Morphological alterations evaluated by computed tomography (CT) are part of the diagnosis of acute respiratory distress syndrome (ARDS).1 These morphological alterations include: ground glass opacification (heterogeneous density with recognizable vessels, GGO) and airspace consolidation (homogeneous density without recognizable vessels or bronchi, CO).2 CO on CT has been associated with a more severe clinical course and greater progression to death.3 Furthermore, CO refers to lung parenchyma with alveolar occupation, collapse, or a combination of both. Therefore, CO would be related to oxygenation and the degree of lung static compliance (Crs). For this reason, this study aims to evaluate the relationship between CO quantification present in the CT and respiratory variables assessed during the first day of mechanical ventilation (MV).
This prospective study was conducted in the intensive care unit of the Hospital Regional Río Gallegos, Argentina. The institutional ethics board approved the study and it was subsequently registered (NCT02799940). Individuals who met criteria for ARDS according to the Berlin definition1 and who required MV for more than 48h were included. Patients with chronic lung disease, high risk of death within three months for reasons other than ARDS, decision to limit therapeutic effort, and unable to be transferred to radiology in the first 72h from the diagnosis of ARDS. Patients were transferred to Radiology under MV in the first 72h after the ARDS diagnosis. A CT scan of the chest was performed during an end-inspiratory pause. CT was evaluated and quantified according to a previous study.4 Briefly, the CT was assessed at three levels: apex (upper part of the aortic arch), hilum (first section below the carina), and base (2cm above the highest diaphragm). Each level (in each of the lungs) was divided into three sections: ventral, medial and dorsal. In each of the 18 locations, the score was performed through the visualization of three morphological findings: normal lung, GGO, and CO. In each location, the occupation was quantified with a score from one to three, so the sum for each subsection should equal three. Subsequently, total GGO and total CO were considered as the sum of all GGO and CO scores from the 18 locations. Scoring was performed by two authors (RSC and CF) where consensus resolved differences.
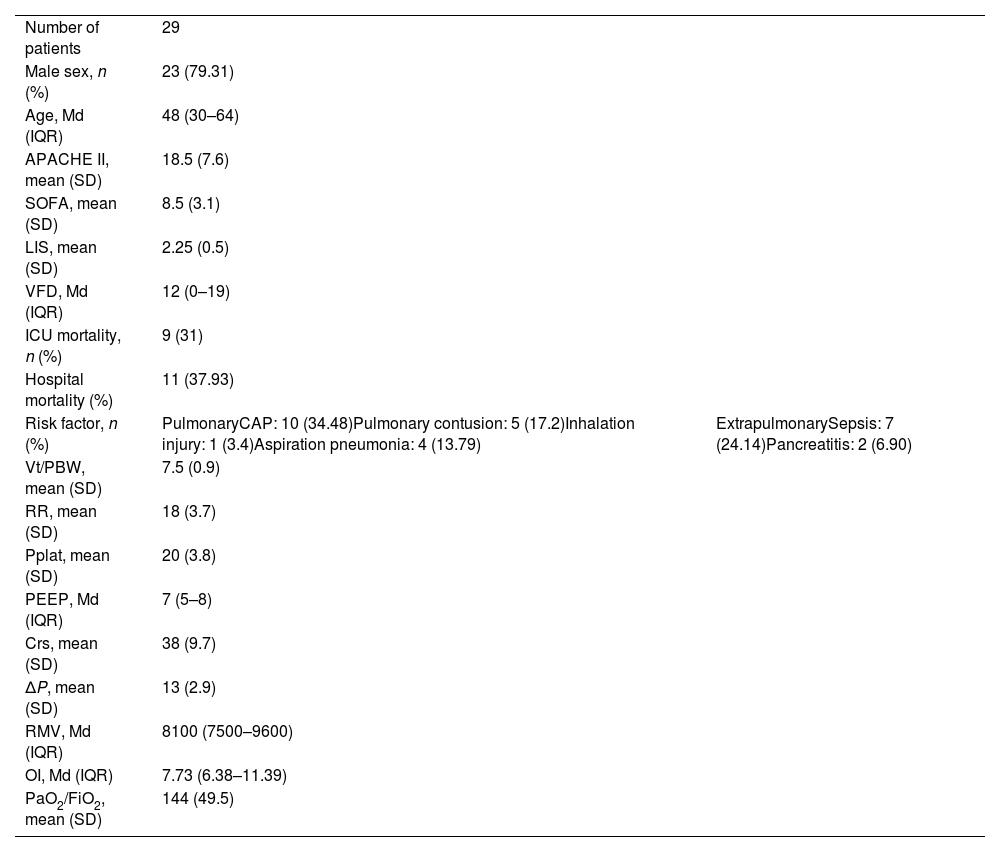
