Super-refractory status epilepticus (SRSE) in pregnancy is a medical emergency that represents a major challenge for physicians. SRSE during pregnancy is rare, but when it does occur, it represents a double threat: significant cognitive sequelae and high mortality rates for the mother, and alterations to foetal growth due to continuous seizures and treatment with antiepileptic drugs (AEDs).1 Despite attempts to identify the most frequent aetiologies and to design treatment protocols, SRSE in pregnancy currently demands significant effort from specialists managing this complication.1,2 We present a case of SRSE in a pregnant patient.
The patient was a 39-year-old woman in the 24th week of her second pregnancy, who presented continuous, generalised tonic–clonic seizures without recovering consciousness between episodes. In the previous weeks, she had visited the hospital due to seizures. She had been diagnosed with idiopathic generalised epilepsy 4 years earlier, and had been under treatment with levetiracetam (LEV; 500 mg/12 h), showing an adequate response; however, seizures reappeared during her first pregnancy (2 years after treatment onset). In the light of this, the dosage of LEV was increased to 750 mg/12 h, and the episodes remitted. Later, at the beginning of her second pregnancy, the patient decided to discontinue treatment.
At the intensive care unit, she presented normal blood pressure (120/75 mm Hg), no proteinuria, and normal CSF values, testing negative for meningoencephalitis and autoimmune encephalitis (anti-NMDAR, anti-VGKC, and anti-DPPX antibodies).
