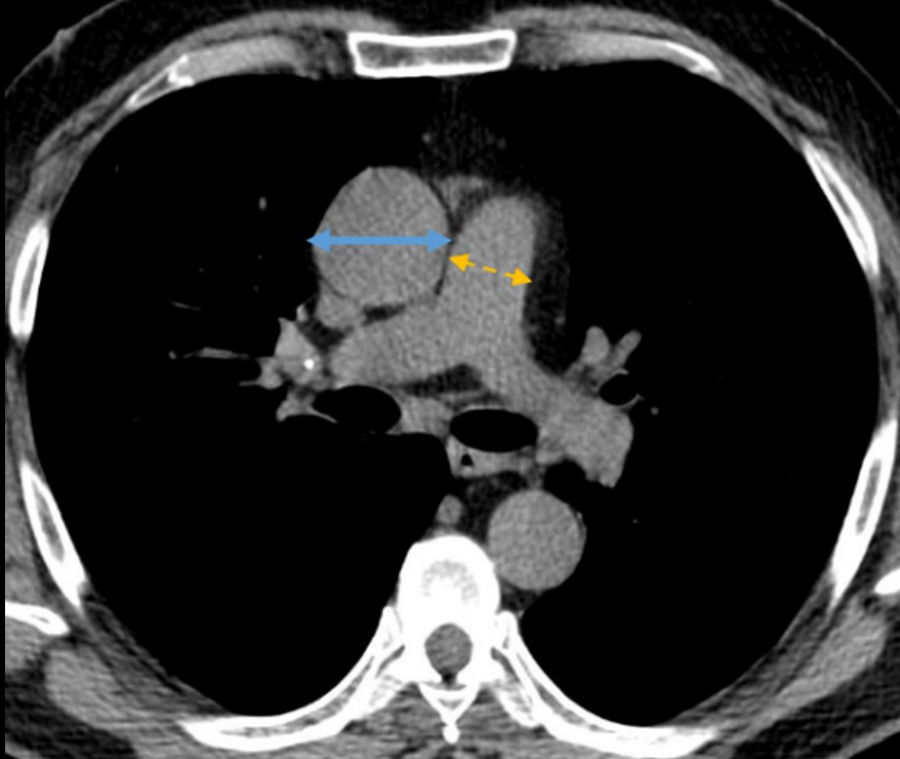
Cystic fibrosis (CF) is an inherited multi-system disease associated with chronic respiratory infections. As the disease worsens, patients develop progressive respiratory failure, pulmonary hypertension and eventually, right ventricular dysfunction. Although the gold standard for diagnosis of pulmonary vascular disease is right heart catheterization, non-invasive techniques, specifically computed tomography (CT), are increasingly being used as diagnostic tools.1 Pulmonary artery enlargement characterized by an increased ratio between pulmonary artery and ascending aorta diameter (PA:A) ratio>1 is a robust indicator of pulmonary hypertension2 (Fig. 1). There are few studies about the paper of vascular alterations and CF. Wells et al.3 demonstrated that pulmonary artery enlargement is prevalent in adult patients with CF and is associated with acute pulmonary exacerbations. The PA:A ratio could be a predictive marker in CF.
In this study, we want to evaluate temporal changes on pulmonary artery size on CT and to assess whether an increase of pulmonary artery in consecutive CT studies could be a factor of worse prognosis.
An ambispective longitudinal study was conducted from 2007 to 2018, retrospective phase 2007–2017 and prospective phase 2017–2018, enrolling adult patients from a cystic fibrosis unit. Inclusion criteria were: CF patients over 18 years, with at least two consecutive thoracic routine CT valid for diagnosis, with respiratory function test at the time of CT. Exclusion criteria were: having only one CT, or an acute exacerbation during the 4 weeks prior to the procedure. The institutional ethics review board approved the study (number 3424). The PA:A ratio was calculated for all the CT studies, and separated in two groups: PA:A ratio≤1 (normal) or PA:A>1 (enlarged) and was correlated with: annual FEV1% change, annual exacerbations and oral and intravenous antibiotic cycles, haemoptysis, lung transplantation and exitus. Of the eighty three patients seen in the cystic fibrosis unit at the study time period, sixty four patients (33 males and 31 females) met the inclusion criteria, median age of 26.84 (SD 7.92) years old. Demographic, clinical, spirometry and PA:A characteristics of the study cohort are shown in Table 1. The median interval between the two CT studies was 3.88±1.59 years. The mean spirometric values of the patients showed dynamic lung volumes lower than the general population, both in absolute values or as percentages of the reference values. There was a worsening of respiratory function. The PA:A ratio mean at the first CT time was 0.90 and at the last CT time was 0.92. Most patients, 56 patients (87%) at the first CT and 54 patients (84%) at the last CT, presented a PA:A≤1 (normal); and 8 patients (13%) at the first CT and 10 patients (16%) at the last CT had PA:A>1 (enlarged). We found a low correlation between pulmonary artery enlargement and exitus (r was 0.008, p<0.005). No statistically significant relationship was found for exacerbations and other clinical variables.
