Acute vestibular syndrome may seem intimidating due to the large overlap of symptoms between vestibular and non-vestibular causes, including serious and benign causes. In addition, there is no diagnostic method to differentiate between central and peripheral causes early.
ObjectiveThis study aimed to evaluate the sensitivity and specificity of the ocular movements test (HINTS) in the detection of central acute vestibular syndrome.
Materials and methodsA prospective cross-sectional study was conducted, which included (n=58) patients admitted with a complaint of acute vestibular syndrome to Tishreen University Hospital in Latakia during the period from April 14, 2021 to July 1, 2022. Patients with acute vestibular syndrome (according to the definition of the International Classification of Vestibular Disorders) who were admitted to the hospital and who had at least one risk factor for stroke were included. Patients with a history of recurrent vertigo, those with diseases that would preclude HINTS testing, such as cervical or ocular diseases, and those for whom MRI was contraindicated were excluded. HINTS testing and brain CT were performed on admission. A brain MRI was performed 48 h after the onset of symptoms. The central lesion was diagnosed with a positive CT scan or MRI.
ResultsOut of the 58 patients, 23 were diagnosed with a central lesion and 35 with a peripheral lesion. We found that in patients with a central lesion, with ischemic stroke being the most common cause. Cerebellar infarction was the most common, with a rate of 34.78%. We found bulbar infarction in 5 patients with a rate of 21.74%, pontine infarction in 4 with a rate of 17.39%, cerebellar metastasis in 3 with a rate of 13.04%, cerebellar peduncle infarction in 2 with a rate of 8.70%, and cerebellar hemorrhage in 1 with a rate of 4.35%. The HINTS test was positive (i.e., indicated a central lesion) in 22 patients with a central lesion and negative (i.e., indicated a peripheral lesion) in 33 patients with a peripheral lesion. Thus, the sensitivity of the HINTS test in detecting central acute vestibular syndrome was found to be 95.65%, and its specificity was 94.29%.
ConclusionThe HINTS test is a simple and cost-effective clinical tool that can be used to accurately diagnose central acute vestibular syndrome.
El síndrome vestibular agudo puede parecer intimidante debido a la gran superposición de síntomas entre causas vestibulares y no vestibulares, incluyendo causas graves y benignas. Además de la falta de un método diagnóstico que permita diferenciar precozmente entre causas centrales y periféricas,
ObjetivoEste estudio tuvo como objetivo evaluar la sensibilidad y especificidad del test de movimientos oculares (HINTS) en la detección del síndrome vestibular agudo central.
Materiales y métodosSe realizó un estudio transversal prospectivo que incluyó (n = 58) pacientes ingresados con una queja de síndrome vestibular agudo en el Hospital Universitario Tishreen de Latakia durante el período comprendido entre el 14 de abril de 2021 y el 1 de julio de 2022. Se incluyeron los pacientes con síndrome vestibular agudo (según la definición de la Clasificación Internacional de Trastornos Vestibulares) que ingresaron en el hospital y que tenían al menos un factor de riesgo de accidente cerebrovascular. Se excluyeron los pacientes con antecedentes de vértigo recurrente, aquellos con enfermedades que impedirían la realización de pruebas HINTS, como enfermedades cervicales u oculares, y aquellos para los que la RM estaba contraindicada. Las pruebas HINTS y el TAC cerebral se realizaron al ingreso. Se realizó una RM cerebral 48 horas después del inicio de los síntomas. La lesión central se diagnosticó con una TC o RM positiva.
ResultadosDe los 58 pacientes, 23 fueron diagnosticados de lesión central y 35 de lesión periférica. Encontramos que, en los pacientes con una lesión central, siendo el ictus isquémico la causa más frecuente. El infarto cerebeloso fue el más frecuente, con una tasa del 34,78%. Encontramos infarto bulbar en 5 pacientes con una tasa del 21,74%, infarto pontino en 4 con una tasa del 17,39%, metástasis cerebelosa en 3 con una tasa del 13,04%, infarto del pedúnculo cerebeloso en 2 con una tasa del 8,70% y hemorragia cerebelosa en 1 con una tasa del 4,35%. La prueba HINTS fue positiva (es decir, indicó una lesión central) en 22 pacientes con una lesión central y negativa (es decir, indicó una lesión periférica) en 33 pacientes con una lesión periférica. Así pues, la sensibilidad de la prueba HINTS para detectar el síndrome vestibular agudo central fue del 95,65%, y su especificidad, del 94,29%.
