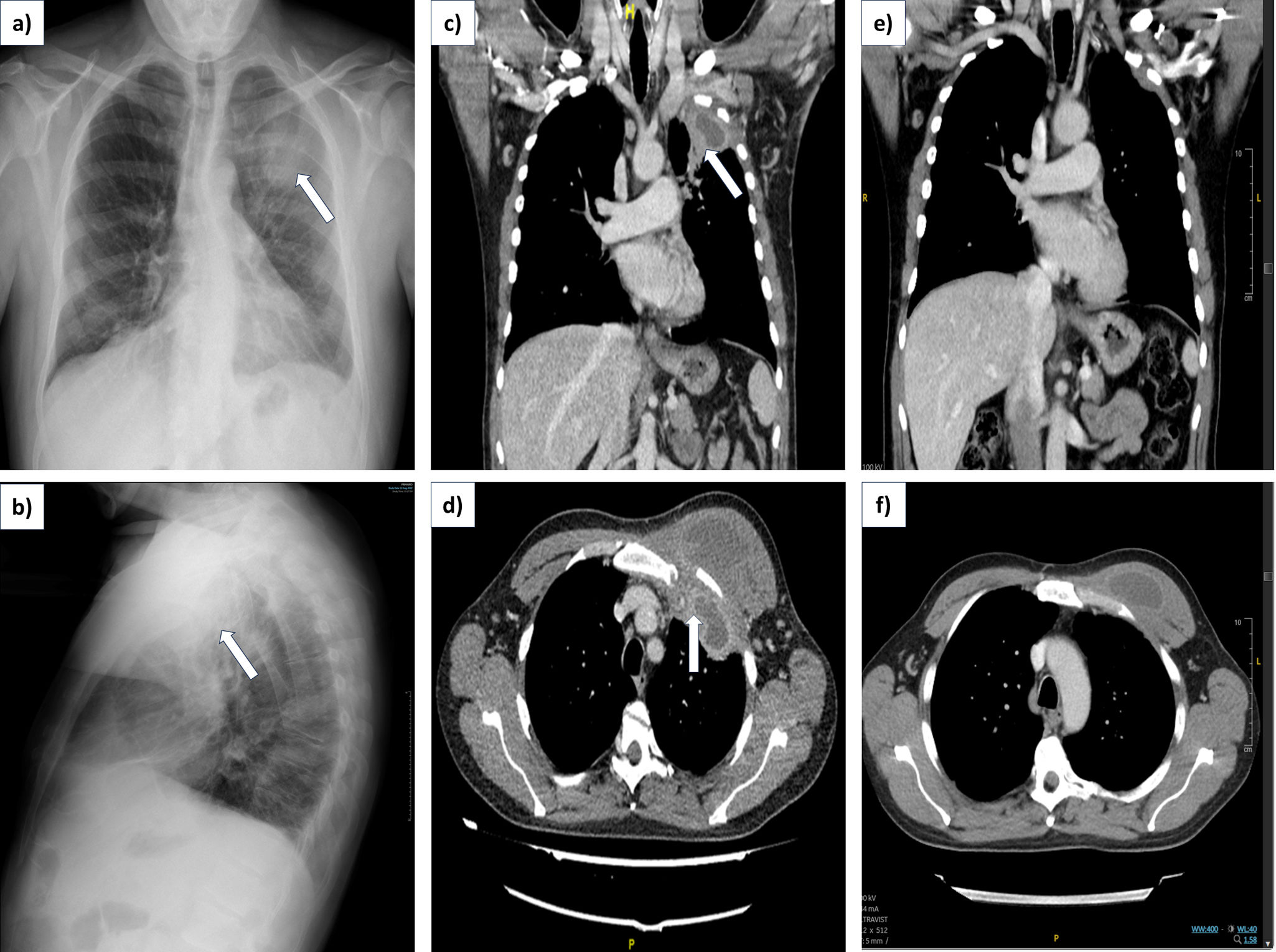
A 41-year-old male smoker, with a history of severe atopic dermatitis, hyper IgE syndrome (confirmed STAT3-HIES [exon20 mutation]) diagnosed at 12 years of age and allergic phenotype asthma treated with LABA/ICS and omalizumab, with a personal history of recurrent skin infections and two episodes of uncomplicated pneumonia. Consulted due to a painful tumor in the left infraclavicular region, difficulty moving the left arm, and cough with mucopurulent expectoration. Physical examination revealed facial eczema and a tumor fixed to deep planes on the left chest wall, with skin rubefaction. Laboratory tests showed leukopenia, anemia and elevated C-reactive protein levels. Chest radiography revealed a left upper lobe mass (LSI) (Fig. 1a and b). Chest tomography (CT) demonstrated a hypodense lesion with central necrosis and peripheral enhancement, infiltrating pectoral muscles with intrathoracic extension that extended into a pulmonary consolidation in the LSI (Fig. 1c and d). With the suspicion of an abscess/empyema necessitatis without fistulization, an aspiration puncture of 110ml of pus was performed, with wide opening and drainage, confirming a positive culture for methicillin-sensitive Staphylococcus aureus. No malignant cells were detected. The patient received 1g/IV/6h of cloxacillin and later oral amoxicillin–clavulanic acid, achieving clinical and radiological resolution at two months (Fig. 1e and f). HIES is a rare primary immunodeficiency characterized by recurrent skin and sinopulmonary infections, as well as cold pulmonary abscesses, mainly caused by S. aureus, with Streptococcus pneumoniae and Haemophilus species being less common. These infections result from impaired neutrophil chemotaxis and defective Th17 differentiation due to STAT3 mutations, increasing susceptibility to bacterial and fungal infections in the skin and mucosa. In our case, it presented as empyema necessitatis, an unusual manifestation of empyema in an uncommon disease. Although classically attributed to Mycobacterium tuberculosis, it has also been documented with S. aureus.1,2 This case is the first known description of empyema necessitatis in an adult with HIES.
(a and b) Posteroanterior and lateral chest radiographs revealed a 5cm peripheral nodular mass in the left upper lobe. (c and d) Chest CT images (mediastinal window), in both coronal and axial views, demonstrated a necrotizing lesion with extrapleural and intrathoracic extension, along with pulmonary consolidation in the left upper lobe, air bronchogram, septal thickening, micronodules, and erosion of the first rib (arrows). (e and f) Chest CT images (mediastinal window, coronal and axial views) illustrated complete resolution of the empyema necessitatis at 2 months.
Ethical approval was not required for this study. However, written informed consent was obtained from the patient for the publication of this case report and accompanying images.
FundingThe authors received no financial support for the research, authorship, or publication of this article.
Authors’ contributionsAll authors contributed to the study's conception, data collection, analysis, manuscript writing, and final approval.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.