Clinical and demographic characteristics of the study population.
| Variables | n=64 |
|---|---|
| Demographics | |
| Age at first CT, years | 26.84±7.92 |
| Sex (male/female) number of patients (%) | 33 (51.64)/31 (48.44) |
| BMI, kg/m2, mean, SD | 22.53±3.03 |
| Genotype, number of patients (%) | |
| Phe508del homozygous | 21 (32.81) |
| Phe508del heterozygous | 26 (40.63) |
| Others | 17 (26.56) |
| Presence of co-morbidities, number of patients (%) | |
| Pancreatic insufficient | 43 (67.19) |
| Hemoptysis | 10 (15.63) |
| Lung transplantation | 6 (9.38) |
| Exitus | 1 (1.56) |
| Annual exacerbations mean, SD | 2.88 |
| Annual oral antibiotic treatments mean, SD | 2.41 |
| Annual intravenous antibiotic treatments mean, SD | 0.33 |
| Spirometric variables, % predicted, mean, SD | |
| FEV1 at first CT time | 71.78 (19.39) |
| FEV1 at last CT time | 66.74 (19.94) |
| FEV1 annual change | −1.30 (2.66) |
| PA:A ratio | |
| At first CT time | 56 (87%) |
| ≤1 (normal), number of patients (%) | 8 (13%) |
| >1 (enlarged), number of patients (%) | |
| At last CT time | |
| ≤1 (normal), number of patients (%) | 54 (84%) |
| >1 (enlarged), number of patients (%) | 10 (16%) |
| At first CT time, mean | 0.90 |
| At last CT time, mean | 0.92 |
CT: computed tomography, SD: standard deviation, BMI: body mass index, CFTR: cystic fibrosis transmembrane regulator, MRSA: methicillin resistant Staphylococcus aureus, FEV1: forced expiratory volume in one second, PA: pulmonary artery, A: aorta.
In the progression of lung diseases such as CF, pulmonary hypertension can develop. Tonelli A. et al.4 described an incidence of pulmonary hypertension on more than half of the patients in 57 adults with advanced stage CF. Hayes et al.5 found in patients with CF who were candidates for lung transplantation that the presence of pulmonary hypertension was associated with an increased risk of death. The reference test for the diagnosis of pulmonary hypertension is the measurement in the pulmonary artery greater than or equal to 25mmHg by right hearth catheterization. Increased diameter of the pulmonary artery on CT is an indicator of hypertension.1 The association has been especially studied in older patients with non-cystic fibrosis bronchiectasis.6 Respiratory exacerbations in CF are associated with progression of lung deterioration and increased mortality. The role of pulmonary vascular disease in exacerbations is not exactly known. In 2016, Wells J. et al.3 correlated pulmonary artery enlargement in CF and the risk of exacerbations. They referred two cohorts of adult patients with the disease, the first cohort was followed for one year and the second for two years. They found that approximately half of the patients in each cohort had a PA:A ratio greater than one and proved that in this group of patients they had more exacerbations. In our cohort, only 13% of our patients at the first CT and 16% at the last CT had a PA:A ratio greater than one. One explanation may be that our group were young patients, but surprisingly, Wells's work found that patients with an enlarged pulmonary artery were younger than those without. In our study, we also demonstrate a slight enlargement of the pulmonary artery between the first and the second tomography. One limitation of the study could be the mean following period was only 3.88 years, longer period could give us more information. There was a relationship between pulmonary artery enlargement and death, although in our series there was only one death, and this result should be evaluated with caution; future studies analyzing other variables could be interesting. On the contrary other studies, we did not find correlation between pulmonary artery enlargement and exacerbations. No correlation appeared between the evolution of pulmonary artery enlargement and worsening of respiratory function, lung transplantation, or hemoptysis.
In conclusion, in our study we found a slight enlargement of pulmonary artery over time on consecutive CT exams and a low relation between a pulmonary artery/aorta ratio>1 and exitus. No statistically significant relationship was found for exacerbations and other clinical variables.
Informed consentThe authors confirm that written consent has been obtained from all patients.
FundingThe authors state that this work has not received any funding.
Conflict of interestThe authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.