but in our sample only one patient undergoing lumbar puncture showed elevated proteins. We should stress that CSF analysis was not performed in the majority of patients.
Regarding severity markers, elevated levels of CRP, troponin I, and D-dimer were observed in more than 50% of patients; this finding has been associated with the inflammatory pathophysiology of COVID-19,9 and the high level of respiratory distress it causes. We did not consider this in our analysis of the association with the neurological symptoms recorded.
The main alteration identified in electroneuromyography studies was sensorimotor polyneuropathy, with axonal injury observed in half of these patients. Multiple cases have been reported of polyneuropathy after SARS-CoV-2 infection, which may be related to the immune response and the release of multiple proinflammatory cytokines that cause the axonal injury15; cases of Guillain-Barré syndrome have also been reported in association with the infection.16
It is important to stress that cranial nerve involvement has been common in general, although the most frequently described symptoms are olfactory and gustatory nerve involvement; several cases have also been reported of cranial nerve dysfunction.17 One study reported the cases of two patients with confirmed SARS-CoV-2 infection presenting acute peripheral polyneuropathy accompanied by cranial neuropathy, which was finally diagnosed as Miller-Fisher syndrome.18
Patients were hospitalised for more than one month, with 80% requiring admission to the intensive care unit; 24 patients died. Current evidence suggests that in patients with more severe infections and older age, neurological complications explain 4% of deaths.11
Management of hospitalised patients with SARS-CoV-2In our study, we found that the main medication used for the management of these patients was midazolam, followed by fentanyl, whereas 37 patients received glucocorticoids, and only one received plasmapheresis. Our literature search identified a report of three patients with myoclonus associated with SARS-CoV-2 infection; two of these patients were treated with short cycles of high-dose methylprednisolone and the remaining patient received plasmapheresis, which improved symptoms.19
We also found reports of patients with SARS-CoV-2 infection and generalised seizures treated with such anticonvulsant drugs as levetiracetam, together with symptoms compatible with parainfectious encephalitis associated with SARS-CoV-2 infection treated with immunoglobulins and high-dose methylprednisolone, which improved clinical symptoms and the lesions observed in neuroimaging.20
This study illustrates the great variety of symptoms that may be clinically related to SARS-CoV-2 infection, as well as the wide range of associated neurological manifestations, ranging from mild alterations to severe symptoms that may lead to severe disability or death.
We should mention that we did not analyse the use of experimental drugs or medications for which little scientific evidence is available on the treatment of this new virus. However, clinical histories do provide data for a more extensive future study to measure variables associated with the use of such drugs, the severity of the disease, and its association with neurological manifestations.
Conclusions- •
The neurological manifestations associated with SARS-CoV-2 infection may severely affect patients’ functional status, such as ischaemic or haemorrhagic events or polyneuropathies requiring prolonged comprehensive rehabilitation, increasing costs for the healthcare system.
- •
COVID-19 is associated with a high mortality rate, and it is important to know the possible treatments available to improve these symptoms and help patients to recover quicker with fewer sequelae.
- •
As this is a new disease, with new clinical findings emerging every day, it is necessary to expand our scientific knowledge; this study paves the way for larger studies to analyse associations not addressed in this study.
The authors have no conflicts of interest to declare.
Publication ethicsThis study complies with the principles of the Declaration of Helsinki on medical research involving human subjects (updated at the 64th World Medical Association General Assembly in Fortaleza [Brazil] in October 2013).
The study also complied with the local regulations of the Colombian Ministry of Health, Regulation 8430, of 1993, chapter I “On the ethical aspects of research involving human subjects”.
This study is classified within the “no risk” category. No patient consent was required, and the study was approved by our hospital’s research ethics committee.
All members of the research team will provide information on the study to any organisation with academic or scientific interest in the study, preserving the accuracy of the results and making references to general data and not individual patients or institutions.
Absolute confidentiality will be maintained, as well as the good standing of the professional institution.
Sources of fundingAuthors’ own funding.