Data were recorded on the first day of ARDS: date of ICU admission, age, gender, APACHE-II score,5 ARDS risk factors, PaO2/FiO2 ratio, lung injury score (LIS),6 SOFA,7 Vt/PBW, PEEP, RR, plateau pressure (Pplat), driving pressure (ΔP: Pplat−PEEP), oxygenation index (OI: (mean airway pressure×FiO2×100)/PaO2), respiratory minute volume (RMV: product between Vt and RR). Ventilator-free days (VFD), ICU and hospital mortality were also recorded. The endpoints of the study were: relationship between total CO and Crs (primary) and relationship between total CO and PaO2/FiO2; Pplat; ΔP; RMV; OI; LIS; and VFD (secondaries). Categorical variables were presented as numbers and percentages, while continuous variables were presented as mean (SD) or median and interquartile range (IQR), as appropriate. Pearson or Spearman correlation tests were also used as appropriate. A value of p<0.05 was considered statistically significant. The sample size was calculated according to a previous study.4
We included 29 patients. Time between the ARDS diagnosis and the CT's performance: 1 day (IQR: 0–1). Baseline characteristics and respiratory parameters are detailed in Table 1. In CT, according to quantification, 11.6% were total GGO (with the greater medial location in the ventral–dorsal gradient), 26.4% corresponded to total CO (with the greater dorsal location), while 61.9% was normal lung. There was a negative correlation between total CO and Crs: −0.38 (p=0.04). In relation to the secondary results, only PaO2/FiO2 (r: −0.4775, p: 0.008), ΔP (r: 0.43, p: 0.01) and VFD (r: −0.42, p: 0.02) presented a statistically significant correlation.
Baseline characteristics and respiratory parameters.
| Number of patients | 29 | |
| Male sex, n (%) | 23 (79.31) | |
| Age, Md (IQR) | 48 (30–64) | |
| APACHE II, mean (SD) | 18.5 (7.6) | |
| SOFA, mean (SD) | 8.5 (3.1) | |
| LIS, mean (SD) | 2.25 (0.5) | |
| VFD, Md (IQR) | 12 (0–19) | |
| ICU mortality, n (%) | 9 (31) | |
| Hospital mortality (%) | 11 (37.93) | |
| Risk factor, n (%) | PulmonaryCAP: 10 (34.48)Pulmonary contusion: 5 (17.2)Inhalation injury: 1 (3.4)Aspiration pneumonia: 4 (13.79) | ExtrapulmonarySepsis: 7 (24.14)Pancreatitis: 2 (6.90) |
| Vt/PBW, mean (SD) | 7.5 (0.9) | |
| RR, mean (SD) | 18 (3.7) | |
| Pplat, mean (SD) | 20 (3.8) | |
| PEEP, Md (IQR) | 7 (5–8) | |
| Crs, mean (SD) | 38 (9.7) | |
| ΔP, mean (SD) | 13 (2.9) | |
| RMV, Md (IQR) | 8100 (7500–9600) | |
| OI, Md (IQR) | 7.73 (6.38–11.39) | |
| PaO2/FiO2, mean (SD) | 144 (49.5) |
APACHE II: acute physiological and chronic health evaluation; CAP: community-acquired pneumonia; Crs: static compliance (ml/cmH2O); ΔP: driving pressure; ICU: intensive care unit; IQR: interquartile range; LIS: lung injury score; Md: median; OI: oxygenation index; PaO2/FiO2: partial pressure of arterial oxygen/fraction of inspired oxygen ratio; PEEP: positive end-expiratory pressure (cmH2O); Ppl: plateau pressure (cmH2O); RMV: respiratory minute volume (ml/min); RR: respiratory rate; SD: standard deviation; SOFA: Sepsis related Organ Failure Assessment; VFD: ventilator-free days; Vt/PBW: predicted tidal volume (ml/kg of predicted body weight).
