Though many different stents with various diameters and lengths are available, the shapes are hardly ever ideal because of the distorted anatomy in patients with diseased airways.1 For treatment of tracheobronchial stenosis, benign or malignant stenosis, it is essential to choose the correct type of prosthetic material, the stent length to avoid migration and consequent obstruction of the distal airway ventilation.2
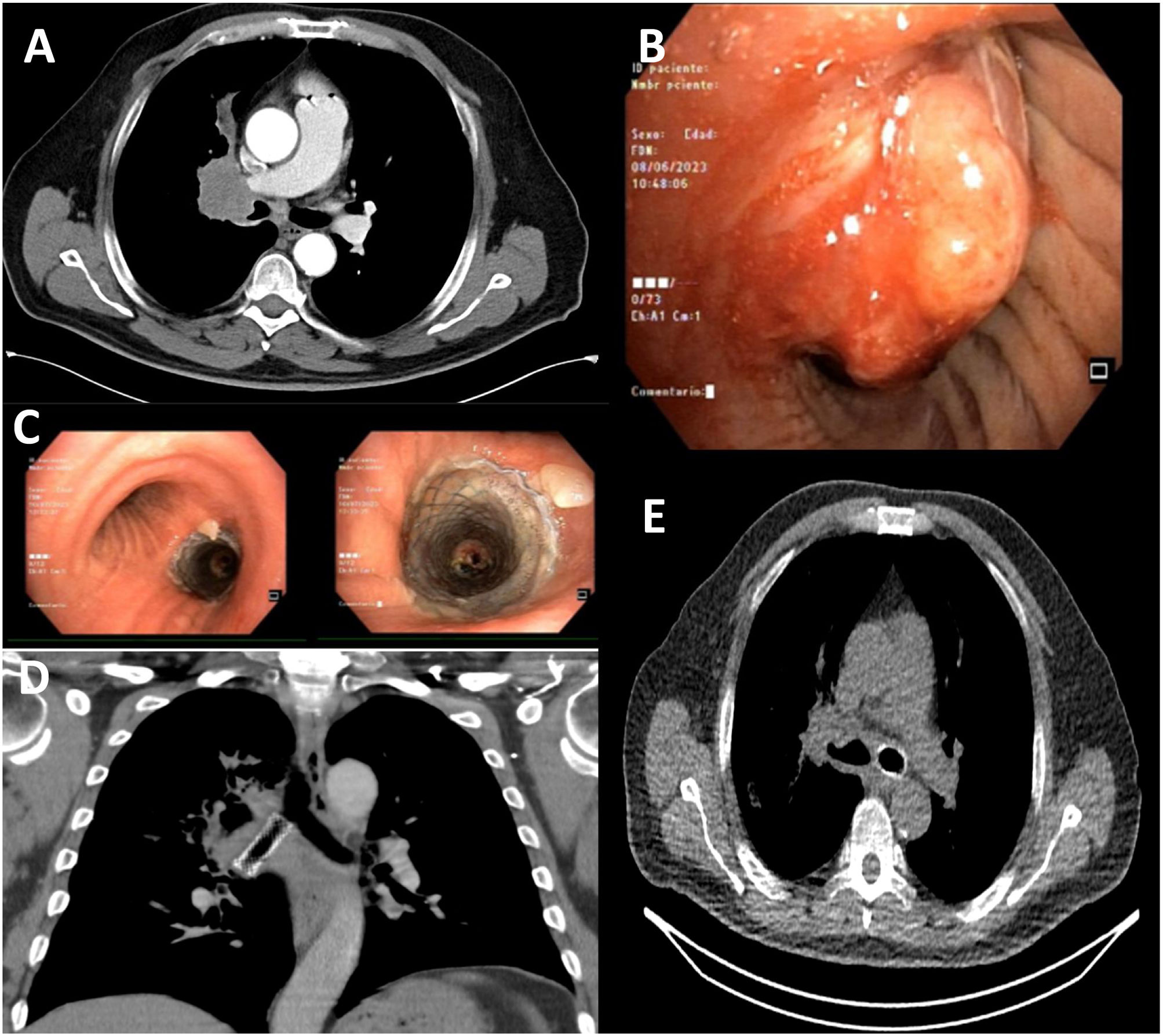
We present a 66-year-old man, ex-smoker with index of 40packs/year, with a history of arterial hypertension, type 2 diabetes mellitus and benign prostatic hypertrophy. As result of hemoptoic expectorations, a chest CT was performed, which revealed a right hiliar mass with wide mediastinal contact and invasion and stenosis of the right main bronchus, and ipsilateral superior lobar bronchus, and intermediate bronchus (Fig. 1A). Flexible bronchoscopy was performed, observing a neoproliferative lesion that occludes the right upper lobe (Fig. 1B) and extends along the lateral surface of the intermediate with 70% bronchial obstruction, which allows visualization of distal lumens, showing free the middle lobe and the right lower lobe.
(A) CT with a right hilar mass with wide mediastinal contact and invasion and stenosis of the right main bronchus, right superior lobar bronchus, and intermediate bronchus. (B) Flexible bronchoscopy with a neoproliferative lung cancer. (C) STENT SEMS LEUFEN 14*40 in the right main bronchus. (D) CT chest coronal section, prosthesis in RMB. (E) Pulmonary ventilation SPECT with axial tomography, migration of stent to LMB.
It was classified as squamous cell carcinoma with subsequent staging cT4N2M1c (left adrenal, hepatic and retroperitoneal implants), PDL-1 of 80%. During systemic treatment, the patient was admitted to the pulmonology service due to hypoxemic respiratory failure secondary to obstructive pneumonitis due to progression of lung neoplasia.
An emergency rigid bronchoscopy was performed where a tumor was observed at the entrance of the right main and intermediate bronchus. After its mechanical resection, a SEMS LEUFEN 14*40 prosthesis was placed (Fig. 1C, D).3 The patient was discharged a week later, undergoing oncological treatment with pembrolizumab with good results and radiological response.
During follow-up, pulmonary ventilation SPECT with axial tomography was performed for suspected PE, where embolus in the pulmonary arteries was ruled out but migration of the stent to the left side was observed (Fig. 1E). A new rigid bronchoscopy was performed where the stent was removed, observing an improvement in the diameter of the right main and intermediate bronchus, not requiring new prosthesis placement.
The natural migration of the material is to move toward the proximal lumen and even expectoration with the coughing itself. What is unusual about this case, is that element was perfectly adapted to the left main bronchus and it could have been adjusted perfectly as did. Therefore, we must not only choose the best possible tracheobronchial stent at the time of its placement,4 but also strictly monitor this kind of synthetic material to treat the granulation tissue that it may generate, or avoid its migration as much as possible,5 given the new targeted systemic therapies and immunotherapy with a decrease in tumor volume in a short time after their first doses.
Informed consentInformed consent was obtained from the patient for the publication of his clinical data and the use of diagnostic images.
FundingThe authors declare that no funding was received for this article.
Authors’ contributionsAll the listed authors have made substantial contributions to all areas as outlined therein.
Conflicts of interestNone of the authors has any conflict of interest of any type.