The united airways concept calls for a multidisciplinary approach to asthma and/or chronic rhinitis/rhinosinusitis (CRS), aimed at integral airway treatment1,2 and better coordination among specialists.3 Failure to treat rhinitis/rhinosinusitis is associated with poor asthma control, especially of severe asthma.4,5 Biological treatments targeting type 2 (T2) inflammatory mediators in severe respiratory diseases offer a new therapeutic option directed against the pathophysiological mechanism of these difficult-to-control united airways diseases (UAD).
UAD endotyping/phenotyping currently focuses on distinguishing between T2 and non-T2 inflammation as a determining factor in the choice of biologic. In our setting, >80% of patients with CRS with nasal polyps (CRSwNP) and >50% of asthmatic patients have a T2 inflammatory endotype in the nasal and bronchial mucosa that may benefit from the same biologic. CRSwNP, with or without asthma, is the most severe form of T2 inflammation in the upper airway, and is also the most costly due to the greater need for treatment and use of healthcare services, and a greater reduction in health-related quality of life (HRQoL). There are currently no T2 inflammation biomarkers that can predict the response of patients with a specific inflammatory endotype to biological treatment. Consequently, therapeutic decisions are still based on phenotypic characteristics or clinical markers.
Several studies have shown a link between the upper and lower airways. In patients with asthma and CRSwNP, a correlation has been shown between higher sinus occupancy and poorer asthma control.6 Late onset is associated with severe asthma,7 and the same is true of CRSwNP and aspirin-exacerbated respiratory disease (AERD), which usually appears between the fourth and fifth decades of life. AERD is associated with severe asthma and CRSwNP, and is a clinical marker of UAD severity.8
Anosmia is linked to the intensity of T2 inflammation and predicts positive findings in nasal endoscopy (NE) and sinus computed tomography (CT) scan.9,10 Anosmia is also a determining factor in QoL measured using the Sinonasal Outcome Test (SNOT-22).
There are several T2 inflammation biomarkers in UAD, mainly eosinophilia, fractional exhaled nitric oxide (FeNO), and total serum IgE. Evidence has shown that the greater the intensity of T2 inflammation, the higher the prevalence of CRSwNP and its multimorbidity with asthma.
Poor implementation of UAD concept, failure and lack of coordination in the management of UAD comorbidities, absence of a common interdisciplinary language that unifies concepts and the way in which to record standard “quantifiable” variables, have been identified as the main unmet needs in patient management.
A multidisciplinary group of Ear, Nose and Throat (ENT) physicians, allergologists, pulmonologists and hospital pharmacists from different centres met with the aim of developing a checklist for the management of UAD, for interdisciplinary use. The item selection was unanimously agreed after three rounds of review in which the discussion focused on the definitions of inflammatory phenotypes and endotypes (T2 or non-T2) and on the selection of T2 biomarkers and clinical markers. The diagnostic definitions and the severity and control criteria proposed in Clinical Practice Guidelines (CPGs) were used, as well as the criteria provided in international consensus documents for selection of CRSwNP patients for biological treatment.2,4,11,12 This checklist aims to facilitate the standardised recording of clinical and biological markers that can be used to objectively evaluate the degree of involvement and response in each patient, and to improve both interdisciplinary communication and patient selection and follow-up for anti-T2 biological therapy in routine clinical practice.
A standard checklist should include the collection of clinical markers of UAD severity. CRSwNP, late-onset asthma, AERD, anosmia, impaired QoL, surgical recurrence, and corticosteroid dependence are independently associated with severe asthma, and are useful clinical markers to select candidates for biological therapy.2,12 The same variables that reflect CRSwNP severity can be used to evaluate therapeutic response.13 Improvement in symptoms and NP size on NE, sinus occupancy on sinus CT scan, and QoL may be indicators of a good response to biologics and, therefore, of a reduction in the need for systemic corticosteroids.