ConclusionesLa prueba HINTS es una herramienta clínica sencilla y rentable que puede utilizarse para diagnosticar con precisión el síndrome vestibular agudo central.
Dizziness is a common emergency complaint in the United States, accounting for 3.3%–4.4% of cases (approximately 4.4 million cases) annually.1 A study showed that 19.7% of emergency department dizzy patients had acute vestibular syndrome (AVS), and 25.4% of these AVS patients had a stroke. 69.9% of all dizziness patients received neuroimaging in the emergency department (MRI 58.2%, CT 11.6%).2 The economic cost of dizziness patients in the United States is estimated to be 10 billion dollars annually. This cost is mainly attributed to brain imaging, which is performed on approximately half of patients, and admission of 20% of patients.1
To reduce this cost without increasing the risk of missing a potentially life-threatening stroke, several studies have suggested searching for tests that can effectively diagnose central acute vestibular syndrome.1
One promising algorithm for evaluating patients with acute vestibular syndrome, especially in emergency departments, is the HINTS test. Multiple studies have found that this test has high sensitivity and specificity in diagnosing central acute vestibular syndrome.3–7
Study importanceAcute vestibular syndrome is a condition that can be challenging to diagnose due to the similarities between vestibular and non-vestibular causes, including both serious and benign causes. Although this condition is usually benign, stroke should be considered in everyone with acute vestibular syndrome since it could be indicative of vertebrobasilar disease, a larger preventable stroke, or impending cerebellar herniation.
Stroke is common enough and variable enough in presentation. It is worth noting that stroke can present similarly to vestibular neuritis, which is a more common condition.8 However, about two-thirds of stroke patients do not show focal neurological signs that are detectable by non-neurologists, and the same is true for one-third of patients examined by neurologists.9 The National Institutes of Health Stroke Scale (NIHSS) neglects many of the debilitating aspects of posterior circulation stroke, including dizziness, and can completely fail to detect posterior circulation stroke.8
Magnetic resonance imaging, including diffusion-weighted imaging, can also fail to detect ischemic stroke in the posterior fossa for up to 48 h after symptom onset. False negative increases as the period between the onset of symptoms and the MRI is short, which may prevent patients from receiving timely treatment with thrombolytics or catheter thrombectomy, which should be administered within hours after symptom onset, especially since this type of stroke, if not treated, has important consequences for the patient.10–14 Moreover, MRIs are often not available in emergencies.
Therefore, there is a need for tests that can diagnose central lesions early with high sensitivity and specificity. The HINTS test is a simple clinical test that can be performed within minutes and without cost, making it particularly important for diagnosing acute vestibular syndrome and identifying patients who may require urgent treatment.
Study objectivesThe study aims to determine the sensitivity and specificity of the Horizontal Head Impulse, Nystagmus, and Skew Deviation Test (HINTS) in detecting Central Acute Vestibular Syndrome and to determine the sensitivity and specificity of each test separately.
Research materials and methodsStudy designA prospective observational descriptive cross-sectional study was conducted at Tishreen University Hospital in Latakia, Syria, from April 14, 2021 to July 1, 2022.
The sampleInclusion criteriaPatients with acute vestibular syndrome, as defined by the International Classification of Vestibular Disorders, who were admitted to the hospital and had at least one risk factor for stroke, including smoking, hypertension, diabetes mellitus, hyperlipidemia and cholesterolemia, atrial fibrillation, hypercoagulable states, or a history of stroke or myocardial infarction.
Exclusion criteria- •
Patients with a history of recurrent dizziness.
- •
Patients who have diseases that prevent the performance of the HINTS test, such as cervical and ocular diseases.
- •
Patients for whom MRI is contraindicated.
Patients were entered according to inclusion and exclusion criteria and a detailed clinical history was taken, including age, sex, and vascular risk factors. A general clinical examination and complete neurological examination were performed on admission. HINTS testing was performed upon admission. A CT scan of the brain was performed on admission for all patients. A brain MRI was performed 48 h after the onset of symptoms for all patients except those diagnosed by CT. A daily neurological examination was performed and when any new symptoms developed.