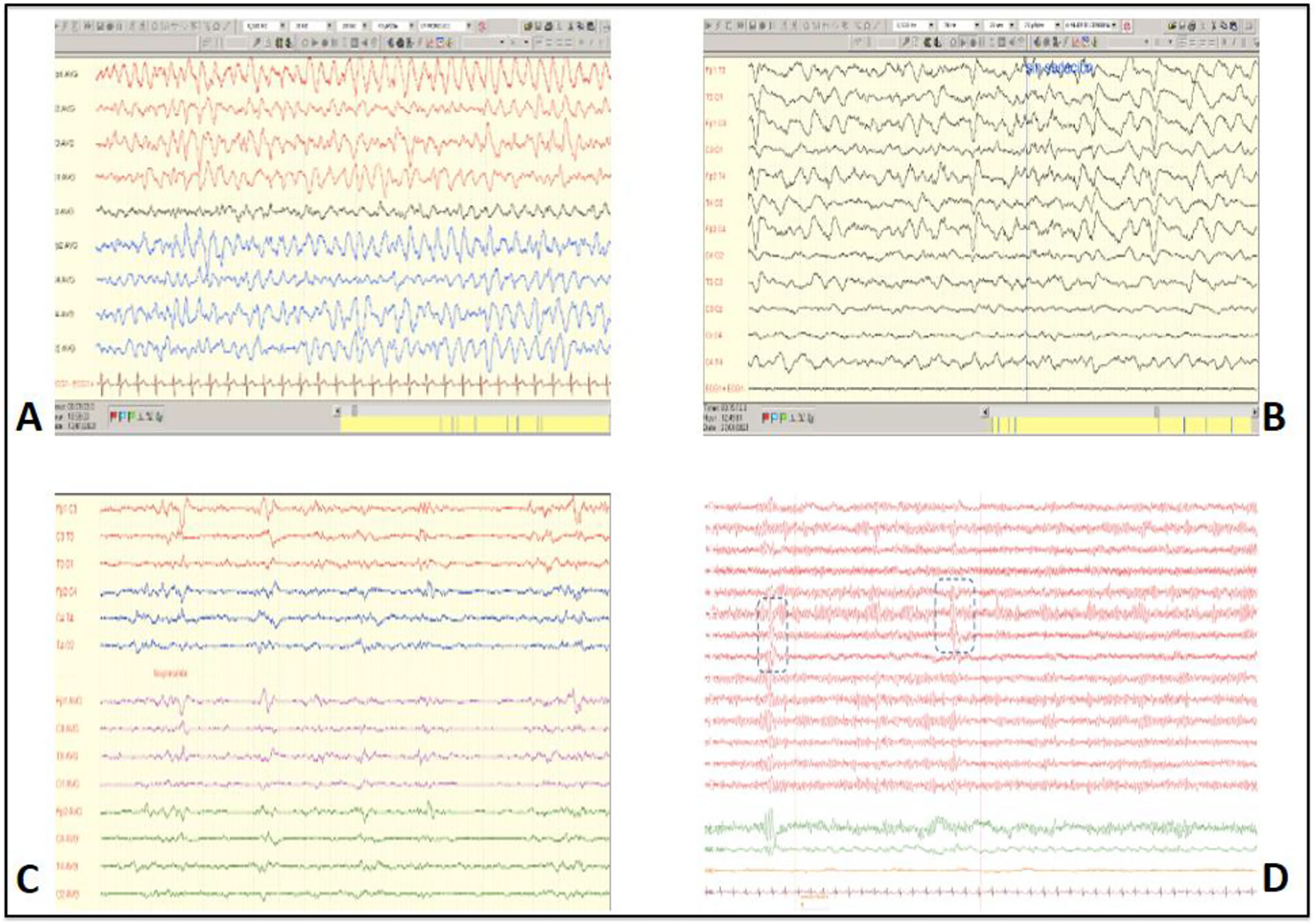
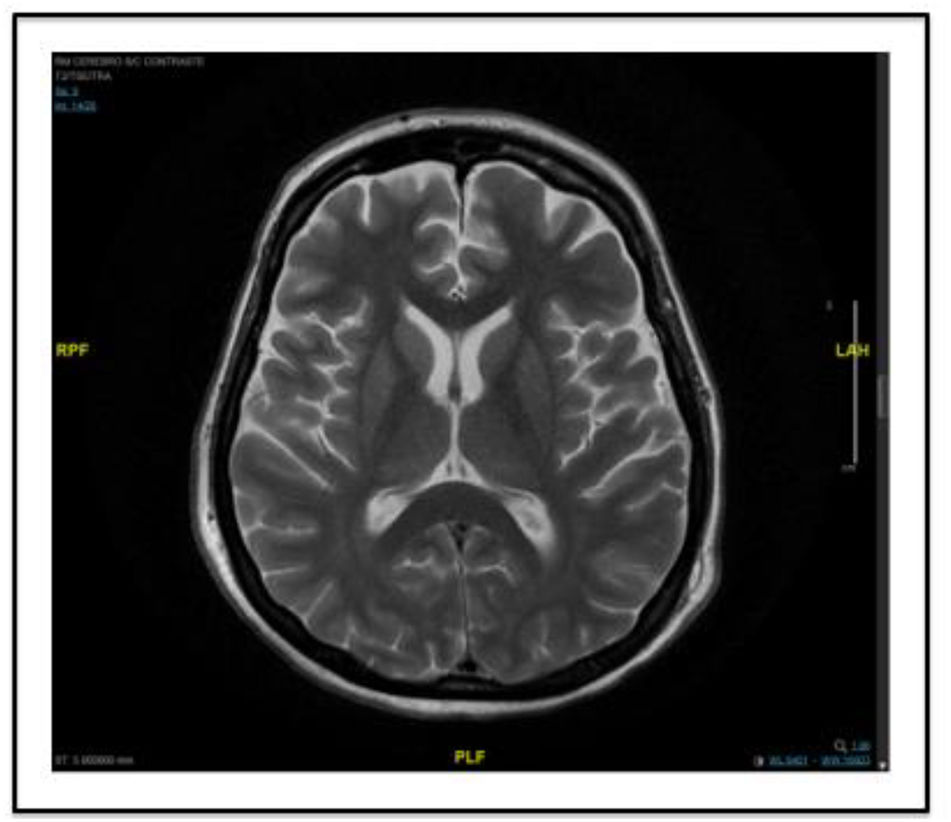
An MRI study yielded normal findings, and an EEG (Fig. 1) showed generalised delta activity with spike-wave patterns and dominant bifrontal projection. The patient was diagnosed with status epilepticus. Several AEDs and combinations of AEDs were administered: LEV at 4000 mg/day, lacosamide at 200 mg/12 h, brivaracetam at 100 mg/12 h, perampanel at 12 mg, valproic acid (VPA) at 4800 mg/day, and immunoglobulins (0.7 g/kg/day for 3 days) with propofol at 15 mL/h and midazolam (MDZ) at 12 mL/h. EEG activity did not improve. On day 14 of SRSE (26 weeks of gestation), due to the high doses of AEDs and anaesthetics, we opted to perform a caesarean section. A new EEG study performed after the procedure showed periodic, lateralised, predominantly bifrontal discharges (Fig. 1). In view of these findings, we added other AEDs: phenobarbital (4 mg/kg/day), a second cycle of immunoglobulins (0.7 g/kg/day for 3 days), and phenytoin (100 mg/8 h); the latter drug was quickly suspended because the patient presented signs of phenytoin hypersensitivity syndrome. Despite this treatment, EEG activity did not improve by day 25. Therefore, we induced barbiturate coma with infusion of thiopental (5 mg/kg/h) for 4 days, achieving no response. On day 30 of SRSE, AEDs were combined with ketogenic diet and methylprednisolone (1 mg/kg/day for 5 days). An MRI study performed 2 days later (Fig. 2), after withdrawal of propofol and MDZ, showed no new findings, and an EEG study showed that epileptiform activity had resolved.