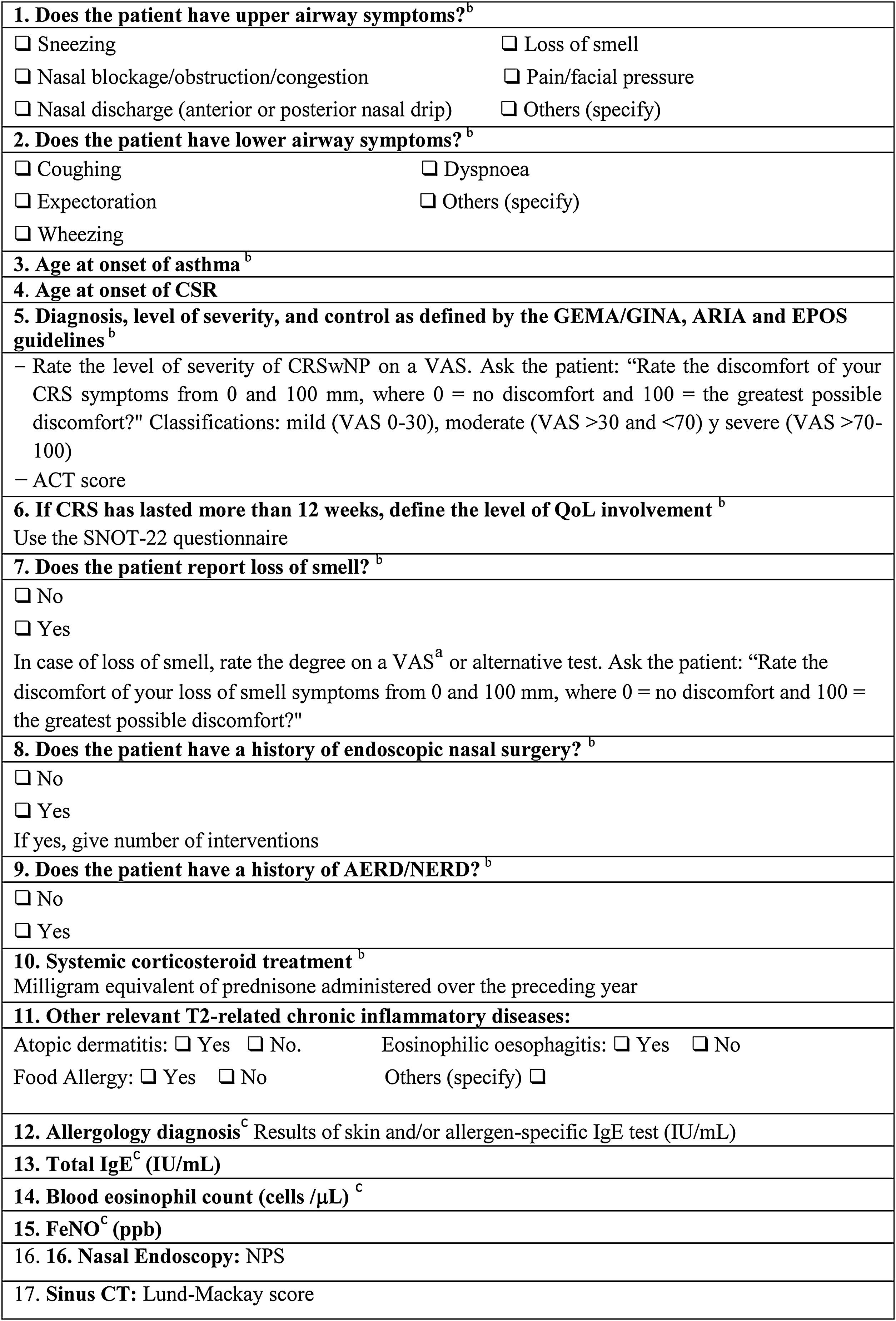
The checklist for the unified approach to UAD (Table 1) includes the recording of upper and lower airway symptoms, as well as specific clinical situations such as AERD.
Data collection checklist for multidisciplinary management and standardised approach to T2 inflammation-related diseases of the airway: CRSwNP and Asthma.
Abbreviations: ACT, asthma control test; CRS, chronic rhinosinusitis; CRSwNP, chronic rhinosinusitis with nasal polyps; FeNO, fractional exhaled nitric oxide; IgE, immunoglobulin E; IU, international units; AERD/NERD, aspirin or nonsteroidal antiinflammatory drug (NSAID)-exacerbated respiratory disease; NPS, nasal polyp score; ppb, parts per billion; SNOT-22, sino-nasal outcome test 22; QoL, quality of life; VAS, visual analogue scale.
aEVA 0–100mm. Anosmia is indicated by VAS>70mm, Hyposmia by VAS>30mm and <70 and Normosmia by VAS<30mm.
bClinical markers of severity.
cBiological markers of T2 inflammation.
