We present the case of a 47-year-old man, a former smoker, with a history of resolved cholesteatoma and vasovagal syncope came to our office. He worked for more than 10 years in a marble workshop making tiles. Consulted in the interstitial lung disease unit immediately after diagnosis in another center of silicosis and systemic symptoms such as weight loss (3–4kg), fever, night sweats, Raynaud's phenomenon, swelling of the fingers, minimal skin thickening on fingers and cheeks without telangiectasias or pitting, myalgia without loss of force, erythematous lesions on the skin and dysphagia that partially improve after the use of corticosteroids. Positron emission tomography (PET/CT) revealed hypermetabolic adenopathies. Endobronchial ultrasound (EBUS) was performed with a report of mature lymphocytes and anthracotic macrophages; no granulomas were observed. In the bronchoscopy there are no microbiological findings that suggest an infectious process and a macrophage bronchoalveolar lavage (BAL) of 90%. Given the suspicion of autoimmune disease, specific studies were performed. Capillaroscopy revealed a pattern of active scleroderma. Dermatological echo described increased Doppler recording in fingers and cheeks. Esophageal manometry showed a hypercontractile esophagus. Muscle resonance described fascial edema in some posterior muscle groups of thighs with distal peritendinous extension and left iliac, without fatty infiltration or edema and a muscle biopsy disclosed findings suggestive as an immune-mediated necrotizing myositis. Serological tests were positive for antinuclear antibodies with nucleolar pattern and anti-Scl 70 antibodies. Spirometry showed normal values with diffusing capacity of the lung for carbon monoxide (DLCO) of 85%.
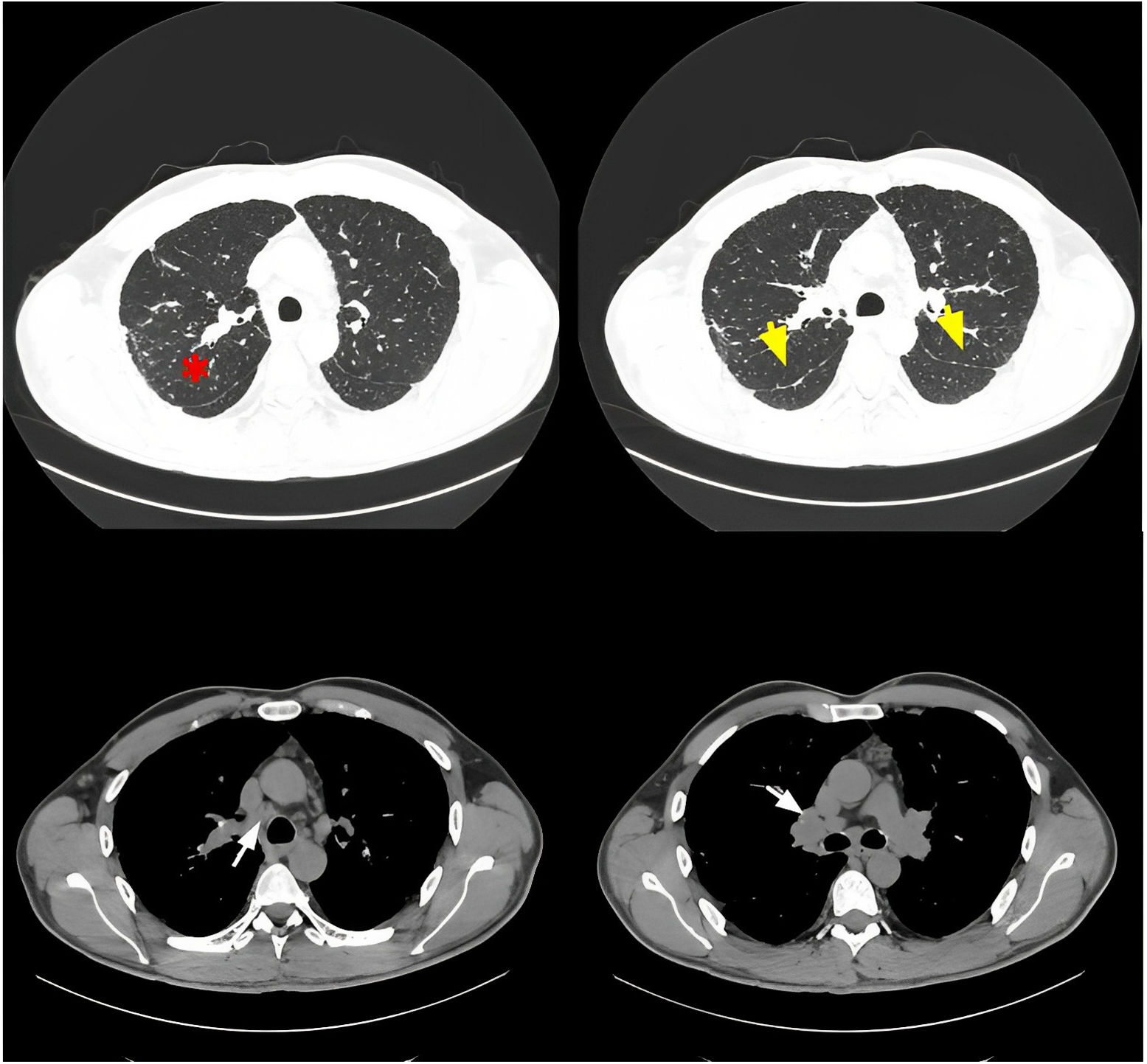
The chest CT revealed micronodules with a diffuse bilateral distribution, with predominantly upper scar paths without data of pulmonary fibrosis (Fig. 1). In multidisciplinary discussion, the patient was diagnosed simultaneously with a combination of systemic sclerosis with limited cutaneous involvement and immune-mediated necrotizing myopathy plus silicosis, defined as Erasmus syndrome. Immunosuppressive treatment based on sodium mycophenolate was started.
Silicosis is a diffuse interstitial occupational disease caused by sustained inhalation of silica with variable presentation and clinical course. Systemic sclerosis developed in people with silicosis is explained by an exaggerated production of proinflammatory substances and changes in cell apoptosis.1
Erasmus syndrome is a rare condition, first described in 1957 as the development of systemic sclerosis in people exposed to silica.2 Diagnosis is made based on the identified exposure history and the presence of clinical, laboratory, and capillaroscopy features consistent with autoimmune disease. Radiological changes must be considered, since it has been described that patients with this association of silicosis plus autoimmune disease can progress and develop pulmonary fibrosis.3
Informed consentInformed consent was obtained from the patient for publication of the clinical data and images present in this manuscript.
Authors' contributionsMaría Belén Noboa: Wrote the manuscript. Arranged the meetings for the reviewers.
Fernanda Hernández González: Manuscript reviewer.
Gema Lledó: Manuscript reviewer.
Gerard Espinosa: Manuscript reviewer.
Jacobo Sellarés: Manuscript reviewer. Senior author.
FundingNo external financing has been needed for this study.
Conflicts of interestDr. Gerard Espinosa has received funding for scientific presentations from Boehringer Ing, Gebro, Glaxo-Smith-Kline. Dr. Jacobo Sellarés has received funding for scientific presentations or grants from Roche, Boehringer Ing and Gebro.