The first description of Horner syndrome in humans was made in 1864 in a 24-year-old soldier who was shot in the cervical region. In 1869, Johann Friedrich Horner further detailed a description of the neurological syndrome as the combination of ptosis, miosis and anhidrosis.1 Horner's syndrome results from the injury of the sympathetic system, with the most frequent cause being neoplastic (35–60%), other causes including infections and iatrogenesis (10–18%), and finally vascular and traumatic causes (4–13%).2 Although the first description of the syndrome was secondary to penetrating injury, it is considered a rare complication of cervical trauma, especially if there is no carotid dissection; hence the relevance of this case.
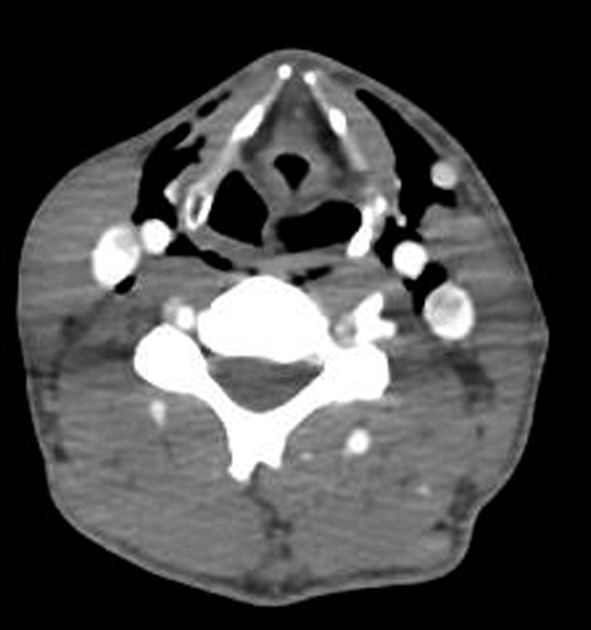
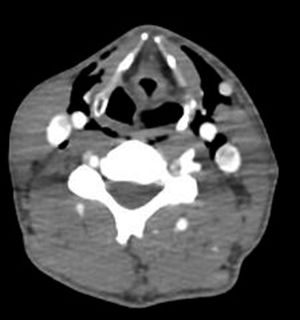
A 39-year-old man was admitted to the emergency room in our hospital after a car accident. No previous diseases were known. There was no loss of consciousness, no nausea or vomiting, and he remained hemodynamically stable during his stay in the emergency room. Upon examination, respiratory and cardiac auscultation was normal, however palpitations revealed that the patient had pain in the right antero-superior iliac spine and right rib, as well as ptosis and miosis of the left eye, without apparent anhidrosis (fig. 1). There were neither latero-cervical murmurs nor subcutaneous emphysema found during the physical exam, and the rest of the neurological examination was without clinically relevant findings. A protocol CT total body scan revealed cervical emphysema, pneumomediastinum, pulmonary contusion and splenic laceration. A CT angiography of the neck was specially requested, showing bilateral latero-cervical emphysema with no dissection of the carotid or vertebral arteries (fig. 2). Given the results, we performed a neurosonological study with an ecodoppler that showed no intimal flap, although it showed hipoecogenic bubbles surrounding the left carotid artery. Conservative treatment was pursued related to the neurologic findings and after one year the patient improved to full recovery of the symptoms.
Horner's syndrome results from a lesion to the oculosympathetic pathway at some point along its path from the hypothalamus to the ocular innervation passing through the adventitial layer of the internal carotid artery. Oculosympathetic paralysis arises from injury to the first, second, or third neuron. Clinically, it presents with ptosis due to involvement of the Müllerian muscle, miosis, and in its complete form, facial anhidrosis. The presence of anhidrosis, not present in our patient, usually suggests a central or preganglionic (first or second-order) lesion.
We suspected a post-traumatic Horner syndrome due to the presence of a cervical emphysema with no carotid damage, probably due to compression of third-level neurons rather than direct neuronal injury, because of the rapid recovery after conservative treatment. Despite it being a rare condition, this phenomenon has been reported previously without vascular damage, although with different pathological mechanisms. The case-reports described in the literature are due to different etiologies, such as: penetrating cervical injury,3,4 severe retching,5 fracture of the first rib6 or have been described as a post-surgical complication, specially in relation to otorhinolaryngology, thoracic and cervical spine surgeries.7,8 The difference and importance of the clinical case presented lies in the fact that our patient had a lesion of the sympathetic pathway without apparent cervical injury or traumatic vascular injury.
This clinical report highlights the importance of always considering a vascular emergency and suspecting carotid dissection until proven otherwise in the case of a post-traumatic Horner syndrome, even with minor trauma such as cervical manipulations or jerky head movements due to the proximity of the internal carotid to the sympathetic system, as the management of the disease changes according to the etiology of the syndrome.
Declaration of competing interestThe authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical considerationsThe authors declare that they have followed their center's protocols on the publication of patient data and have obtained the corresponding permissions.