Issues related to the standard diagnostic strategy in the management of UAD were also included. For the treatment of sinonasal diseases, the 4-step diagnostic algorithm proposed in the latest SEPAR guidelines for the management of UAD was considered14:
- –
Step 1: note nasal and sinus symptoms in the medical record using the definitions established in the ARIA and EPOS CPGs,2,4 and assess the severity level using a visual analogue scale (VAS) (Table 1). Special attention should be paid to recording anosmia9 and rating its severity using a VAS (Table 1); this does not preclude the use of other more specific smell tests.
- –
Step 2: evaluate polyp size (Nasal Polyp Score [NPS]) using NE.
- –
Step 3: perform respiratory allergy tests. The most commonly available T2 biomarkers in routine clinical practice are included: blood eosinophils (cells/μL), FeNO (ppb), total IgE (IU/mL), skin allergy testing or specific IgE in blood. The SNOT-22 questionnaire is recommended for QoL assessment.
- –
Step 4: perform imaging tests, primarily sinus CT scan and evaluation using the Lund-Mackay score (required for presurgical assessment).
Finally, the checklist includes questions regarding the presence of other T2 diseases, especially atopic dermatitis, food allergy and eosinophilic oesophagitis.
In summary, CRSwNP and late-onset asthma can be treated with the same anti-T2 biological therapy, which allows a comprehensive approach to UAD and requires proper patient selection.15 The use of a standard checklist of objective variables as part of the multidisciplinary UAD management could significantly improve clinical communication between specialists, in addition to facilitating the early diagnosis of T2 inflammatory diseases of the entire airway, and the proper selection of candidates for biological treatment, with subsequent follow-up and evaluation of their response. To the best of our knowledge, this is the first proposal for a standard interdisciplinary checklist for the management of T2 inflammation of the airways in the context of asthma and CRSwNP. This consensus checklist will need to be validated in clinical practice. Also, research on the quantitative evaluation of the proposed variables might help to predict the need for subsequent therapeutic interventions.
Authors’ contributionAll authors have equally contributed to and approved the content of this manuscript.
FundingThis work has been carried out within the framework of the Vía Respiratoria Única (United Airway) project, which has received unconditional sponsorship from AstraZeneca.
Conflicts of interestJ.-A.C.V.: Advisory boards for and speaker's honoraria from GSK, AstraZeneca and Sanofi. Financial assistance with travel/attendance to meetings from AstraZeneca, GSK, Novartis and Sanofi.
M.A.-C.: Consultancy fees from Sanofi, AstraZeneca and Novartis. Speaker's honoraria from Sanofi.
J.D.R.: Speaker's honoraria from Bial, AstraZeneca, Sanofi, GSK, Chiesi and Novartis.
AstraZeneca. Financial assistance with travel/attendance to meetings from Sanofi.
M.G.: Speaker's honoraria from AstraZeneca, Sanofi and Genzyme. Advisory boards and data safe monitoring for AstraZeneca, Sanofi and Genzyme.
C. Colás: Speaker's honoraria from GSK, AstraZeneca, Sanofi, Viatris, Chiesi and Novartis. Financial support for materials, equipment or other services from GSK, AstraZeneca and Viatris.
I.P.G.: Speaker's honoraria from GSK, AstraZeneca, and other non-profit organizations. Financial assistance with travel/attendance to meetings from AstraZeneca.
C. Cisneros: Funding/grant support for research projects from AstraZeneca, GSK, Novartis, Sanofi, Chiesi, Pfizer and Muncipharma. Consultancy fees from Sanofi, AstraZeneca, GSK and Novartis. Speaker's honoraria from GSK, AstraZeneca, Sanofi, Menarini, Chiesi and Novartis. Financial assistance with travel/attendance to meetings from AstraZeneca, GSK, Novartis and Sanofi. Advisory boards and data safe monitoring for GSK, Novartis, AstraZeneca and Sanofi. Financial support for materials, equipment or other services from GSK, AstraZeneca and Chiesi.
The authors would like to thank Susana Cañón-Sánchez from Medical Statistics Consulting S.L. (Valencia) for providing scientific support and medical writing services.