The main findings of this study are (1) in patients with ARDS, CO present at baseline CT was the most frequent finding and (2) the greater the consolidation (total CO), greater alterations in the respiratory variables: Crs, ΔP, VFD and less oxygenation.
In lung CT, CO refers to absence of alveolar aeration, product of occupation, collapse or a combination of both. A plausible expression in lung mechanics of this morphological alteration should be the decrease in Crs. This pilot study supports this hypothesis, showing that the higher the CO, the lower the Crs. The importance of this result lies in the fact that the quantification of the consolidation in CT can be done, through a simple method for intensivists, without the use of any additional software. In addition, assuming the absence of mathematical coupling between variables (Crs and ΔP), we found a correlation between total CO and ΔP, which is the normalized volume according to the degree of lung compliance. In turn, this relationship, could be of importance in ventilatory management. A recent study found that the benefit of using a low Vt in ARDS varies depending on elastance (inverse of Crs), suggesting that the lung protective ventilation strategy should focus primarily on ΔP to improve elastance rather than from Vt.8 For this reason, the magnitude of CO in relation to mechanical parameters (Crs and ΔP), would allow us to assess the risk of injury related to the Vt according to the Crs. The magnitude of CO, in this way, would have prognostic implications. Furthermore, due to alveolar compromise, the increase in CO should be related to less oxygenation. However, the previous evidence is not conclusive about CO and oxygenation.9–11 The findings of this study support this association, since a negative correlation was found between total CO and PaO2/FiO2. Data from this study also show correlation between VFD and total CO. VFD is a measurement used in studies that address lung function in critically ill patients.12 Its measurement focuses on the duration of MV days, and thus, indirectly, in patients with lung involvement, it would be associated with mortality.13 Our study has certain limitations. We used three axial slices as an expression of the entire lung and this method has been questioned, arguing that the more heterogeneous the lung is, the less representative the assessment may be with only three slices.2 However, several authors have used this methodology,14,15 considering that it is sufficient to assess the lesions present in ARDS. In conclusion, this study evaluated the pulmonary expression of consolidation evidenced in the CT of ARDS patients. It was corroborated that the higher the degree of CO, the lower both oxygenation and Crs. Thus, the CO magnitude, assessed through a simple method, could have prognostic implications. This physiological study presented here will be useful in planning a larger study evaluating clinical endpoints, which may reaffirm the findings of this study.
Authors’ contributionsLiterature search: Roberto Santa Cruz, Fernando Pagano, and Gustavo Domeniconi.
Data collection: Roberto Santa Cruz and Carolina Favot.
Study design: Roberto Santa Cruz.
Analysis of data: Roberto Santa Cruz, Carolina Favot, and Marcelo Choi.
Manuscript preparation: Roberto Santa Cruz and Gustavo Domeniconi.
Review of manuscript: All authors.
FundingThe study had no source of funding.
Conflicts of interestThe authors declare that they have no conflict of interest.
The authors would like to thank the Academic Writing Center (Universidad de Magallanes), who helped us with the writing of the manuscript. We also want to thank Engineer Roberto de Miguel, who helped us with the Stata analysis.