A 34-week-old male neonate was diagnosed with probable pulmonary agenesis at 20-week prenatal ultrasound. At birth, he was placed on noninvasive positive pressure ventilation for 24h, with further quick de-escalation. Chest X-ray was performed showing complete opacification of left hemithorax with mediastinal shift to left and hyperinflation of the contralateral lung.
The echocardiogram showed agenesis of the left pulmonary artery and vein, patent foramen ovale (PFO), persistent ductus arteriosus and double superior vena cava system. Normal abdominal and transfontanelar ultrasounds were also performed.
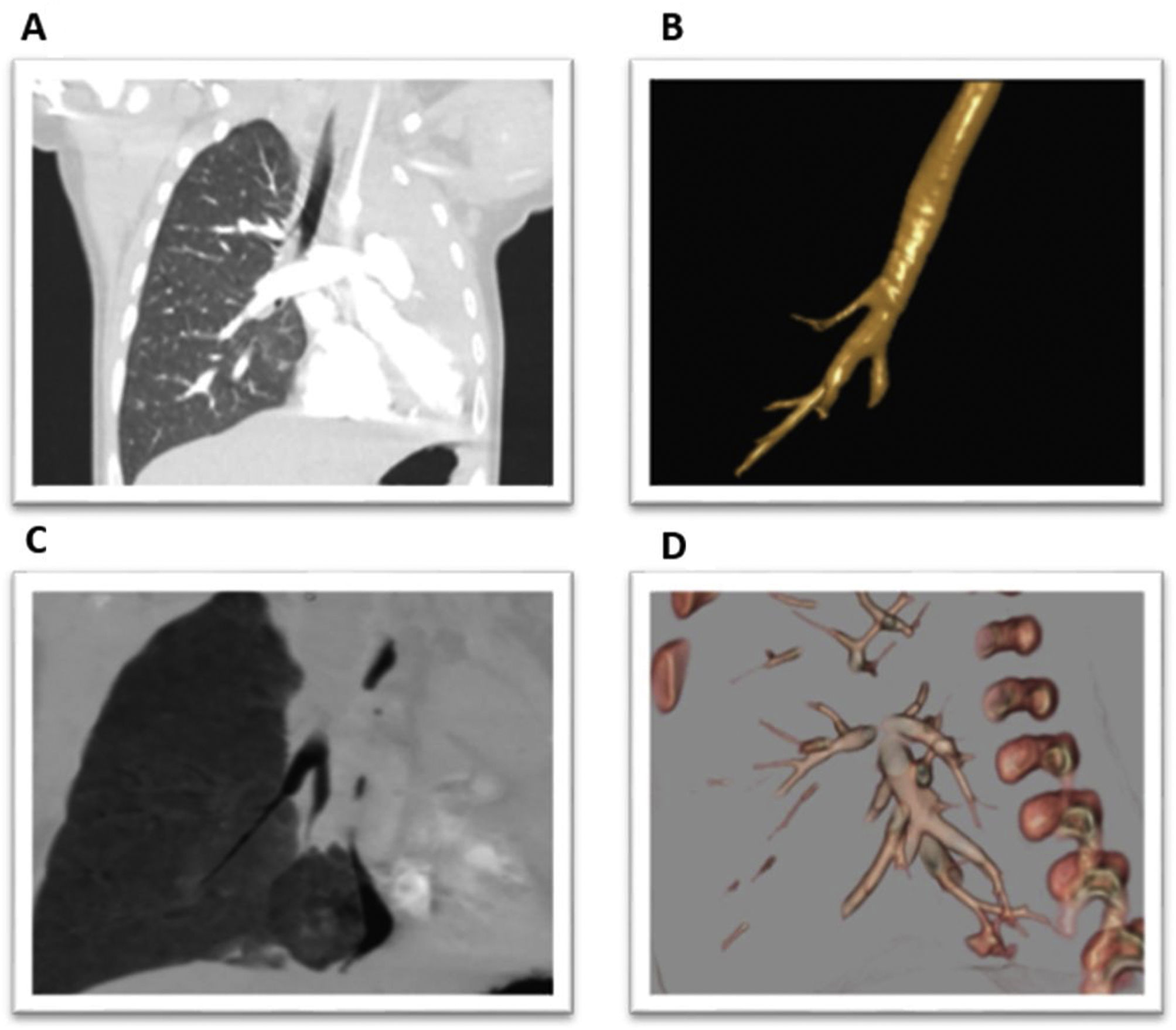
At the 4th month of life, chest computed tomography (CT) confirmed left pulmonary agenesis along with the presence of tracheal bronchus, right accessory pulmonary portion or “islet” with its own bronchus and a small pulmonary artery from the right pulmonary artery and a small arteriovenous fistula in posterior basal segment (Fig. 1).
(A) Coronal section of CT chest showing the tracheal bronchus. (B) 3D reconstruction of the patient's tracheobronchial tree. (C) Coronal section of CT chest showing accessory pulmonary portion separated from the right lung. (D) 3D reconstruction showing the small arteriovenous fistula.
At the age of twenty months, our patient remains asymptomatic. In addition to the current vaccination schedule, he has received pneumococcal polysaccharide vaccine (PPSV23), flu vaccination and RSV-neutralizing monoclonal antibody (Palivizumab).
Pulmonary agenesis is defined as ipsilateral absence of parenchyma, main bronchus, and pulmonary artery1. Despite the complexity of the malformation, the absence of significant clinical signs is not exceptional. Better prognosis has been described in left agenesis, as in the case of our patient. Although it can occur in isolation, pulmonary agenesis is frequently associated with other malformations, mostly cardiovascular anomalies1,2. However, the presence of up to 3 associated pulmonary malformations, as it has been described, is unusual.
Informed consentInformed consent was obtained from the patient's relative for publication of the clinical data and images present in this manuscript.
FundingThis work has no funding.
Authors’ contributionAll authors have contributed to this work as listed in the authors’ contribution section.
Conflicts of interestThe authors do not fear any conflict of interest.