The findings of the HINTS test were adopted to differentiate between central and peripheral lesions as follows8:
Horizontal head impulse test: It is considered positive if there is a rapid eye movement to catch the target.
- •
Its positivity indicates a peripheral lesion.
- •
Its negativity indicates a central lesion.
Nystagmus test:
- •
Gaze-evoked horizontal direction-changing nystagmus, pure vertical nystagmus, and pure torsional nystagmus indicate a central lesion.
- •
Unidirectional horizontal spontaneous nystagmus is indicative of a peripheral lesion.
Skew deviation test:
- •
The presence of skew deviation indicates a central lesion.
The HINTS test is considered positive (i.e., indicates a central lesion) if any of the previous three tests are indicative of a central lesion. The HINTS test is considered negative (i.e., indicates a peripheral lesion) when all 3 tests are indicative of a peripheral lesion.
A central lesion is diagnosed by a positive CT scan on admission or a positive MRI performed 48 h after the onset of symptoms.
The diagnosis of peripheral lesion was made by a negative repeated neurological examination and negative magnetic resonance imaging performed 48 h later, and clinical improvement.
Statistical analysisThe baseline characteristics of the study population were summarized using descriptive statistics. We used a t-test, chi-square test, or Fisher's exact test to compare the baseline characteristics of central acute vestibular syndrome patients vs. peripheral acute vestibular syndrome patients. Two-sided tests were used and p values <.05 were considered statistically significant. All analyses were done in SPSS statistical software version 20.0.0.0.
ResultsThe study included (n=58) patients with acute vestibular syndrome admitted to Tishreen University Hospital between April 14, 2021 and July 1, 2022. The number of patients of male patients was 25 (43.10%) and the number of patients of female patients was 33 (56.90%). The patients' ages ranged from 27 to 85 years, and the mean age was 60.15±14.1 years.
The study of vascular risk factors showed that hypertension was the most common risk factor at a rate of 60.34% and that the presence of a hypercoagulable state was the least common risk factor at a rate of 1.72%, as shown in Table 1 (See Fig. 1).
Prevalence of vascular risk factors in patients with acute vestibular syndrome.
| Vascular risk factor | Number of patients | Rate |
|---|---|---|
| Hypertension | 35 | 60.34% |
| Smoking | 24 | 41.38% |
| Diabetes mellitus | 24 | 41.38% |
| Prior stroke | 14 | 29.31% |
| Prior myocardial infarction | 7 | 12.07% |
| Hyperlipidemia and hypercholesterolemia | 6 | 10.34% |
| Atrial fibrillation | 5 | 8.62% |
| Hypercoagulable state | 1 | 1.72% |
A brain CT was performed on admission for all patients, and a brain MRI was performed 48 h after the onset of symptoms for all patients except one patient who was diagnosed with a cerebellar hemorrhage by CT. The study found that 23 patients (39.66%) had central acute vestibular syndrome, while 35 patients (60.34%) had peripheral acute vestibular syndrome. Among patients with central acute vestibular syndrome, it was found that cerebellar infarction was the most common diagnosis at a rate of 34.78%, while cerebellar hemorrhage was the least common diagnosis at a rate of 4.35%, as shown in Fig. 2.
Clinical examination of patients with peripheral acute vestibular syndrome showed that peripheral vestibulopathy affected the right side in 22 patients (62.86%) and the left side in 13 patients (37.14%).
Acute vestibular syndrome was accompanied by a group of symptoms, the most common of which was headache, at a rate of 29.31%, as shown in Table 2.
Clinical examination of patients showed that the Romberg sign was the most common sign seen in patients with acute vestibular syndrome (60.34%), while 2 patients did not show significant clinical findings (3.45%), as shown in Table 3.