(A) The first EEG study, showing generalised delta activity with spike-wave patterns and dominant bifrontal projection, consistent with status epilepticus. (B) EEG performed on day 15, after the caesarean section, showing periodic, lateralised, predominantly bifrontal discharges. (C) EEG performed on day 27, during barbiturate coma therapy, showing a burst-suppression pattern. (D) Final EEG, showing normal brain activity with occasional, predominantly temporal theta activity.
The patient's progression after resolution of SRSE was good: ketogenic diet was suspended and doses of VPA, phenobarbital, and methylprednisolone were gradually reduced, with no further seizures. At discharge, the patient presented completely normal cognitive function, with EEG showing normal activity with occasional, predominantly temporal theta activity (Fig. 1).
The neonate was born with a severe coagulopathy and remained in the paediatric intensive care unit for more than 80 days. The child presented pulmonary haemorrhage and underwent surgical treatment for intestinal atresia and patent ductus arteriosus.
This article reports the first case of SRSE in pregnancy according to the new ILAE classification, published in 2015, which defines SRSE as status epilepticus persisting for at least 24 h after onset of anaesthesia, including cases in which status epilepticus recurs upon the reduction or withdrawal of anaesthesia. Compared with status epilepticus, SRSE is associated with poorer prognosis and higher mortality rates (25%–58%).3 However, prognosis is even poorer when SRSE manifests during pregnancy.
Many factors contribute to the appearance of seizures in pregnant patients. Firstly, abnormal maternal immune tolerance to the embryo may lead to autoimmunity against brain tissues, and the resulting increases in levels of neurokinin B, inflammatory cytokines, endothelins, and tissue plasminogen activator may trigger seizures. Secondly, increased oestrogen and progesterone levels, the pharmacokinetic mechanisms of AEDs or withdrawal of these drugs, and psychological or behavioural changes may also cause seizures.2,4
Several causes may be identified. AED withdrawal, as in the case of our patient, is the most frequently described in the literature. Other common causes that may be ruled out with EEG, MRI, and laboratory studies include eclampsia, posterior reversible encephalopathy syndrome, venous sinus thrombosis, autoimmune encephalitis, subarachnoid haemorrhage, cavernoma, pyridoxine deficiency, and viral encephalitis.2,4
However, the greatest challenge in pregnant patients is their treatment. While many standardised protocols have been developed for SRSE in the general population, most of the drugs recommended are harmful to the foetus. However, continuous seizures reduce placental blood flow, potentially giving rise to intrauterine growth restriction, pre-term birth, or low birthweight.2 LEV is recommended for the treatment of SRSE in pregnancy, as it is the safest AED for the foetus; the combination of two anaesthetic agents such as propofol and MDZ is permitted as, due to their shorter half-life, they are associated with lower risk, better cardiovascular stability, and less liver damage than thiopental; the use of VPA should be limited due to its teratogenic effects.1
One study establishes that SRSE should be managed in accordance with its aetiology and the foetus' gestational age,1 and several authors report cases in which SRSE remitted with termination of pregnancy4; however, in our case, this did not occur immediately or in the following days. It is difficult to establish whether SRSE in our patient resolved due to caesarean section, and what role the other treatments played.
This was a challenging case, with good outcomes for mother and neonate.
Consent to publicationThe patient gave written informed consent for the publication of this article and the accompanying images.
Conflict of interestThe authors have no conflicts of interest to declare.