Results of clinical examination findings in patients with acute vestibular syndrome.
| Clinical sign | Number of patients | Rate |
|---|---|---|
| Romberg sign | 35 | 60.34% |
| Ataxia | 17 | 29.31% |
| Positive finger to nose test | 12 | 20.69% |
| Facial hemisensory loss | 6 | 10.34% |
| Body hemisensory loss | 6 | 10.34% |
| Peripheral facial palsy | 4 | 6.90% |
| Diminished gag reflex | 4 | 6.90% |
| Horner's syndrome | 3 | 5.17% |
| Gaze palsy | 2 | 3.45% |
| No significant clinical findings | 2 | 3.45% |
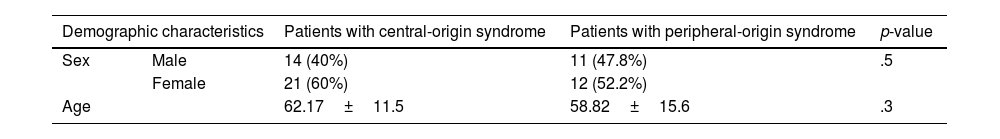
Table 4 shows the results of the differences in demographic characteristics between patients with central-origin syndrome and peripheral-origin syndrome.
Results of the differences in demographic characteristics between patients with central-origin syndrome and peripheral-origin syndrome.
| Demographic characteristics | Patients with central-origin syndrome | Patients with peripheral-origin syndrome | p-value | |
|---|---|---|---|---|
| Sex | Male | 14 (40%) | 11 (47.8%) | .5 |
| Female | 21 (60%) | 12 (52.2%) | ||
| Age | 62.17±11.5 | 58.82±15.6 | .3 | |
We note from the previous table that there are no statistically significant differences between the 2 groups of patients in terms of demographic characteristics.
Table 5 shows the results of differences in the prevalence of vascular risk factors between patients with central-origin syndrome and peripheral-origin syndrome.
Results of differences in the prevalence of vascular risk factors between patients with central-origin syndrome and peripheral-origin syndrome.
| Vascular risk factor | Patients with central-origin syndrome | Patients with peripheral-origin syndrome | p-value |
|---|---|---|---|
| Hypertension | 15 (65.2%) | 20 (57.1%) | .5 |
| Smoking | 9 (39.1%) | 15 (42.9%) | .7 |
| Diabetes mellitus | 13 (56.5%) | 11 (31.4%) | .04 |
| Prior stroke | 10 (43.5%) | 7 (20%) | .04 |
| Prior myocardial infarction | 5 (21.74%) | 2 (5.71%) | .1 |
| Hyperlipidemia and hypercholesterolemia | 4 (17.39%) | 2 (5.71%) | .07 |
| Atrial fibrillation | 3 (13%) | 2 (5.7%) | .3 |
| Hypercoagulable state | 1 (4.3%) | 0 (0%) | .2 |
We note from the previous table that there were statistically significant differences with regard to the presence of diabetes mellitus and previous stroke, which were higher in the group of patients with central-origin syndrome.
Table 6 shows the results of the differences in accompanying symptoms between patients with central-origin syndrome and peripheral-origin syndrome.
Results of the differences in accompanying symptoms between patients with central-origin syndrome and peripheral-origin syndrome.
| Accompanying symptom | Patients with central-origin syndrome | Patients with peripheral-origin syndrome | p-value |
|---|---|---|---|
| Headache | 8 (34.8%) | 9 (25.7%) | .4 |
| Dysarthria | 5 (21.7%) | 2 (5.7%) | .02 |
| Dysphagia | 4 (17.4%) | 0 (0%) | .01 |
| Ptosis | 2 (8.7%) | 0 (0%) | .07 |
| Hearing loss | 1 (4.3%) | 1 (2.9%) | .7 |
| Tinnitus | 0 (0%) | 2 (5.7%) | .2 |
We note from the previous table that there are statistically significant differences with regard to the presence of dysphagia and dysarthria, which were higher in patients with central-origin syndrome.
Table 7 shows the results of the differences in clinical examination findings between patients with central-origin syndrome and peripheral-origin syndrome.
Results of the differences in clinical examination findings between patients with central-origin syndrome and peripheral-origin syndrome.
| Clinical sign | Patients with central-origin syndrome | Patients with peripheral-origin syndrome | p-value |
|---|---|---|---|
| Romberg sign | 0 (0%) | 35 (100%) | .0001 |
| Ataxia | 17 (73.9%) | 0 (0%) | .0001 |
| Positive finger to nose test | 12 (52.2%) | 0 (0%) | .0001 |
| Facial hemisensory loss | 6 (26.09%) | 0 (0%) | .004 |
| Body hemisensory loss | 6 (26.09%) | 0 (0%) | .001 |
| Peripheral facial palsy | 4 (17.4%) | 0 (0%) | .01 |
| Diminished gag reflex | 4 (17.4%) | 0 (0%) | .01 |
| Horner's syndrome | 3 (13%) | 0 (0%) | .02 |
| Gaze palsy | 2 (8.7%) | 0 (0%) | .07 |
| No significant clinical findings | 2 (8.7%) | 0 (0%) | .07 |
We note from the previous table that there are statistically significant differences in the clinical examination findings between the 2 groups with regard to the presence of Romberg's sign, which was present only in patients with peripheral-origin syndrome, as well as with regard to the presence of ataxia, a positive finger-to-nose test, hemisensory loss in half of the face or body, peripheral facial palsy, gag reflex weakness, and Horner's syndrome, which were present only in patients with the central-origin syndrome. There were no statistically significant differences regarding the presence of gaze palsy or the absence of significant clinical findings.
Table 8 shows the results of the HINTS test in both central and peripheral acute vestibular syndrome patients.
From the table, we found that the sensitivity of the HINTS test in diagnosing central acute vestibular syndrome is 95.65% (95% CI [88–100]) and its specificity is 94.29% (95% CI [84–99]).
Table 9 shows the results of the horizontal head impulse test in both central and peripheral acute vestibular syndrome patients.
From the table, we found that the sensitivity of the horizontal head impulse test in diagnosing central acute vestibular syndrome is 91.30% (95% CI [81–97]) and its specificity is 97.14% (95% CI [90–100]).
Table 10 shows the results of the nystagmus examination in both central and peripheral acute vestibular syndrome patients.
From the table, we found that the sensitivity of the nystagmus examination in diagnosing central acute vestibular syndrome is 78.26% (95% CI [66–83]) and that its specificity is 94.29% (95% CI [72–93]).
Table 11 shows the results of the skew deviation test in both central and peripheral acute vestibular syndrome patients.
From the table, we found that the sensitivity of the skew deviation test in diagnosing central acute vestibular syndrome is 21.74% (95% CI [13–34]) and its specificity is 100% (95% CI [91–100]).
DiscussionThe study included (n=58) patients with a mean age of 60.15 years. The percentage of females in our study was 56.90%. This is consistent with the study conducted by S. Agus et al., which found that vestibular symptoms are more prevalent in women and that the most common age of onset ranges from 51 to 60 years. [15] Another study conducted by T. Muelleman et al. showed that women are more affected and that the peak incidence occurs at the age of 60–69 years. [16]
We found that the most common vascular risk factor in patients is hypertension. The results also showed that there were statistically significant differences regarding the presence of diabetes mellitus and previous strokes, which were higher in the group of patients with central-origin syndrome. This may be because diabetes, known for its severe vascular complications, is more difficult to treat than hypertension. It is known that having a stroke increases the likelihood of other strokes in the future.
The proportion of central lesions was 39.66%, despite the sample being selected from patients with high vascular risk. This is consistent with peripheral lesions being much more common, as all studies have shown.17
In patients with central lesions, we found that ischemic stroke was the most common cause, and cerebellar infarction was the most common, accounting for 34.78%. We found bulbar infarction in 5 patients (21.74%), pontine infarction in 4 (17.39%), cerebellar metastasis in 3 (14.04%), cerebellar peduncle infarction in 2 (8.70%), and cerebellar hemorrhage in 1 (4.35%). This is consistent with what Kerber and Kattah found.5,18
A clinical examination of patients with peripheral acute vestibular syndrome showed that peripheral vestibulopathy affected the right side in 22 patients (62.86%) and the left side in 13 patients (37.14%). This is consistent with the study of both Mandala and Shim, which showed that the right side is more affected by vestibular neuritis than the left side.19,20 Cnyrim found that the ratio of right ear involvement to left ear involvement was 1.5:1.3 Researchers have not found an explanation for this phenomenon yet.
We found that the most common symptom accompanying both the central and peripheral lesions is headache, at a rate of 34.8% and 25.7%, respectively. The results also showed statistically significant differences with regard to the presence of dysphagia and dysarthria, which were higher in patients with central-origin syndrome. This is consistent with what Cnyrim found in his study.3
Clinical examination showed that ataxia is the most common sign seen in patients with central lesions, at a rate of 73.9%. The most common sign seen in patients with peripheral lesions is the Romberg sign, with a rate of 100%. The examination did not show any abnormalities in two patients with a central lesion (8.7%). We found statistically significant differences in the clinical examination findings between the 2 groups with regard to the presence of Romberg's sign, which was present only in patients with peripheral-origin syndrome, as well as with regard to the presence of ataxia, positive finger-to-nose test, hemisensory loss in half of the face or body, peripheral facial palsy, gag reflex weakness, and Horner's syndrome, which were present only in patients with the central-origin syndrome. This is consistent with what Cnyrim found in his study.3
The horizontal head impulse test was positive (i.e., indicating a peripheral lesion) in 2 patients with a central lesion and negative (i.e., indicating a central lesion) in 1 patient with a peripheral lesion. Its sensitivity was 91.30% (95% CI [81–97]), and its specificity was 97.14% (95% CI [90–100]). The test was the most sensitive of the 3 tests for diagnosing a central lesion. Cnyrim, Kattah, and Chen found that its sensitivity was 60, 93, and 80, respectively, and its specificity was 93, 100, and 90, respectively.3,5,6
We found that peripheral nystagmus was found in 5 patients with a central lesion and that central nystagmus was found in 2 patients with a peripheral lesion. Its sensitivity was 78.26% (95% CI [66–83]), and its specificity was 94.29% (95% CI [72–93]). Cnyrim, Kattah, and Chen found its sensitivity was 56, 20, and 56, respectively, and its specificity was 83, 100, and 100, respectively.3,5,6
The test of skew was positive (i.e., indicating a central lesion) in 5 patients with a central lesion and negative (i.e., indicating a peripheral lesion) in all patients with a peripheral lesion. Its sensitivity was 21.74% (95% CI [13–34]), and its specificity was 100% (95% CI [91–100]). The test was the most specific of the three tests for diagnosing a central lesion. Cnyrim, Kattah, and Chen found that its sensitivity was 40, 25, and 30, respectively, and its specificity was 100, 96, and 90, respectively.3,5,6
We found that the HINTS test was positive (i.e., indicative of a central lesion) in 22 patients with a central lesion and negative (i.e., indicative of a peripheral lesion) in 33 patients with a peripheral lesion. Thus, the sensitivity of the HINTS test in detecting central acute vestibular syndrome was 95.65% (95% CI [88–100]), and its specificity was 94.29% (95% CI [84–99]). This is consistent with a systematic review by Ohle et al. that included 617 patients and found that the HINTS test had a sensitivity of 96.7% and a specificity of 94.8% when performed by neurologists.7
ConclusionsThe HINTS test has high sensitivity and specificity for diagnosing central acute vestibular syndrome. The sensitivity is 95.65%, and the specificity is 94.29%.
The HINTS test is a simple and easy method that allows early diagnosis of the central lesion, especially since there is no diagnostic method that confirms the diagnosis early.
The horizontal head impulse test has the highest sensitivity among the three tests, amounting to 91.30%.
The skew test has the highest specificity among the 3 tests, reaching 100% in our study.
There are cases of central lesions with clinical manifestations and neurological examination similar to peripheral lesions, which represents a challenge when evaluating patients with acute vestibular syndrome, especially in emergency departments.
RecommendationsWe suggest adopting the HINTS test as part of the routine evaluation of patients with acute vestibular syndrome.
We suggest adopting the HINTS test as a screening test for stroke in patients with acute vestibular syndrome with low vascular risk and an intact neurological examination.
We propose adding the HINTS test to the NIHSS scale to evaluate stroke patients with acute vestibular syndrome.
We suggest that studies be conducted to investigate the sensitivity and specificity of the HINTS test performed using modern video-oculography techniques.
We suggest conducting studies to investigate the sensitivity and specificity of the HINTS test, along with the degree of vascular risk and focal neurological signs, especially ataxia, to achieve optimal sensitivity and specificity of 100%.
Study limitationsIn our study, the HINTS test was performed by neurology residents, which prevents the generalizability of the results, as several studies have found discrepancies in results when the test is performed by emergency physicians.
Ethical disclosuresProtection of human and animal subjects.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.